It would seem that in the first posts I explained why this is so. But the comments to the post show that this was not enough. So let's do everything according to the rules of scientific discussion. Let's analyze the theses and bring relevant research to them.
This is exactly what they do in the scientific and medical world. If you have an opinion, you need to justify it. Preferably, on a sample of 20 or more patients with the same distribution in a double study. It is desirable that the studies be confirmed by different clinics in different countries where these types of operations are performed.
Let's start.
Defining the terms
SMILE
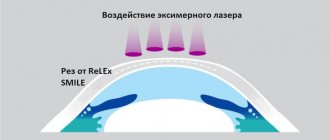
(ReLEx SMILE or simply SMILE) born in 2007 - Small incision lenticular extraction - 100% femtosecond technology. The prefix Femto- means that the laser has a very short pulse: 1015 pulses fit in every second. In this case, the coherence and power of the output beam is maximum. With its help, a three-dimensional “figure” is cut out in the form of an individual lens - a lenticule inside the cornea and removed through a small entrance (1.5 - 4 mm). The “figure” is microinvasively removed from the inner layer of the cornea - nothing is evaporated, and the cornea takes on a new shape. Here are the details. Here is the principle of the operation, and here is the operation itself. Within the SMILE EYES holding - 0.5% on enchancment (additional correction), worldwide - up to 2%.
This is how ReLEx SMILE FLEX,
born in 2005, is performed - the predecessor of the SMILE method, also 100% femtosecond technology. Now it is fashionable to sell it as “pseudo-SMILE”. The difference is that, like SMILE, a custom lens is cut into the cornea, but a flap cap is cut around the circumference to remove it. That is, there is no heating and evaporation - this is a plus, but otherwise - it’s the same opening of the “lid”. It is done under one laser, no excimer is needed. Does not provide the patient with significant advantages over femtoLASIK. The equipment manufacturer offers it as part of the surgeon’s preparation for the SMILE method.
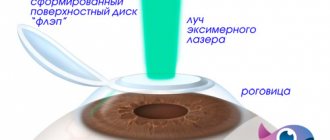
femtoLASIK
(FS-LASIK, femtosecond LASIK) born in 2000 - a method using two lasers: a femtolaser and an excimer laser.
A femtolaser is used to form a “lid” in the cornea, then the lid is manually folded back. An excimer laser is needed to evaporate the lens in the middle layers of the cornea. There is a thermal effect. The operation depends on the quality of each of the two lasers (older models of both together can spoil the overall result). Then the lid is put back in its original place. It never grows, you can always raise it. The purpose of the operation is not to burn the upper layers of the cornea, which are the strongest and contain the largest number of nerve endings. Now this is one of the most common operations in Russia and in the world. Inside the holding it is only about 5-10% of the entire myopia correction. Statistics on additional correction in the world are 8-12%.
The term "SUPER LASIK"
– not a separate method – used as a characteristic of the evaporation profile with an excimer laser – an individual evaporation profile in the cornea is implied. That is, it can be both “SUPER-femtoLASIK” and “SUPER-simple-LASIK”. In scientific medical publications, the term “Super Lasik” (precisely with the prefix “Super”) is not used and is not an official medical term. It has gained some popularity in the advertising of some medical clinics, apparently wanting to attract additional attention due to “bright terminology.”
LASIK
(Laser-Assisted in Situ Keratomileusis) – born in 1989 – surgical separation of the flap cap using a microkeratome device, a special machine with a “shaving” blade and subsequent excimer laser evaporation of the lens on the cornea. To evaporate a lens in the middle layers of the cornea, you need one laser - an excimer and a mechanical microkeratome device. LASIK is a combination of mechanical and laser effects. The result depends on the quality of the laser and the quality of the microkeratome. There is a thermal effect.
All its varieties are also obsolete: the Epi-LASIK
- an attempt to reduce the thickness of the corneal slice - indicates that the cut is made on the very surface of the cornea and the
REIK
- “horseradish is not sweeter than radish” - this is the same LASIK. By the way, a thin flap “wrinkles” more and “flies” more easily when injured. The flap also becomes the “culprit” of additional optical aberrations that affect the postoperative quality of vision.
In our clinic today, the microkeratome is “covered” as an exhibition exhibit; for modern surgical practice, this is already barbaric. It is extremely rarely needed, for example, to cut through scars.
LASIK/femtoLASIK
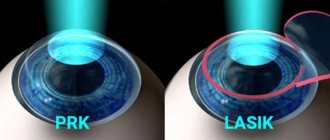
PRK
(Photorefractive keratectomy, PRK) - born in 1985 - a method of evaporating a lens in the upper layers of the corneal stroma without creating a flap with preliminary removal of the surface layer of the epithelium. The oldest method of all laser correction methods.
Complications have been well studied, the largest statistics on them is up to 15%. Within 1-1.5 diopters of correction it performs well, but with higher myopia all the shortcomings creep out. Due to difficult healing, large wound surface and risks, it can only be recommended for economic reasons.
Of the minuses, a huge (πR2 is the area of a circle!) surface of the cornea is “evaporated”, it is important that the most durable surface layers are destroyed, the boundary Bowman’s membrane is evaporated, exactly the same amount of tissue is evaporated as with LASIK, scarring is possible with the appearance of persistent opacities - haze.
The cornea of the eye has a layered structure: epithelium, Bowman's membrane, stroma, Descemet's membrane, posterior epithelium (endothelium). A stable refractive effect is achieved only by changing the geometry of the stroma (the main layer of the cornea). Reaching the stroma is a serious problem, so all types of PRK differ in the way they “pass” the first two layers: the epithelium and Bowman’s membrane. The old “classical” method was used to mechanically remove the epithelium - scraping it off the surface. There is an option of chemical exposure with a 20% alcohol solution - and then scrub. Then it will be LASEK
or
epi-LASEK
.
The epithelium can be “burned out” with the same excimer laser - this will be transepithelial PRK
or
Trans-PRK
. In foreign publications it is found under the designations "ASA", "ASLA", "C-Ten" and "TransPRK". In the early years, trans-PRK was a two-stage procedure; in modern lasers it is a one-stage procedure.
Therefore, it is correct to say that Trans-PRK, an improved technique, but only within the framework of this method, allows us to reduce a number of inevitable shortcomings of the PRK method itself and errors in the results.
But the method itself, alas, cannot be called new.
Although even today there are clinics that sell Trans-PRK as “the most modern method”, and sometimes “the most gentle”.
And PRK is also PRK in Africa, even if he is “Trans”. Marketing geniuses often do this very well! For example, the Estonian procedure eLASIC,
despite the name being similar to another method, is PRK.
This is what PRK looks like
. The only plus is that there is no “lid” and the problems associated with it. Well, one more thing - the surgeon does not need to bother pressing the pedal twice and controlling transitions from one software to another.
The advent of the ReLEx SMILE method almost completely eliminated the need to perform PRK in any variant.
Our PRK technique is used exclusively for medical reasons in cases where correction by other methods is impossible or it is necessary to remove the upper layers of the stroma (for example, if there is opacities).
Here is a comparison of the entire line of methods.
Preparing for surgery
Surgery using the PRK method is a gentle and maximally safe vision correction. However, this is a serious intervention in one of the most important organs, on which the quality of our life directly depends. Therefore, the preparatory preoperative stage should be approached with the utmost seriousness: this will help reduce risks and facilitate rehabilitation.
First of all, you need to undergo a full diagnostic examination, which includes:
- a detailed survey about existing diseases, eye conditions in the past and present;
- determination of the type and degree of refractive error;
- obtaining a map, shape and value of the radius of curvature of the cornea surface, measuring its thickness;
- measurement of intraocular pressure;
- examination of the anterior segment of the eye and fundus.
Diagnostics are carried out in all branches in Yaroslavl, Vologda, Cherepovets and usually take from 1.5 to 2 hours.
After diagnosis, you will be given a list of tests (laboratory blood tests) required to be taken before surgery to rule out any contraindications to laser intervention.
The attending physician will provide you with detailed recommendations and requirements for immediate preparation for the operation. For example, you will need:
- refrain from drinking alcohol for 3 days preceding the procedure;
- do not use decorative cosmetics or perfume on the day of surgery;
- Avoid taking medications as directed by your doctor;
- do not use hard contact lenses for 3 weeks, soft contact lenses for 2 weeks;
- come to the operation in comfortable, fluff-free clothes without a high collar.
SMILE vs PRK according to visual acuity scale
Nethradhama Superspecialty Eye Hospital Study, doi: 10.1155/2017/5646390.
A sample of 120 eyes from 60 patients (34 women, 26 men) undergoing bilateral low myopia correction (up to 4 diopters) with either ReLEx SMILE or PRK. Visual acuity, contrast sensitivity, and higher-order aberrations were recorded preoperatively and compared postoperatively. A comparison was made 3 months after surgery.
Results: At 3 months, the SMILE group showed significantly better visual acuity compared with the PRK group. Postoperative spherical equivalent was comparable in both groups (SMILE = -0.15 ± 0.19 D, FFR = -0.14 ± 0.23 D, p = 0.72). However, SE (sphere equivalent) predictability was better in the SMILE group, with 97% of eyes within ±0.05 D compared with 93% of eyes in the PRK group.
Total higher-order aberrations were significantly higher in the PRK group compared with the SMILE group. The SMILE group showed slightly better contrast sensitivity. Four eyes in the PRK group lost one line of visual acuity due to ocular blur.
Both SMILE and PRK are effective for the correction of low myopia. However, the SMILE procedure offered improved visual quality and better patient satisfaction due to greater postoperative comfort and lower induction of aberrations at 3 months.
My comment:
with the expansion of the sample to 6 diopters, the PRK method would begin to lose numerically more strongly, since it gives a much higher probability of haze and subsequent blurring with increasing cutting depth. The structure of the cornea is restored after a serious PRK burn with scars almost always; they often lie outside the visual area, at the boundaries of the lens evaporation and have little effect on visual acuity. However, this risk is decisive when choosing a medical method for a healthy patient without special indications. Plus, in this study, patients noted a higher subjective quality of life in the SMILE methods, since the postoperative period was painless for them (except for the first day).
By the way, the German refractive community Kommission Refraktive Chirurgie (KRC), as well as the German Association of Ophthalmologists (DOG), prohibits the use of PRK methods to correct myopia with a spherical equivalent greater than -6 diopters. That is, if you have 5.5 and astigmatism more than 1.5, PRK cannot be done! In general, by choosing SMILE you will save your cornea and minimize recovery time.
But let's look at another study. It is more modern, so it was not PRK methods that were compared with SMILE, but the more modern LASIK (transmitting much less energy to the eye and to the middle parts of the stroma, and not to the frame) and SMILE. Here it is:
Indications for correction
Before prescribing the procedure, the ophthalmologist conducts a complete examination of the patient's vision. It is important to remember that each case is individual and each person has their own characteristics of the anomaly and the structure of the eye as a whole. Excimer laser correction is performed for myopia, farsightedness and astigmatism. The advantage of the MAGEK technique is, first of all, the wide range of initial refractive error. While other techniques involve working with significant limitations, MAGEK offers the opportunity to perform an operation with both minimal and maximum results for examining deviations. Correction is carried out with values from -0.25 to -15.0 diopters for myopia. For farsightedness - +5.0 diopters, for astigmatism - from -0.25 to -6.0 diopters.
Assessment of corneal transparency
Department of Ophthalmology, Philipps University of Marburg, Marburg, Germany, doi: 10.3109/02713683.2015.1107590
58 myopic eyes from 33 patients treated with SMILE were compared with 58 eyes of 33 patients treated with FS-LASIK. All procedures were performed using the VisuMax femtosecond laser and the MEL 80 excimer laser. The outcome was assessed using 3 optically significant concentric radial zones (0-2 mm, 2-6 mm and 0-6 mm) around the corneal apex and at 3 different anatomical corneal layers (front, center and rear).
After SMILE, the total of all corneal layers in a 0-6 mm radial ring did not show significant changes compared to preoperative values. After FS-LASIK, the overall outcome was significantly reduced. At 3 months postoperatively, the results leveled off—there were no statistically significant differences between the two groups across all annular spaces examined.
Let me translate the result: no opacities remain immediately with SMILE, but opacities with femtoLASIK methods almost completely disappear within 3 months.
My comment:
By the way, hazes after PRK are visible decades later, just like traces of scars after keratotomy. They look like this:
Hayes after PRK
Corneal scars after radial keratotomy
It is not yet possible to predict the tendency of the cornea to haze: the effect occurs due to the fact that the outer epithelium of the eye is separated from the embryonic cells of the ectoderm (cornea) by Bowman's membrane. When it is burned out by PRK, a pseudo-Bowman's membrane is visible on histology - this epithelium is in direct contact with the ectoderm cells and a framework begins to form to replace the lost membrane. This frame is not always transparent.
Contraindications
Unfortunately, in some cases such an operation cannot be performed for objective reasons. Obvious contraindications to PRK are:
- acute inflammatory processes of the organs of vision;
- some infectious diseases;
- glaucoma;
- progressive myopia;
- cataract;
- pathological changes in the fundus;
- corneal dystrophy or degeneration;
- pathological processes in the retina;
- a number of endocrine diseases (especially diabetes);
- pregnancy;
- breastfeeding period;
- immunodeficiency states;
- autoimmune diseases;
- age up to 18 years, when eye tissue is still forming.
Bowman's membrane and Hayes - what is the danger of PRK (transFRK)
PRK (transPRK, etc.) is a cheap, practical and well-studied method.
But they moved away from it to femtoLASIK methods, and then to SMILE. Why? Now I will try to explain this in simple words, and then I will show the research. According to its morphology, the cornea, like a pie, consists of 5 layers: epithelium, anterior limiting (Bowman's) membrane, intrinsic substance (stroma), posterior limiting (Descemet's) membrane and endothelium.
At the stage of embryonic development, it is formed from three different types of tissue: the epithelium further develops from the surface ectoderm, the middle layer of stroma from the mesoderm, and the inner layer of the endothelium from the neuroectoderm. As they develop and differentiate, each of these tissues, in order to maintain its structure and specificity, needs isolation, which is achieved through the parallel development of boundary membranes - the endothelium forms Descemet's membrane, and the stroma forms Bowman's membrane.
This is the structure of the cornea.
Normally, the cornea has physiological defects in Bowman's membrane, through which nerve fibers penetrate from the stroma into the epithelium. In a healthy cornea, there are few such holes, and there are certain protective mechanisms. When we evaporate Bowman's membrane during PRK, we disrupt the protective barriers and cause inflammation, the body reacts to this by forming fibrous connective tissue. It is subepithelial and intraepithelial fibrosis that is haze (haze (fleur) - from the English haze - fog). It is the reason for the rather slow achievement of final results when performing photorefractive keratectomy (PRK); this remains one of the main problems of the method. Stabilization of refraction, as a rule, lasts several months and may be accompanied by regression or the appearance of haze.
Poorly treatable, severe opacities are rare. But even transient moderate haze during its existence can reduce uncorrected visual acuity and contrast, which becomes a partial return to preoperative refraction and worsens the quality of life of patients.
Thus, possible clouding of the cornea, slow achievement of the optical effect and pain make PRK (transPRK) one of the most unpopular methods of laser vision correction.
Traditional treatment after PRK involves long-term use of corticosteroids, which reduces the frequency and intensity of haze, and also to a certain extent influence the postoperative dynamics of refraction. However, in some cases, corneal opacities in the photoablation zone turn out to be quite persistent and intense, which requires a different approach to treatment. In this case, laser and even surgical methods can be added to drug therapy.
It should be noted that when using PRK as a method of additional correction, the risks are minimal, since the refractive component to be corrected is small. Especially in combination with surface treatment with antimetabolites. But with the initial correction of more than 1-2 diopters, all the disadvantages of PRK appear with all their might.
Here are details about complications.
The nerves are restored, but it takes time. Therefore, after PRK methods, maintenance therapy is needed (up to six months) so that nothing bad happens to the eye during this time. Complete regeneration to a level sufficient for trophic management takes about a year. With the SMILE method, only about 10-15% of nerve endings are cut off, which creates significant differences.
The second feature is the corneal frame. The link contains a description of keratoconus - protrusion of the cornea forward due to intraocular pressure. This is the most common complication, and it is extremely unpleasant. The only way to avoid it is to go deeper into the cornea. The cornea is heterogeneous. The strongest layers are on the surface. At a depth of 120 to 150 microns, loose layers begin. It is there that work is carried out on all methods starting with LASIK. With PRK we remove the strongest part of the upper stroma - see picture above.
I have already said about the specifics that it is better to keep the epithelium and stroma separated. With PRK this is impossible, but with other methods it is possible.
Rehabilitation
After the operation, the patient remains under the supervision of doctors in the hospital of the Medicine 24/7 clinic. She is prescribed antibacterial, anti-inflammatory and painkillers.
Medical procedures and drug therapy at the Medicine 24/7 clinic help reduce the risk of postoperative complications: the formation of adhesions, chronic abdominal pain, urination and defecation disorders, and the development of intestinal obstruction.
To prevent the formation of postoperative cysts, drainage of the retroperitoneal space may be prescribed.
After 7 - 10 days, the sutures are removed. During this time, postoperative pain usually subsides and there is no need for painkillers.
To prevent prolapse of internal organs for 2 months after surgery, it is recommended to wear a bandage, as well as limiting physical activity, avoiding sex, visiting the bathhouse, sauna, and swimming pool.
The first day after surgery, food intake is excluded. Starting from 2–3 days, it is allowed to take liquid fortified nutritional mixtures. After another 2 days, liquid porridges, pureed, light foods are allowed.
After a week, you can switch to a nutritious diet in compliance with the rules of the diet - boiled fish and meat, fermented milk products, pasta and other dietary products.
Aberrations
“Comparison of the visual results after SMILE and femtosecond laser-assisted LASIK for myopia.
Lin F, Xu Y, Yang Y.” Sixty eyes from 31 patients with a mean spherical equivalent of -5.13 ± 1.75 diopters underwent myopia correction using the SMILE procedure. Fifty-one eyes of 27 patients with a mean spherical equivalent of -5.58 ± 2.41 diopters were treated with the FS-LASIK procedure. Results: Neither after 1 nor after 3 months were there any statistically significant differences in visual acuity parameters. High-order aberrations and spherical aberration were significantly lower in the SMILE group than in the FS-LASIK group.
Conclusion: SMILE has a lower induction rate of higher order aberrations and lower spherical aberration than the FS-LASIK procedure.
My comment:
Visual acuity after femtosecond LASIK and after SMILE in quantitative terms was the same in the two groups, but the quality of vision in the group after SMILE was higher due to smaller induced aberrations.
This is due, firstly, to the fact that the SMILE profile itself is aspherical, and the creation of such a profile with an excimer is only possible on modern machines and requires a 5-10% larger volume of corneal evaporation.
Secondly, the optical zone after SMILE is always slightly larger than or equal to the planned one, and with femtosecond LASIK it is slightly smaller than planned.
The damage factor that is significant with femto- and mechanical LASIK + the effect of an excimer laser is completely absent with SMILE.
Comparison of biological indicators of corneal damage
According to the study “Comparison of Corneal Biological Healing After Femtosecond LASIK and Small Incision Lenticule Extraction Procedure” (doi: 10.3928 / 1081597X-20140320-03) on 128 eyes (69 for SMILE, 59 for femtoLASIK).
Tests were done for visual acuity, refraction, Norn test, Schirmer test, corneal sensitivity test, ocular surface index, corneal hysteresis and corneal stability coefficient were measured. Measurements were taken before the operation, on the first day, a week, a month, a quarter and six months after the operation. Result: There was no significant difference in visual outcomes between SMILE and femtoLASIK. After surgery, corneal sensitivity was significantly reduced in the femtoLASIK group and changed slightly in the SMILE group. Early biological corneal healing after SMILE was superior to femtoLASIK. My comment:
In patients after SMILE, dry eye syndrome is significantly less pronounced, corneal sensitivity and strength are preserved with comparable indicators of postoperative visual acuity.
Schirmer test (tear production) and its result
Norn's test (tear film stability)
Now the next study.
How is the operation performed?
Radical removal of the cervix and body of the uterus with uterine appendages is carried out in the operating room of the Medicine 24/7 clinic, equipped in accordance with the highest standards of European and world surgery.
The operation is performed under general anesthesia.
The patient is in a supine position with legs elevated 30–45%. Access can be created by a vertical incision of the abdominal wall bypassing the navel or a horizontal incision with dissection of the rectus abdominis muscles (according to Czerny).
Next, the surgeon cuts the ligaments that support the uterus, separates the bladder, ligates and crosses the feeding blood vessels.
After this, the cervix and body of the uterus, the upper third of the vagina are removed, homeostasis of the vaginal stump is performed, regional lymph nodes, fallopian tubes, and ovaries are excised. It is very important not to damage the ureters.
Wertheim's operation is performed in an open manner, since the doctor must have a clear view of the surgical field so as not to damage the blood vessels and nerves. This minimizes the risk of complications.
After the operation, the incisions are closed with sutures.
The success of the operation depends, first of all, on the qualifications of the surgeon. At the Medicine 24/7 clinic, surgical treatment is performed by doctors who have extensive experience in performing such interventions. This guarantees better results and minimal risk of complications.
We will call you back
Leave your phone number
Biomechanical properties of the human cornea
doi: 10.1007/s10792-017-0575-6
In this pilot study, 11 pairs of human corneas unsuitable for transplantation were divided into two groups. The corneas of the right eye were treated using femtosecond laser LASIK (FSLASIK), the corneas of the left eye were treated using small incision lenticule extraction (SMILE). Pachymetry was measured in each eye immediately before laser refractive surgery. All corneas were refractively corrected with a -10.00 D sphere and -0.75 D cylinder at 0° with a 7-mm area with either a 110-μm flap (FS-LASIK) or a 130-μm cap (SMILE). For 2D biomechanical measurements, corneoscleral discs were subjected to two testing cycles (preliminary strain curve from 0.03 to 9.0 N and stress relaxation at 9.0 N for 120 seconds) to analyze the elastic and viscoelastic properties of the material. The effective elastic modulus was calculated. Statistical analysis was performed with a 95% confidence interval.
In stress-strain measurements, the effective elastic modulus was 1.47 times higher. The effect size is significant. No significant differences were observed among relaxation-stress measurements, with mean remaining stress of 181 ± 31 kPa after SMILE and 177 ± 26 kPa and FS-LASIK after relaxation.
Conclusions: Compared to flap-based procedures such as FS-LASIK, the SMILE technique can be considered superior in terms of biomechanical stability when experimentally measured in human fellow eyes ex vivo.
My comment
: before this, the same results were calculated by mathematical modeling by Professor Ranstein (UK), and Professor Secundo confirmed the theoretical conclusions by measuring on paired human eyes (his corneal strength indicators after SMILE are even higher than in theory) in a special Swiss laboratory. These are truly revolutionary results!
So,
So what is better for myopia?
Let's go through the theses again:
- PRK, femtoLASIK and SMILE operations are no better or worse than each other, each has its own area of application. It is logical to use PRK as a method of additional correction and for special medical purposes. Should not be considered for primary correction. FemtoLASIK can be done if there is no technological or financial opportunity to do SMILE, and the thickness and shape of the cornea allows the cap to be cut off. ReLEx SMILE is the most gentle operation, the operation of choice for myopia and/or myopic astigmatism. It combines the advantages of two predecessor technologies - FemtoLASIK and PRK, but does not have their disadvantages.
- The PRK method (trans-PRK) destroys the outer epithelium of the eye, Bowman's membrane and the upper (most durable) layers of the cornea.
The disadvantages are impaired innervation (and dry eye), opacities during the formation of pseudo-Bowman's membrane, and medium risks of keratoectasia (protrusion of the cornea). The advantage is that you can perform this operation several times. PRK is certified in many countries for active sports. In short, it’s cool for those who love oldstyle technologies - they’re ready to exchange a new Mercedes for an old Volga GAZ-21. - FemtoLASIK suppresses about 75-90% of the superficial nerve endings in the cornea, the remaining ones are barely enough to control trophism, but this is better than burning out the entire surface. The work is carried out in the loose layers of the cornea, the frame suffers due to the cut of the lid. Due to the risk of displacement or tearing, the flap is not permitted for correction in a number of dangerous professions and for athletes. If everything went smoothly, it gives a good optical effect and precise correction.
- SMILE is the most modern method, clinical use for more than 10 years: the first patients (not counting test pigs) have been walking after surgery since 2007. The corneal frame will be preserved, and about 80% of the nerves will be preserved. The application requires a unique VisuMax laser and a well-trained surgeon to extract the excised material through a narrow tunnel. The most painless operation, allowing you to use your eyes from the next day without restrictions - this determines its cost. Provides the least amount of visual distortion due to aberrations. Currently, about two million operations have been performed worldwide, but the number of devices, clinics and operated patients is growing exponentially.
- Laser methods of vision correction are not the only possible methods of surgical vision correction: you can embed lenses into the eye, segments into the cornea, or replace your own lens with an artificial one with new optical properties (more details here).
- Vision correction - in most cases it is done out of a desire to improve the quality of life, rarely for medical reasons. Insurance medicine in most countries (including Russia) does not cover the costs of its implementation. It’s up to you to decide whether to have vision correction or wear glasses/contact lenses, but in any case, to choose the right option you need to be information savvy.
I suggest you decide using the facts.
How is the operation performed?
The operation itself takes no more than 15 minutes. They give you knee-length shoe covers and a sterile cloak. You lie down on the table and look at the red dot at the top. What if you lose it? Everyone lost her, including me. It’s impossible to follow because the lights are shining from above, the doctor is wielding an instrument, drops are dripping. The doctor regularly reminds: “Look at the point.” While the laser is operating, the doctor holds the patient's head with his hands.
Anesthetic is poured into the eye in advance and generously. When the surgeon starts cutting the cornea, you don't feel anything. The laser operates for 40 seconds. At this time, a burning smell appears. The eye is poured with water from a spray bottle. The doctor places a protective lens, which is removed after 4-5 days.
Corridor of the Alexander Tikhov clinic in Yaroslavl
At the very end, you need to close your eyes, the table with the patient moves somewhere to the side, the surgeon takes the operated patient by the shoulders with both hands and in the voice of a necromancer proclaims: “Get up!”
Doctors give you a bandage, look at your eyes again after 10 minutes, give you painkillers - these are diclofenac drops - and send you to a hotel. The hotel is included in the price of the contract. She's five minutes from the clinic. There are good rooms, everything you need is there.