How to find conjunctivitis according to ICD
In the international classification, conjunctivitis corresponds to code H10. Moreover, as is known, this disease has several varieties, which are also listed in the ICD:
- H10.0 - purulent;
- H10.1 - atopic;
- H10.2 - all sharp;
- H10.3 - acute, unspecified;
- H10.4 - chronic;
- H10.5 - blepharoconjunctivitis;
- H10.8 - others;
- H10.9 - unspecified.
A number of conjunctivitis not listed in this list are designated in international documentation using codes H10–H13, depending on the characteristics.
The ICD classification allows doctors and pharmacists from different countries to determine the disease and methods of its treatment, which allows them to use treatment methods that have already been proven in practice. And it is also used when releasing medicines for conjunctivitis for export by some countries, and by others when purchasing and using them, knowing in what case they should be used.
B30.1 Conjunctivitis caused by adenovirus H13.1*
B30.0 Keratoconjunctivitis caused by adenovirus H19.2*
Diagnostics
In the diagnosis and treatment of allergic conjunctivitis, coordinated interaction between an ophthalmologist and an allergist-immunologist is important. If the history shows a clear connection between conjunctivitis and exposure to an external allergen, the diagnosis is usually beyond doubt
An ophthalmological examination reveals changes in the conjunctiva (edema, hyperemia, papillary hyperplasia). Microscopic examination of conjunctival scrapings in allergic conjunctivitis reveals eosinophils (10% and above). In the blood, an increase in IgE of more than 100-150 IU is typical. To determine the cause of allergic conjunctivitis, tests are carried out: elimination, when against the background of clinical manifestations, contact with the suspected allergen is excluded, and exposure, which consists of repeated exposure to this allergen after the symptoms subside. After the acute allergic manifestations of conjunctivitis subside, skin allergic tests (application, scarification, electrophoresis, prick test) are performed. During the period of remission, they resort to provocative tests - conjunctival, sublingual and nasal. In case of chronic allergic conjunctivitis, examination of eyelashes for demodex is indicated. If an eye infection is suspected, a bacteriological examination of a smear from the conjunctiva for microflora is carried out.
What it is?
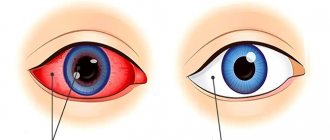
The disease occurs with equal frequency in both adults and children. It is an inflammatory process that affects the mucous membrane of the organ of vision. Pathogenic bacteria begin to actively multiply in the conjunctiva, causing a reaction in the body.
The patient notices redness of the eye and the release of a whitish discharge. Over time, the color of the secretion changes to yellowish or even greenish. On average, the illness lasts about 7–10 days.
Expert opinion
Ermolaeva Tatyana Borisovna
Ophthalmologist of the highest category, Candidate of Medical Sciences
To diagnose purulent conjunctivitis and then prescribe etiotropic treatment, the doctor may refer the patient to a conjunctival smear for microflora. Based on the results of the study, the ophthalmologist will find out which microbe led to the inflammation.
How to forget about eye problems?
Have you ever experienced vision problems? Judging by the fact that you are reading this article, you or your loved ones have encountered this. And you know firsthand what it is:
- When vision in one eye sharply deteriorates;
- The feeling of a black curtain in front of the eyes that covers some part of the field of vision;
- Sharp pain in the eye, redness, blurred vision;
- Blurry, unclear image;
- Dark spots, partial opacities, a feeling of fog or haze before the eyes;
- A burning sensation, sand in the eyes, a sensation of a foreign body, lacrimation or, conversely, a feeling of dryness;
- Floating spots before eyes...
Surely you have tried a bunch of medications, drops, injections, doctors, examinations, and, apparently, none of the above has helped you... And there is an explanation for this: it is simply not profitable for pharmacists to sell a working product, since they will lose customers! It was against this that the leading ophthalmologists and ophthalmologists of Russia jointly spoke out, presenting a long-known effective remedy for EYE PROBLEMS among the people, which REALLY TREATS, and not only reduces pronounced symptoms!
What is keratoconjunctivitis?
For reference! Depending on the etiology, keratoconjunctivitis according to ICD-10 is indicated by different codes:
- H16 (non-infectious origin, occurrence due to external influences);
- H19.8 (keratoconjunctivitis sicca);
- H19.2 and H19.3 (adenoviral and herpetic, respectively).
The disease is an infectious-inflammatory process that develops in the tissues of the cornea and mucous membrane.
Moreover, the conjunctiva is initially affected, since the infection initially settles on it.
But already within a few hours or the first days, pathological processes move from the mucous membrane to the cornea, the tissues of which lie in deeper layers.
Usually the disease is an advanced form of conjunctivitis, which can have such consequences after two weeks.
Note! The risk group includes men aged 55 years and older.
This is explained by the fact that at this age, local immunity is no longer stable, being weakened as a result of the development of age-related degenerative processes in tissues and in the immune system as a whole.
Therefore, men of the older age group should take the most responsible approach to the treatment of even mild conjunctivitis in order to avoid such complications.
It is also necessary to avoid self-medication during the treatment of other ophthalmological diseases.
The risk of developing keratoconjunctivitis may increase during periods of long-term treatment with corticosteroid drugs over a long course.
What kind of disease is this?
Keratoconjunctivitis is an eye disease that occurs with simultaneous inflammation of the cornea and conjunctiva.
Most often it affects people aged 55-79 years , of whom men .
The disease is quite common in the group of ophthalmological pathologies, this is due to its microbial origin and the high susceptibility of the mucous membranes of the eyes to infectious agents.
Non-infectious lesions of this kind are less common.
The disease is usually acute, but with a weakened immune system, ineffective or incomplete treatment, the inflammatory process can become chronic.
Acute keratoconjunctivitis with timely started therapy goes away without a trace, i.e. without complications on the organs of vision. But a constantly progressing process can be dangerous for patients and lead to deterioration of visual acuity, impaired nutrition and eye function.
Keratoconjunctivitis: photo
Bacterial keratoconjunctivitis goes away the fastest, while viral forms of the disease are more difficult and take longer to treat.
Lifelong therapy is required for keratoconjunctivitis that develops against the background of endocrine diseases and systemic pathologies.
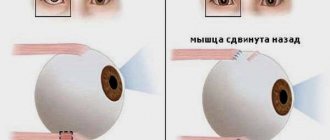
Pathogenesis and pathological picture
text_fieldstext_fieldsarrow_upward
In accordance with the entry gate, the adenovirus is localized initially in the epithelial cells of the mucous membranes of the upper respiratory tract, eyes, and intestines. Its reproduction occurs only inside the affected cells, mainly in the nuclei. During the incubation period, the virus accumulates in epithelial cells and regional lymph nodes. At the same time, the phagocytic activity of the cells of the macrophage system is suppressed, tissue permeability increases, and the virus penetrates the bloodstream, and then other organs. The pathogen is fixed by the cells of the macrophage system of the liver and spleen, causing changes in them, often leading to an enlargement of these organs.
Viremia in adenoviral diseases is long-lasting and can be observed not only in clinically pronounced, but also in asymptomatic forms of the disease. Replication of the virus in lymphoid tissue is accompanied by an increase in the submandibular, cervical, axillary, mesenteric lymph nodes, and inflammatory changes in the tonsils.
Damage to various parts of the respiratory tract and eyes occurs sequentially. The process involves the mucous membrane of the nose, pharynx, trachea, bronchi, tonsils, conjunctiva, cornea, as well as the intestinal mucosa are affected. In case of death, the autopsy reveals the phenomena of peribronchial pneumonia with severe edema and necrosis of the walls of the bronchi and alveoli.
The adenovirus reproduces in intestinal epithelial cells and its lymphatic system. The resulting inflammatory process apparently develops with the participation of intestinal bacterial flora and is clinically manifested by diarrhea and mesadenitis.
Treatment
- identification and elimination of the allergen;
- desensitizing and local therapy;
- symptomatic therapy;
- immunotherapy;
- prevention of secondary infection and complications.
Read more about treatment in adults in this article.
Drops are the main means for treating the disease after eliminating the allergen. Allergodil, Opatanol, Cromohexal, Optikrom are most often prescribed. For dry eyes, drops are prescribed that stimulate tear production; for corneal damage, drops with decaspanthenol are needed; for swelling of the eye, vasoconstrictor drops are prescribed.
Read more about what drops are used in treatment here.
In childhood, it is necessary to exclude the allergen, as well as use drugs that relieve symptoms and strengthen general and local immunity. In some cases, traditional medicine is recommended.
Treatment of the disease
Treatment of each type of conjunctivitis has its own characteristics. If an allergic or medicinal type manifests itself, it is necessary to limit contact with the allergen, which will lead to a weakening of the symptoms, and subsequently complete relief from them. If it is impossible to interrupt contact, antihistamine blockers are used.
Important! Despite the fact that conjunctivitis, code H10 according to the ICD, is a common disease, you should never self-medicate. If any symptoms occur, be sure to see a doctor.
Viral types are treated with special drops, but in addition, do not forget that, as a rule, in this case, conjunctivitis has concomitant diseases, which should also be gotten rid of. In the case of bacterial diseases, the doctor must prescribe antibiotics that attack the source of the problem, and ointments are used to relieve symptoms. Fluoroquinol drugs are also used.
Forms of the disease and characteristics
The clinical picture depends entirely on the causes of the disease and its form. There are two main forms. Firstly, the acute form, it is characterized by the sudden appearance of symptoms of the disease. The eyes quickly turn red, severe pain and itching appear. Sometimes pinpoint bleeding is noticeable. The eyelids swell and discharge appears from the eyes. Secondly, the chronic form, in which inflammation usually spreads to both eyes. The course of the disease is very sluggish, the clinical picture develops gradually. Typically, this form occurs in other chronic diseases in the human body. In addition, there are several types of the disease:
- Viral. Usually develops together with herpes or other viral diseases. Frequent symptoms are severe itching and lacrimation. By the way, the mucus that comes out of the eye is purulent in most cases. The inflammation quickly spreads to both eyes. In addition to such symptoms, you can also notice a runny nose, sore throat, and low-grade fever.
- Bacterial. Usually caused by staphylococcus, streptococcus, gonococcus, pneumococcus. The peculiarity is that the discharge has a gray or cloudy purulent tint. They have a very viscous consistency, which causes the eyelids to stick together, especially after the patient has slept. The skin around the eyes is also affected.
- Fungal. Develops due to exposure to fungal microorganisms on the mucous membranes. Typically these are actinomycetes, molds and yeasts.
- Allergic. Manifests itself as an allergic reaction to something. Characterized by severe pain, burning and itching. Typically, additional symptoms are bronchial asthma and runny nose. If you do not come into contact with the allergen, these symptoms quickly disappear on their own.
- Chemical. In this case, conjunctivitis is caused by toxic or chemical substances that enter the person's eyes. He will complain of severe pain in his eyes, but there are simply no other symptoms.
- Drug. This form is caused by the use of various medications that have caused side effects. Usually, symptoms of conjunctivitis appear in the first 6-8 hours after taking the drug. The clinical picture develops quite quickly, a burning sensation and copious mucus discharge appear.
Classification
The disease is usually divided into separate types and forms.
By type:
Have you ever had purulent conjunctivitis?
Not really
- Pseudomonas aeruginosa . Caused by the bacterium Pseudomonas aeruginosa (Pseudomonas aeruginosa). Usually develops when wearing contact correction products for long-term use.
- Gonococcal . The cause of the disease is Neisseria gonorrhoeae (gonococci). It is characterized by a rather severe course and the threat of serious complications. The disease can be transmitted to the newborn during its passage through the birth canal.
- Staphylococcal . Caused by microbes of the Micrococcaceae family (micrococci). Typically, this type of purulent conjunctivitis affects children who neglect the rules of personal hygiene. It occurs in acute or chronic form.
- Chlamydial . Develops against the background of general chlamydia. The disease is caused by Chlamydia trachomatis (chlamydia trachomatis). Bacteria enter the eyes through the reproductive organs. The peculiarity of the disease is its hidden course. Symptoms are poorly developed, but the disease progresses rapidly, affecting the organ of vision and becoming chronic.
By form:
- Spicy . It is characterized by pronounced manifestations of the disease. For the first symptoms to appear, purulent conjunctivitis requires only a few hours or 1–2 days. The patient is concerned about increased purulent discharge from the eye and redness of the conjunctiva. Usually the illness lasts about 7–10 days. Most often, only one eye is involved in the pathological process.
- Chronic . Characterized by periods of exacerbation and remission. Occurs with mild symptoms.
Prevention
Primary prevention is aimed at preventing the development of allergic conjunctivitis, which primarily includes the formation in patients of a competent attitude towards their health, familiarization with the causes and mechanisms of the development of the disease based on broad information about the features of the development of AK, possible etiological and provoking factors, the need for elimination measures and mandatory compliance with doctor’s orders. Primary prevention should be carried out starting during pregnancy and from the first days of life. During pregnancy, it is necessary to provide proper and varied nutrition, corresponding in volume and ratio of food ingredients to age, body weight, concomitant diseases and energy costs, strict exclusion of active and passive smoking is required, etc. It is necessary to fight and maintain motivation for breastfeeding children. For infants and children at high risk of developing asthma and allergies (this includes children from families where at least one parent or sibling has an allergy), multiple interventions are offered to reduce early life exposure to house dust mites, such as bed covers and special coverings for parent and child beds, washing bedding and soft toys at temperatures exceeding 60 ºС, the use of acaricides, smooth floors without carpets, etc.
Secondary prevention - prevention of exacerbation of allergic conjunctivitis in those people who suffer from allergies: - carefully collect and analyze allergic, pharmacological and nutritional history; – limit contact with the causative allergen as much as possible; – do not prescribe medications manufactured or containing plant materials to patients with seasonal allergic conjunctivitis caused by sensitization to plant pollen; – for patients with allergic conjunctivitis caused by sensitization to medications, do not prescribe these drugs and those similar in chemical structure, and clarify the synonyms of the drugs, since the drug produced by different companies may have different trade names; – do not use cosmetics containing plant materials in patients with seasonal allergic conjunctivitis caused by sensitization to plant pollen; – do not consume food products of plant origin that have cross-reactions with causally significant pollen or fungal allergens.
Tertiary prevention is important for people who have suffered severe complicated manifestations of allergic conjunctivitis, and includes the development of measures for long-term control over the symptoms of the disease: - constant monitoring by an allergist-immunologist; – the patient has a written treatment plan; – education and training of patients, including in allergy schools.
Consequences and complications
Although purulent conjunctivitis rarely leads to the development of various ailments, sometimes the disease threatens with serious complications. These include:
- bacterial keratitis;
- corneal thorn;
- decreased visual acuity;
- corneal ulcer;
- transition to a chronic form.
With timely and adequate therapy, these adverse consequences can be avoided.
Drug-induced conjunctivitis in a child
The disease can occur acutely (within the first hour after using any drug) and subacutely (within the first day after using the drug). Most often (in 90% of cases) drug-induced conjunctivitis occurs with long-term use of drugs (several days or weeks). An allergic reaction can develop both to the drug itself and to the preservative of eye drops, most often with topical use of antibacterial drugs and local anesthetics.
Acute allergic conjunctivitis is characterized by the appearance of rapidly increasing glassy chemosis and edema of the conjunctiva, severe itching, burning, and copious mucous (sometimes filmy) discharge from the conjunctival cavity. Some areas of the mucous membrane may be eroded. Papillary hypertrophy of the upper eyelid is noted; follicles appear in the area of the conjunctiva of the lower transitional fold and the lower eyelid.
Viral conjunctivitis in children
ICD-10 code
- B30.0 Keratoconjunctivitis caused by adenovirus (H19.2).
- B30.1 Conjunctivitis caused by adenovirus (H13.1).
- B30.2 Viral pharyngoconjunctivitis.
- B30.3 Acute epidemic hemorrhagic conjunctivitis (enteroviral; H13.1).
- B30.8 Other viral conjunctivitis (H13.1).
- B30.9 Viral conjunctivitis, unspecified.
- H16 Keratitis.
- H16.0 Corneal ulcer.
- H16.1 Other superficial keratitis without conjunctivitis.
- H16.2 Keratoconjunctivitis (epidemic B30.0 + H19.2).
- H16.3 Interstitial (stromal) and deep keratitis.
- H16.4 Neovascularization of the cornea.
- H16.9 Keratitis, unspecified.
- H19.1 Keratitis caused by herpes simplex virus and keratoconjunctivitis (B00.5).
Adenoviruses cause two clinical forms of eye disease: adenoviral conjunctivitis (pharyngoconjunctival fever) and epidemic keratoconjunctivitis (more severe and accompanied by damage to the cornea). In children, pharyngoconjunctival fever often occurs, and epidemic keratoconjunctivitis occurs less frequently. Viral conjunctivitis is almost always accompanied by a general reaction of the body in the form of damage to the upper respiratory tract, increased body temperature, sleep disturbances and the appearance of dyspepsia, soreness and enlarged lymph nodes.
Adenoviral conjunctivitis (pharyngoconjunctival fever)
The disease is highly contagious and is transmitted by airborne droplets and contact. Mostly children of preschool and primary school age in groups are affected.
Eye damage is preceded by a clinical picture of acute catarrh of the upper respiratory tract with symptoms of pharyngitis, rhinitis, tracheitis, bronchitis, otitis, dyspepsia, and an increase in body temperature to 38-39 ° C.
The incubation period is 3-10 days. The lesion is usually bilateral: first one eye, and after 1-3 days - the second. Characterized by photophobia, lacrimation, swelling and hyperemia of the skin of the eyelids, moderate hyperemia and infiltration of the conjunctiva, scanty serous-mucous discharge, small follicles, especially in the area of transitional folds, and sometimes pinpoint hemorrhages. Less commonly, pinpoint subepithelial infiltrates of the cornea are formed, disappearing without a trace. In children, delicate grayish-white films may form, which, when removed, reveal the bleeding surface of the conjunctiva. Papillary reaction is rarely observed. Half of the children have regional painful pre-auricular adenopathy. All clinical symptoms last no more than 10-14 days.
Epidemic keratoconjunctivitis
The disease is highly contagious. The infection spreads by contact, less commonly by airborne droplets. Infection often occurs in medical institutions. The duration of the incubation period is 4-8 days.
The onset is acute, affecting both eyes. Against the background of moderate respiratory manifestations, almost all patients experience enlargement and tenderness of the parotid lymph nodes. Clinical manifestations are similar to adenoviral conjunctivitis, but more pronounced. The course is more severe: films often form on the conjunctiva and hemorrhages. On the 5-9th day from the onset of the disease, pinpoint subepithelial (coin-shaped) infiltrates appear on the cornea, leading to decreased vision. In their place, persistent corneal opacities form. The duration of the infectious period is 14 days, the duration of the disease is 1-2 months, after recovery immunity remains.
Epidemic hemorrhagic conjunctivitis
It is less common in children than in adults. The causative agent is enterovirus-70. The disease is transmitted by contact; it is distinguished by extremely high contagiousness. “explosive type” of the epidemic, short incubation period (12-48 hours).
On examination: swelling of the eyelids, chemosis and infiltration of the conjunctiva, individual small follicles on the lower transitional fold, moderate mucous or mucopurulent discharge. Hemorrhages into and under the conjunctival tissue are typical, occurring in the first hours of the disease and disappearing after a few days. The sensitivity of the cornea is reduced, sometimes pinpoint subepithelial infiltrates occur, quickly and completely disappearing after a few days. Characterized by enlargement and tenderness of the anterior ear lymph nodes. The duration of the disease is 8-12 days, ending with recovery.
Treatment of bacterial eye conjunctivitis in children
Bacterial conjunctivitis in a child is a quite serious disease, which, if not treated correctly, can cause complications or become chronic. Therefore, when the first symptoms of the disease appear in a child, it is necessary to consult an ophthalmologist.
Furacillin solution is used to wash the eyes. To prepare it, bring 100 ml of water to a boil, add the crushed tablet and boil until completely dissolved. Then the volume of the solution is brought to 100 ml with boiling water.
After the solution has cooled, immerse a sterile cotton or gauze swab in it, wring it out lightly and wash the child’s eyes in the direction from the temple to the nose. It also helps remove crusts and pus. You need to take a separate swab for each eye.
If the inflammation affects only 1 eye, both still need to be washed, since the infection spreads quickly. On the first day of the disease and in the presence of a large amount of pus, the procedure is carried out every 3 hours, and then up to 4 times a day.
To relieve inflammation, use eye drops:
- Sulfacyl Sodium;
- Levomycetin;
- Vitabact;
- Fulcithalmig;
- Normax.
They are used according to the instructions. You need to instill it with a pipette with rounded edges or using a special dropper that comes with the bottles.
Since most eye drops are stored in the refrigerator, you need to warm them first by holding them in your hand. The child should be placed on a flat surface and the solution should be dripped under the lower eyelid. If the baby closes his eyes, just stretch the eyelids slightly with your fingers and drop them into the gap, the medicine will distribute itself after the baby opens his eyes. Excess solution should be blotted off using a sterile gauze pad, a separate one for each eye.
The doctor may also prescribe eye ointments with an antibiotic: Erythromycin or Tetracycline. The ointment is carefully placed under the lower eyelids, slightly pulling them back.
It must be remembered that the vast majority of eye drops have a limited shelf life after opening (usually 28 days). After this period, it is not recommended to use the product. Also, such drugs are stored in a cool place, so do not forget to put them in the refrigerator so that they do not lose their medicinal properties.
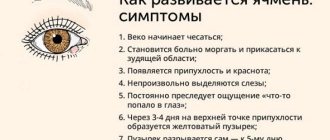
Symptoms
People with all forms of allergic conjunctivitis experience severe itching and burning in both eyes. Although symptoms usually occur in both eyes, in some cases one eye may be more affected than the other. The conjunctiva becomes red and sometimes swells, giving the eyeball a swollen appearance. With seasonal and year-round conjunctivitis, a large amount of liquid, watery discharge appears from the eye, which can sometimes become viscous, and watery lacrimation is observed, sometimes burning. Many people report itchy eyes. Most people suffering from this disease also note the presence of a runny nose. With spring conjunctivitis, the discharge from the eyes is thick and mucus-like. It, unlike other types of allergic conjunctivitis, often causes damage to the cornea and leads to painful ulcers. The latter cause severe pain in the eye when looking at bright light and sometimes lead to permanent loss of vision.
Causes
The development of allergic eye conjunctivitis is based on the mechanism of immediate hypersensitivity; accordingly, the symptoms of the disease occur immediately after contact with the allergen. The human eye, due to its special anatomical structure, is exposed to many external factors that can cause an atypical reaction.
The most common allergens that cause conjunctivitis are:
- Household: dust mites, dust, feathers from pillows, cosmetics, household chemicals, medications (especially eye medications).
- Epidermal: wool, dead animal skin cells, bird feathers, aquarium fish food.
- Pollen: pollen of various plant species during their active flowering period.
At the same time, an allergic reaction to food causes conjunctivitis extremely rarely. Heredity also influences the likelihood of developing symptoms of the disease. Allergic conjunctivitis in children, the treatment of which is quite difficult, especially at an early age, often appears in cases where one or both parents are allergic.
Possible consequences, complications
The disease is dangerous because it can provoke complications. One of them is visual impairment.
After suffering from conjunctivitis, color perception may deteriorate , when the child confuses colors and does not perceive shades. But this rarely happens.
The most common consequence is the transition of the disease to a recurrent chronic form or a protracted illness. Then children constantly need medications to relieve unpleasant symptoms.
The consequence may be suppuration. In this case, the disease is mild.
With a viral type of disease, within 5-7 days from the moment of infection, the body develops immunity against the infection, and the disease passes without a trace.
Among the reasons for the recurrence of conjunctivitis in a child, poor immunity, poor hygiene, and a tendency to allergic reactions should be noted.
You will learn about the causes and methods of treating conjunctivitis, including in children, from this video:
Allergic conjunctivitis
DEFINITION
Allergic conjunctivitis is an inflammatory lesion of the conjunctiva caused by exposure to allergens and characterized by hyperemia and swelling of the mucous membrane; swelling, itching and hyperemia of the skin of the eyelids; the formation of follicles or papillae on the conjunctiva; sometimes damage to the cornea with visual impairment.
ETIOLOGY
Due to their anatomical location, the eyes are highly susceptible to pollen allergens. The most common manifestation of hypersensitivity is inflammation of the conjunctiva (allergic conjunctivitis), but the lesion can affect any part of the eye.
The eyes may be the site of allergic reactions in many systemic immunological disorders, with ocular involvement often being the most dramatic manifestation of the disease. The allergic reaction plays an important role in the clinical picture of infectious eye diseases.
The discovery of the genetic basis of allergic conjunctivitis is very important not only for understanding the molecular etiology, but also for the development of new therapeutic approaches
PATHOGENESIS
Allergic conjunctivitis occurs due to an IgE-mediated hypersensitivity reaction and is more often seasonal, less often year-round. The triggering factor for allergic conjunctivitis is contact of the corresponding allergen with the conjunctiva, which causes degranulation of mast cells, leading to an early phase of clinical response and subsequent allergic inflammatory reaction.
The severity of the disease and its course are related to the concentration of the allergen in the environment and the reactivity of the body. Histamine is the main mediator released by mast cells and influences the development of symptoms of allergic conjunctivitis. It is histamine that causes such characteristic manifestations of allergic conjunctivitis as itching, lacrimation, redness, swelling of the eyelids and conjunctiva.
Hypersensitivity reactions are classified into immediate (develop within 30 minutes of exposure to the allergen) and delayed (occur 24-48 hours or later). This division of allergic reactions is of practical importance in prescribing drug treatment. Immediate reactions cause a simultaneous release into the tissue (at the site of contact with the allergen) of a large amount of biologically active substances from mast cell granules, basocytes and eosinophils (degranulation).
CLINICAL PICTURE
Although all ocular allergies have a common pathophysiological mechanism, they differ in their clinical manifestations, which complicates and complicates the diagnosis and treatment of the disease.
DIAGNOSTICS
In some cases, the typical picture of the disease or a clear connection with the effects of an external allergenic factor leaves no doubt about the diagnosis. In most cases, the diagnosis of allergic eye diseases is fraught with great difficulties and requires the use of specific allergological research methods.
CLASSIFICATION
The most frequently identified clinical forms of allergic conjunctivitis are the following, characterized by their own characteristics in the choice of treatment:
? hay fever conjunctivitis:
? vernal keratoconjunctivitis;
? large papillary conjunctivitis;
? drug allergies;
? chronic allergic conjunctivitis.
conclusions
As a rule, adenoviral conjunctivitis develops after a runny nose and pharyngitis. Therefore, with the right actions at the very beginning of infection, eye infection can be completely avoided.
However, if this does happen, do not let the disease take its course and visit a doctor, even if you are not going to take strong medications. After all, the virus can have a completely different nature and serious complications in case of inadequate therapy.
The main obstacle to infection can be the immune system. Strengthen it in every possible way, and not only with pharmacy vitamins. After all, natural food gives the body not only vitamin components and essential microelements, but also supplies tissues with building material to create new cells to replace dead ones. That is why give preference to natural fish and meat over ready-made sausages or canned food. This will help to avoid slagging of the body and will also serve to strengthen the immune system.