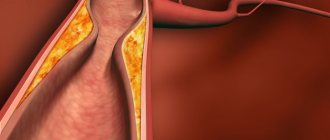
Hyphema in ophthalmology is a pathological condition of the eyes that occurs due to hemorrhage in the anterior chamber of the eyes. Often the iris that bleeds is the one whose tissue is characterized by a large number of blood vessels. It is impossible to say about the exact volume of blood.
Sometimes a thin strip appears, which can only be seen under a microscope, and in some cases a spot forms in the area of the eyeball.
This area is limited on the outside by the cornea, and on the back by the membrane and lens. The blood is always in the lower part, since it is heavier than the eye fluid.
People over 40 years of age, as well as those who have injured their visual organs, are more susceptible to the development of hyphema (that is, the disorder can be diagnosed in any person, even a child). The peculiarity of the disease is its severe course and the high probability of relapse. If proper treatment is not started on time, the person will become completely blind. Reference! The code for hyphema in the international classification ICD-10 is H21.0.
Symptoms
There are 4 degrees of severity of hyphema:
- 1st degree – the anterior chamber is blocked by blood by 1/3:
- 2nd degree – the volume is filled with blood from 1/3 to half;
- 3 degree – more than 1/2;
- Grade 4 – the anterior chamber is completely filled with blood.
Depending on the severity, symptoms will vary. As a rule, patients present the following complaints:
- general eye soreness;
- sensitivity to bright light;
- blurred vision, “veil” before the eyes;
- neurological symptoms: dizziness, headaches.
If these signs appear, you should contact an ophthalmologist.
Hemorrhage into the anterior chamber of the eye (hyphema)
The anterior chamber of the eye is the area between the cornea (the clear, convex “lens” of the eye) and the iris (the disk with the pupil in the center that gives our eyes their unique color) and the lens (the clear lens behind the pupil). Normally, this area is filled with an absolutely transparent liquid - the moisture of the anterior chamber; the appearance of blood is called hyphema or hemorrhage into the anterior chamber of the eye.
The causes of hyphema, although they seem completely unrelated, carry at their core the same element - rupture of the vessel. They are conventionally divided into three groups:
- Trauma is the most common cause of hyphema.
- trauma can be penetrating - damage to the eye is accompanied by communication between the internal contents of the eyeball and the environment; such trauma often occurs from the action of sharp objects, less often from the action of blunt objects;
- the injury is not penetrating - while the external integrity of the eye, its internal structures are destroyed, which leads to the outflow of blood into the anterior chamber of the eye; such injury is almost always a consequence of the action of blunt objects;
- The group of injuries also includes all types of operations on the organs of vision, which may be accompanied by hyphema.
- Diseases of the eyeball
associated with the formation of new, defective vessels inside the eye (neovascularization). Newly formed vessels have structural defects that cause their increased fragility, which is associated with the outpouring of blood into the anterior chamber of the eye with little or no impact. Such diseases include:
- diabetic angiopathy (a consequence of diabetes mellitus);
- retinal vein blockage;
- retinal disinsertion;
- intraocular tumors;
- inflammatory diseases of the internal structures of the eye.
- Diseases of the body as a whole:
- chronic alcohol and drug intoxication;
- blood clotting disorder;
- oncological diseases;
- systemic connective tissue diseases.
degree of hyphema
Hyphema, based on the level of blood in the upright position of the patient, is divided into four grades:
- The 1st visually anterior chamber of the eye is occupied by blood by no more than a third;
- 2nd blood fills the anterior chamber of the eye to no more than half;
- The 3rd chamber is filled with blood by more than ½, but not completely;
- 4th total filling of the anterior chamber of the eye with blood “black eye”.
Despite the obvious conventionality of this division, it is of practical importance for the choice of treatment tactics and prognosis of the outcome of hemorrhage. The degree of hyphema is also determined by its symptoms and their severity:
- Visually detectable presence of blood in the anterior chamber of the eye;
- Decrease in visual acuity, especially in a lying position, to the point that only the sense of light is preserved and no more (at 3-4 degrees);
- Blurred vision in the affected eye;
- Fear of bright light (photophobia);
- Sometimes there is a feeling of pain.
The diagnosis of hemorrhage in the anterior chamber of the eye at a doctor’s appointment usually does not cause any significant difficulties and is based on technically simple manipulations:
- Visual inspection;
- Tonometry – measurement of intraocular pressure;
- Visometry – establishing visual acuity;
- Biomicroscopy is an instrumental method using a special ophthalmological microscope.
manifestations of hemorrhage in the anterior chamber of the eye
Treatment of hyphema is always associated with the elimination of the pathology that caused it - the abolition of blood-thinning drugs, the fight against inflammatory diseases of the eye, giving up bad habits, maintaining the elasticity of the vascular wall, etc. Almost always, small amounts of blood in the cavity behind the cornea resolve on their own with the use of a 3% solution of potassium iodide and blood-lowering drugs.
Surgical treatment is performed in case of complicated hyphema; indications for surgery are:
- There is no effect from the use of drugs (the blood does not resolve) within 10 days;
- The blood has lost its fluidity - a clot has formed;
- The cornea began to stain with blood;
- Intraocular pressure does not decrease during treatment.
If the operation is refused, serious complications such as glaucoma may develop, as well as a significant drop in visual acuity due to a decrease in the transparency of the blood-stained cornea.
Video: what does hemorrhage in the anterior chamber of the eye look like?
Degrees and types
In accordance with the amount of collected blood, doctors distinguish 3 degrees of hyphema of the visual organ:
- The blood level does not exaggerate 2 mm. There are blood smears on the iris.
- The degree of blood ranges from 2–5 mm.
- Total hyphema.
If there are no noticeable changes, ophthalmologists talk about the presence of microhyphema, which can only be seen under a microscope.
Blood accumulations can form in the anterior chamber, retina, and vitreous body. When hemorrhage occurred in the first variant, a uniform formation of a scarlet hue appears. In a lying position, the liquid spreads over the surface. When standing, blood settles at the bottom of the eyeball.
Bleeding that occurs in the retina of the eye is almost invisible. And this does not depend on the degree of damage. Patients are tormented by a disorder of clear vision, the formation of floaters over the visual organ. Excessive bleeding can lead to blindness.
Hemorrhages in the orbit occur due to injury, blood pathologies, and vasculitis. Patients experience bulging of the eyes, decreased visibility of the conjunctiva, difficulty in motor activity, and blood draining under the skin of the eyelids.
The formation of blood (hemophthalmos) in the area of the vitreous body implies a brown accumulation behind the lens. Expressed in the form of flashes of light, darkened spots. Total impairment causes complete blindness.
Causes
The most common cause of hyphema formation is mechanical trauma to the eyeball, especially penetrating wounds. Hemorrhage occurs due to damage to the integrity of the blood vessels. If the injury was non-penetrating, it could provoke a sharp rise in intraocular pressure, which also damages the blood vessels. Also reasons are:
- inflammatory ophthalmological diseases: inflammation of the choroid, iris, ciliary body;
- retinal detachment.
Patients with diabetes are at risk. Provoking factors are autoimmune diseases, problems with blood clotting, and cancer.
Reasons for development
Experts talk about four main factors leading to the occurrence of a violation:
- Traumatic hyphema - the most popular cause of development is mechanical in nature. A through puncture, in which all eye membranes are injured, leads to rupture of blood vessels, from which blood spills into the anterior wall. But with blunt trauma, hemorrhage occurs due to a sharp drop in eye pressure, which provokes rupture of blood vessels in the membrane of the visual organ. This most often occurs with concussions and wounds.
- Hyphema of the eye after surgery , for example, cataract removal - when performing laser or strip depilation, the plexus of blood vessels (ciliary body or iris) is sometimes damaged. If hemorrhages occur during the rehabilitation period, this is due to a blood clot and unstable geodynamics.
- Diseases of the organs of vision . Some pathological processes in the eyes can lead to the fact that new vessels grow greatly and at the same time have thin walls. Because of this, the walls break even with slight vibrations.
- General systemic diseases of the body . Diseases that are accompanied by blood clotting disorders also lead to hemorrhage in the organs of vision. In addition, it is worth noting that frequent consumption of alcoholic beverages and drugs provokes disruptions in the process of blood clotting and fragility of blood vessels. All this contributes to the development of hyphema.
What could be the reason?
Hyphema of the eye can form due to the following reasons:
Why does the inside of my eye hurt?
- injury. We are talking about both a penetrating wound and a blunt wound;
- ophthalmological operations. The greatest danger is posed by hemorrhages that developed during the first few days after surgery;
- physical exercise. Hemorrhage can occur in pregnant women during pushing, as well as with strong screaming;
- tumor process. The neoplasm compresses and damages blood vessels;
- eye diseases. Diabetes mellitus at the stage of decompensation, thrombosis of the central retinal vein, neoplasms - all these pathologies can cause the development of new blood vessels with thin walls. But when there is a difference in arterial or intraocular pressure, these vessels burst, which leads to hemorrhage. Myopia and retinal angiopathy can also cause hyphema;
- diseases of the coagulation system: hemophilia, leukemia, anemia;
- circulatory diseases: atherosclerosis, microaneurysms, stenosis of vessel walls, arterial hypertension.
Trauma is a common cause of hyphema.
Separately, I would like to say about eye contusion. According to statistics, it is blunt trauma to the eye that causes hyphema. Experts distinguish three degrees of severity of concussion:
- Easy. No visible damage to the eye tissue was detected. Functional disorders are reversible.
- Average. Slight damage to eye structures is typical. Vision drops to light perception.
- Heavy. Disturbances in the structures of the eye are irreversible. There is cosmetic death of the eyeball and complete loss of vision.
Diagnostics
To identify hyphema, a comprehensive diagnosis is necessary. Upon examination and questioning of the patient, it usually turns out that there is a history of trauma or that an ophthalmic operation has recently been undergone.
Before treatment you must:
- biomicroscopy using a three-mirror Goldmann lens. The doctor examines the conjunctiva, lens and vitreous body. The main object for study remains the anterior chamber. The procedure is painless for the patient; first, drops must be dropped into the eyes to dilate the pupil;
- gonioscopy – examination of the anterior chamber with visualization of inflammatory and degenerative changes. The procedure is non-invasive. Gonioscopy cannot be performed for conjunctivitis or keratitis. To avoid infection in the eye, the doctor must thoroughly clean the goniolens;
- ultrasound scanning. A highly informative and sensitive method that allows you to reproduce a two-dimensional image. Helps to identify the inflammatory focus and determine how extensive it is.
You also need to do visometry - a visual acuity test. It will help you understand how much visual acuity has decreased due to the hyphema; for this, it is enough to use a standard letter table. To monitor intraocular pressure, tonometry is performed using a contact or non-contact method.
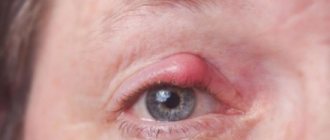
Symptoms of the disease
Symptoms depend on the degree of damage to the eye. The first stage of hyphema can be virtually asymptomatic and is often diagnosed during a scheduled examination by a doctor. The second degree begins with deterioration of the patient’s vision and photophobia.
At this time, hemorrhage is detectable with the naked eye. At the next stage, the symptoms are pronounced, the patient notes a decrease in vision, feels pain and discomfort in the eye area, and external signs of hyphema are clearly visible. The fourth stage is characterized by significant pain and loss of vision (a person can only distinguish light).
General symptoms of hyphema include the following manifestations:
- The affected eye hurts
- Surrounding objects become foggy, visual ability gradually decreases
- Bright light is painful
- “Floaters” appear before the eyes
- Sick man suffering from dizziness
Treatment of hyphema
For grades 1 and 2 of disease severity, drug treatment is indicated. To do this, use eye drops containing corticosteroids and mydriatics - agents that dilate the pupil. Together, these substances not only effectively eliminate the problem, but also prevent relapses.
Read in a separate article: Hemangioma of the eye: what is it, treatment in adults and children
If hyphema is combined with increased intraocular pressure, anti-glaucoma drops are also used: Betaxolol, Pilocarpine, Travatan.
Surgical treatment is prescribed if medication does not have an effect, or the disease has progressed to stage 3 or 4. Trabectulectomy is used. It helps improve blood flow and normalizes intraocular pressure.
The operation is performed using anesthesia, the surgeon makes an incision on the conjunctiva, separates the fibrous plate and makes an incision on the tunica albuginea. Next, a path is formed for the outflow of intraocular fluid. To prevent the formation of a postoperative wound, antitumor antibiotics are used. Sutures are placed on the conjunctiva.
After the intervention, it is necessary to instill antibacterial drops and corticosteroids into the eyes for 4 weeks, and mydriatics will also be needed. It is necessary to keep the level of intraocular pressure under control; it is measured using non-contact tonometry. If the pressure rises, which is natural for the postoperative period, it is reduced with medication.
You need to remain in bed for several days after the operation, but in most cases a hospital stay is not required; the patient can undergo examinations on an outpatient basis.
A decisive examination of the anterior chamber of the eyeball, from which it can be concluded that the patient is healthy, can be carried out no earlier than 3 weeks after the operation.
Treatment methods
In most cases, hyphemas are subject to outpatient treatment with mandatory ophthalmological monitoring on the second and fifth days from the moment of initial treatment. Children under three years of age, patients with extremely high intraocular pressure (if drug treatment is ineffective), as well as patients with a history of increased oncohematological suspicion and grade 3-4 hemorrhages are hospitalized in the hospital.
For several days, the patient must observe strict bed rest, limiting as much as possible (preferably completely eliminating) any physical activity. The affected eye should be covered with a sterile bandage made of soft material during the day - this will help protect the injured areas from secondary damage and reduce pain caused by a pathological reaction to bright light sources. The dressing is also necessary to prevent infection, since injured tissues have increased permeability against the background of decreased specific resistance to various pathogens.
The head of the bed should be raised by 45-50°C.
Drug therapy
For uncomplicated hyphemas of grade 1-2, treatment includes the use of topical drugs (in the form of eye drops) of the following pharmacological groups:
- Glucocorticosteroid groups (prednisolone). Hormone therapy is the basis for the treatment of any intraconjunctival hemorrhages, since these drugs block the processes of dissolution of blood clots and blood clots and have a pronounced anti-inflammatory effect, alleviating the symptomatic course of the disease.
- Hemostatic agents (aminocaproic acid). Aminocaproic acid inhibits the conversion of profibrinolysin to fibrinolysin. It is used systemically in the form of tablets or injections.
- Mydriatics (atropine). Mydriatic eye drops are used to dilate pupils, reduce painful reactions to bright light sources, reduce the risk of developing “false myopia” syndrome and prevent adhesions in the anterior chamber of the eye.
- Antiglaucoma drugs that reduce the secretion of tear fluid (dorzolamide). Used orally in the form of tablets, they are indicated to reduce intraocular pressure.
Glucocorticosteroid drug Auropred
Note! Antiglaucoma drugs are not prescribed to patients who have hyphema due to sickle cell anemia due to the high risk of deformation of red blood cells and further blocking of the pathways for excretion of intraocular fluid, which, in turn, will provoke a re-increase in ophthalmotonus.
Magnetophoresis
Magnetophoresis is a procedure in which a therapeutic effect is achieved through the influence of a magnetic field on damaged eye tissue. First, a subconjunctival injection of hypersmolar saline solution with a salt concentration of 5-10% is performed, after which an alternating magnetic field inductor is applied to the closed eyelids. The duration of the procedure is about 10 minutes.
Resorption of blood and blood clots after magnetophoresis occurs on days 3-5 (with grade 1 microhyphema) or on days 5-7 - with grade 2 hyphema. For grade 3-4 lesions, physiotherapeutic methods, as well as drug treatment, are ineffective.
Magnetophoresis can also be used for faster healing and tissue restoration after surgical treatment of hyphema and glaucoma.
Magnetophoresis
Trabeculectomy of the anterior chamber of the eye
This operation involves the drainage of hemorrhagic fluid and moisture from the anterior chamber of the eye under the conjunctiva, where it is further absorbed. Such manipulations are a common method of treating glaucoma and are used to remove grade 3-4 hyphemas, for which drug therapy is ineffective and impractical.
To perform the manipulations, the doctor may use local anesthesia with mild sedation or more aggressive techniques, such as bulbar or conduction block.
The algorithm of actions for trabeculectomy is usually as follows:
- Local anesthesia using the most appropriate methods to maintain the possibility of interaction between the patient and the doctor.
- Performing two micropunctures parallel to each other.
- Injection of a crystalloid solution for lavage through one of the paracenteses.
- Removal of hemorrhagic fluid and formed blood clots through the second puncture.
Every 2 hours after surgery, it is necessary to instill anti-inflammatory drugs (prednisolone) and antibiotics into the eye (up to 4 times a day). To relieve pain, analgesics or drugs from the NSAID group are used. If a pain attack does not go away even with the use of painkillers, you should seek emergency medical help.
After surgery, the eye is covered with a sterile gauze bandage.
What is hyphema
When the disease occurs, blood and clots collect in the anterior chamber of the eye. The larger the congestion there, the worse the visual visibility. When the chamber is completely filled, vision is completely lost. This appears due to injuries, rupture of recently formed vessels, or due to the presence of hematological diseases.
Hyphema caused by injury is most often observed in men. And other causes of the disease are noted in the same proportion. Patients over 40 years of age have an increased risk of developing hyphema. In infants, the disease can appear due to shaking or congenital blood diseases.
The pathology is associated with a complex course; without appropriate treatment there will be progression. Lack of therapeutic action will lead to complete loss of vision. In 35% of cases, a relapse occurs on day 3.
Hyphema in cats and dogs
Hyphema is diagnosed more often in cats than in dogs. The main reason why this disease develops in animals is trauma (bruise, contusion, penetrating wound) of the eye. Especially in young active dogs and cats, due to fights, after being wounded by a claw, blood vessels inside the eye rupture and blood enters the anterior chamber.
In adult animals, hyphema can develop against the background of high blood pressure due to renal failure. In addition, uveitis (inflammation of the middle membrane of the eye, rich in blood vessels) or retinitis (inflammation of the iris) can provoke the disease.
Hyphema in an animal can be detected by careful examination - bloody clots will be observed in the intraocular fluid. However, only a veterinarian can make a correct diagnosis based on a set of studies (ophthalmoscopy, ultrasound, biomicroscopy, tonometry). In addition, to check the somatic condition of the pet, blood is given for analysis.
Since hyphema is a consequence of the underlying disease, therapy is aimed at treating a specific pathology. Therefore, in each individual case, a different set of drugs is used.
Prevention
There are no special preventive measures that can guarantee the prevention of hyphema, but the following recommendations should be taken into account:
- if the patient has blood diseases, he should undergo regular tests and keep hematological parameters under control;
- for diabetes mellitus type 1, 2 and arterial hypertension, it is necessary to be examined by an ophthalmologist 2 times a year;
- for malignant tumors of the eyeball, consultation with an ophthalmo-oncologist is necessary every 3 months.
Eyes should be protected from mechanical damage; when performing traumatic work, safety glasses should be worn.
With timely treatment of hyphema, the prognosis for life is favorable, the patient remains able to work.
If, due to the advanced state of the disease, visual function has been seriously affected, a disability may be issued by decision of a special commission.
Details of the causes of occurrence
But hyphema is not only injuries, blood diseases, or the result of not entirely adequate treatment. Rupture of microcapillaries in the eye due to insomnia and chronic fatigue is also a hyphema.
Therefore, we present a list of all possible causes of this disease, excluding traumatic ones, with which everything is already clear.
- Lack of sleep. Chronic fatigue and a general drop in tone can cause lack of sleep. Professional and everyday troubles also do not contribute to vascular health.
- Physical exhaustion. Fatigue is a consequence of the accumulation of lactic acid in the body. Neutralized by deep, long physiological sleep.
- Birth trauma of the capillaries, naturally inherent in women.
- For diabetes mellitus. The elasticity of the walls of blood vessels, including the smallest ones, is impaired. With this disease, a strong, persistent thirst is added to the regular redness of the whites of the eyes. Other symptoms include weight gain, itchy skin, and frequent urination.
- Hypertension. Increases and even surges in blood pressure inevitably cause a concomitant increase in the pressure of the intraocular fluid. Another companion of high blood pressure is nosebleeds.
- ARVI infections. Rhinitis can be a provoking factor during ARVI. When you try to blow your nose, massive damage to blood vessels can occur. The capillaries of the eye and even the larger vessels of the sclera are no exception.
Treatment of the disease
The pathology is eliminated by using Atropine. In the early stages of the development of the disease, conservative therapy is used with the help of Prednisolone and Atropine. Corticosteroid drugs stop repeated relapses of hyphema. If a patient has been diagnosed with increased eye pressure, carbonic anhydrase inhibitors are prescribed. Treatment with surgical intervention is recommended at stages 3-4 of the disease. As a result of two parallel punctures, a crystalloid solution is injected into the eye cavity and the accumulated clots are washed out. Trabeculectomy improves fluid outflow and lowers IOP. The disease is treated on an outpatient basis. Only patients with high intraocular pressure, pathological diseases of the hematopoietic system, and children under 3 years of age are recommended to be hospitalized.
Alternative medicine
Traditional methods can be used as an auxiliary therapy. A decoction of chicory will help eliminate the manifestations of hemorrhage. To prepare, you need to take 3 large spoons of the plant root, add 0.5 liters of water, let it boil, and leave for 15 minutes. It is recommended to strain the resulting liquid through cheesecloth. Drink ½ cup 3 times a day, or make compresses based on the resulting decoction.
With microhyphema, there is no need to treat the disease; the blood in the eye cavity can resolve spontaneously. People who have been diagnosed with hyphema should be seen by an ophthalmologist.
Treatment of the disease
The ophthalmologist prescribes treatment after determining the degree of hyphema. In the initial stage, conservative therapy is chosen, and if there is significant hemorrhage, the patient is operated on. Most procedures are performed in an outpatient clinic; children and patients with hemoglobinopathy or serious complications are treated in the hospital.
Recommendations for patients
The treatment prescribed varies, but there are general tips:
- Need to rest and stay in bed
- You need to sleep with a high headboard, raising the top of a hospital bed or placing several pillows at home (the angle should be about 50–60 ̊)
- You can’t bend over, you need to avoid physical activity for a while
- If you need pain medications, consult your doctor. Most of these medications alter blood clotting rates, so refrain from self-administering medications
- If your doctor has advised you to wear a bandage, you should not ignore his recommendation.
Therapy with medications
To treat hyphema, drugs of different effects are prescribed, they are widely used and produce a good effect:
- Medicines to strengthen the walls of blood vessels (Emoprox, Diclofenac, Actovegin, Taufon, Okovit)
- Painkillers (Tylenol, Acetaminophen, Aldolor, etc.)
- Mydriatics to prevent adhesions near the lens and iris (Atropine 1%)
- Medicines to stop bleeding (Purolase, Aminocaproic acid, etc.)
- Medicines with absorbable action (Glycerol, Mannitol, Mannitol, etc.)
- Means for normalizing IOP (Diacarb, Timol, etc.)
Corticosteroid drops
The basis of treatment is corticosteroids, which reduce the likelihood of recurrent hemorrhage (numerous studies indicate a decrease in rates from 12% to 5% of cases). With the help of drops with corticosteroids, inflammation and pain are eliminated.
| The optimal dose and duration of use of these drugs is determined by the doctor for each patient. |
Surgical intervention
The operation is envisaged for the third and fourth degrees of hyphema. The anterior chamber of the affected eye is carefully washed. To do this, the surgeon makes two incisions: a special solution is poured through one, and liquid with blood clots is pumped out of the second. If IOP is high, trabeculectomy is performed, with the help of which blood flow is activated and the pressure is normalized. Indications for surgery are:
- Staining the cornea red
- Formation of blood clots
- Increased IOP
- Lack of expected results after drug treatment
- Third and fourth degrees of pathology
Return to contents
Treatment prognosis
In mild cases, it takes several days to a week for the hyphema to completely resolve. But approximately 1/5 of the patients experience more intense bleeding within 3-5 days, so it is very important to consult a doctor and follow his recommendations exactly.
In general, the prognosis regarding the restoration of previous visual acuity may be different, since this is influenced by many factors, especially the volume of blood shed and the value of intraocular pressure. If the latter remains within normal limits and there is no other damage to the structures of the eye, vision is usually completely restored after a few weeks.
Possible complications and consequences
Timely methods of therapy prevent complications, but if the patient did not pay attention to the problem at first, the situation worsens:
- Repeated bleeding occurs, which is always more intense
- As a result of the formation of blood clots and with significant filling of the eye chamber, an increase in IOP occurs, causing secondary glaucoma
- The optic nerve atrophies
- Synechiae are formed
- In some cases, Schlemm's canal narrows or becomes completely blocked.
Secondary glaucoma cannot be cured, and complications lead to blindness, so it is important to see a doctor as soon as symptoms appear.