ICD 10. CLASS VII. Diseases of the eye and its adnexa (H00-H59)
Excluded: certain conditions arising in the perinatal period ( P00 - P96 ) some infectious and parasitic diseases ( A00 - B99 ) complications of pregnancy, childbirth and the postpartum period ( O00 - O99 ) congenital anomalies, deformations and chromosomal disorders ( Q00 - Q99 ) endocrine diseases systems, nutritional disorders and metabolic disorders ( E00 - E90 ) trauma, poisoning and some other consequences of external causes ( S00 - T98 ) neoplasms ( C00 - D48 ) symptoms, signs and abnormalities identified during clinical and laboratory tests , not classified elsewhere ( R00 - R99 )
This class contains the following blocks: H00 - H06 Diseases of the eyelids, lacrimal ducts and orbit H10 - H13 Diseases of the conjunctiva H15 - H22 Diseases of the sclera, cornea, iris and ciliary body H25 - H28 Diseases of the lens H30 - H36 Diseases of the choroid and retina H40 - H42 Glaucoma H43 - H45 Diseases of the vitreous body and eyeball H46 - H48 Diseases of the optic nerve and visual pathways H49 - H52 Diseases of the eye muscles, disorders of concomitant eye movement, accommodation and refraction H53 - H54 Visual disorders and blindness H55 - H59 Other diseases of the eye and its adnexa apparatus
The following categories are marked with an asterisk: H03 * Lesions of the eyelid in diseases classified in other headings H06 * Lesions of the lacrimal apparatus and orbit in diseases classified in other headings H13 * Lesions of the conjunctiva in diseases classified in other headings H19 * Lesions of the sclera and cornea in diseases classified elsewhere H22 * Lesions of the iris and ciliary body in diseases classified elsewhere H28 * Cataracts and other lesions of the lens in diseases classified elsewhere H32 * Chorioretinal disorders in diseases classified elsewhere H36 * Disorders of the retina in diseases classified elsewhere H42 * Glaucoma in diseases classified elsewhere H45 * Disorders of the vitreous body and eyeball in diseases classified elsewhere H48 * Disorders of the optic [2nd] nerve and visual pathways in diseases , classified elsewhere H58 * Other lesions of the eye and its adnexa in diseases classified elsewhere
Causes of cataracts
Classification by etiology
Classification according to the degree of progression • Stationary (most often congenital, opacification does not change over time) • Progressive (almost always acquired, opacification of the lens increases over time).
Clinical picture
• General symptoms •• Painless progressive decrease in visual acuity •• Fog before the eyes, distortion of the shape of objects •• Ophthalmological examination reveals clouding of the lens of varying severity and localization.
DISEASES OF THE EYELIDS, LACRIMAL DUCT AND ORBITS (H00-H06)
H00 Hordeolum and chalazion
H00.0 Hordeolum and other deep inflammations of the eyelids Abscess } Furuncle } eyelids Stye } H00.1 Chalazion
H01 Other inflammations of the eyelids
H01.0 Blepharitis Excludes: blepharoconjunctivitis ( H10.5 ) H01.1 Non-infectious dermatoses of the eyelid Dermatitis: • allergic } • contact } • eczematous } eyelid Disciform erythematous lupus } Xeroderma } H01.8 Other inflammations of the eyelid, specified H01.9 Inflammation of the eyelid, unspecified
H02 Other eyelid diseases
Excludes: congenital malformations of the eyelid ( Q10.0 - Q10.3 ) H02.0 Entropion and trichiasis of the eyelid H02.1 Ectropion of the eyelid H02.2 Lagophthalmos H02.3 Blepharochalasis H02.4 Ptosis of the eyelid H02.5 Other diseases affecting the function of the eyelid Ankyloblepharon . Blepharophimosis. Wrinkling of the eyelid Excludes: blepharospasm ( G24.5 ) tic (psychogenic) ( F95 . -) • organic ( G25.6 ) H02.6 Xanthelasma of the eyelid H02.7 Other degenerative diseases of the eyelid and periocular region Chloasma } Madarosis } eyelid Vitiligo } H02. 8 Other specified diseases of the century. Hypertrichosis of the century. Unremoved foreign body in eyelid H02.9 Disease of eyelid, unspecified
H03* Lesions of the eyelid in diseases classified elsewhere
H03.0 * Parasitic diseases of the eyelid in diseases classified elsewhere Dermatitis of the eyelid caused by Demodex species ( B88.0 +) Lesions of the eyelid in: • leishmaniasis ( B55 . -+) • loiasis ( B74.3 +) • onchocerciasis ( B73 +) • lice ( B85.3 ) H03.1 * Lesions of the eyelid in other infectious diseases classified in other headings Lesions of the eyelid in: • herpes virus infection ( B00.5 +) • leprosy ( A30 . -+) • molluscum contagiosum ( B08.1 +) • tuberculosis ( A18.4 +) • yaws ( A66 . -+) • herpes zoster ( B02.3 +) H03.8 * Lesions of the eyelid in other diseases classified in other headings. Lesions of the eyelid with impetigo ( L01.0 +)
H04 Diseases of the lacrimal apparatus
Excluded: congenital malformations of the lacrimal apparatus ( Q10.4 - Q10.6 ) H04.0 Dacryoadenitis. Chronic hypertrophy of the lacrimal gland H04.1 Other diseases of the lacrimal gland. Dacryops. Dry eye syndrome Lacrimal gland: • cyst • atrophy H04.2 Epiphora H04.3 Acute and unspecified inflammation of the lacrimal ducts. Dacryocystitis (phlegmatous) } Dacryopericystitis } acute, subacute or Lacrimal canaliculitis } unspecified Excludes: dacryocystitis of the newborn ( P39.1 ) H04.4 Chronic inflammation of the lacrimal ducts Dacryocystitis } Lacrimal gland: } • canaliculitis } chronic • mucocele } H04.5 Stenosis and insufficiency of the lacrimal ducts. Dacryolite. Eversion of the lacrimal punctum Stenosis of the lacrimal: • canaliculus • duct • sac H04.6 Other changes in the lacrimal ducts. Lacrimal fistula H04.8 Other diseases of the lacrimal apparatus H04.9 Disease of the lacrimal apparatus, unspecified
H05 Diseases of the orbit
Excluded: congenital malformations of the orbit ( Q10.7 ) H05.0 Acute inflammation of the orbit Abscess } Cellulitis } Osteomyelitis } orbit Periostitis } Tenonitis H05.1 Chronic inflammatory diseases of the orbit. Granuloma of the orbit H05.2 Exophthalmic conditions Displacement of the eyeball (external) NOS Hemorrhage } Edema } of the orbit H05.3 Deformation of the orbit Atrophy } Exostosis } of the orbit H05.4 Enophthalmos H05.5 Unremoved long-standing foreign body due to penetrating injury to the orbit Retrobulbar foreign body H05.8 Other diseases of the orbit. Orbital cyst H05.9 Disease of the orbit, unspecified
H06* Lesions of the lacrimal apparatus and orbit in diseases classified elsewhere
H06.0 * Lesions of the lacrimal apparatus in diseases classified elsewhere H06.1 * Parasitic invasion of the orbit in diseases classified elsewhere Infection of the orbit with echinococci ( B67 . -+) Orbital myiasis ( B87.2 +) H06.2 * Exophthalmos due to dysfunction of the thyroid gland ( E05 . -+) H06.3 * Other lesions of the orbit, in diseases classified elsewhere
CONJUNCTIVAL DISEASES (H10-H13)
H10 Conjunctivitis
Excludes: keratoconjunctivitis ( H16.2 ) H10.0 Mucopurulent conjunctivitis H10.1 Acute atopic conjunctivitis H10.2 Other acute conjunctivitis H10.3 Acute conjunctivitis, unspecified Excludes: ophthalmia of the newborn NOS ( P39.1 ) H10.4 Chronic conjunctivitis H1 0. 5 Blepharoconjunctivitis H10.8 Other conjunctivitis H10.9 Conjunctivitis, unspecified
H11 Other diseases of the conjunctiva
Excluded: keratoconjunctivitis ( H16.2 ) H11.0 Pterygium Excluded: pseudopterygium ( H11.8 ) H11.1 Conjunctival degeneration and deposits Conjunctival: • argyria • calculi • pigmentation • xerosis NOS H11.2 Conjunctival scars. Symblepharon H11.3 Conjunctival hemorrhage. Subconjunctival hemorrhage H11.4 Other conjunctival vascular diseases and cysts Conjunctival: • aneurysm • hyperemia • edema H11.8 Other specified diseases of the conjunctiva. Pseudopterygium H11.9 Disease of the conjunctiva, unspecified
H13* Lesions of the conjunctiva in diseases classified elsewhere
H13.0 * Filarial invasion of the conjunctiva ( B74 . -+) H13.1 * Acute conjunctivitis in diseases classified elsewhere Conjunctivitis (caused by): • acanthamoeba ( B60.1 +) • adenoviral follicular (acute) ( B30.1 + ) • chlamydial ( A74.0 +) • diphtheria ( A36.8 +) • gonococcal ( A54.3 +) • hemorrhagic (acute) (epidemic) ( B30.3 +) • herpesvirus ( B 00.5 +) • meningococcal ( A39 .8 +) • Newcastle ( B30.8 +) • herpes zoster ( B02.3 +) H13.2 * Conjunctivitis in diseases classified elsewhere H13.3 * Ocular pemphigoid ( L12 . -+) H13. 8 * Other lesions of the conjunctiva in diseases classified elsewhere
DISEASES OF THE SCLERA, CORNEA, IRIS AND CILIARY BODY (H15-H22)
H15 Diseases of the sclera
H15.0 Scleritis H15.1 Episcleritis H15.8 Other scleral lesions. Equatorial staphyloma. Scleral ectasia Excludes: degenerative myopia ( H44.2 ) H15.9 Disease of the sclera, unspecified
H16 Keratitis
H16.0 Corneal ulcer Ulcer: • cornea: • NOS • central • marginal • perforated • annular • with hypopyon • Moray
H16.1 Other superficial keratitis without conjunctivitis Keratitis: • areolar • filiform • coin • card-shaped • stellate • banded • superficial punctate Photokeratitis Snow blindness H16.2 Keratoconjunctivitis Keratoconjunctivitis: • NOS • externally caused • neurotrophic • phlyctenulous Nodular [nodular] ophthalmia Superficial keratitis with conjunctivitis H16.3 Interstitial (stromal) and deep keratitis H16.4 Neovascularization of the cornea. Shadow-like vessels (corneal). Pannus (corneal) H16.8 Other forms of keratitis H16.9 Keratitis, unspecified
H17 Scars and corneal opacities
H17.0 Adhesive leukoma H17.1 Other central corneal opacities H17.8 Other corneal scars and opacities H17.9 scars and opacities, unspecified
H18 Other corneal diseases
H18.0 Pigmentation and deposits in the cornea. Hemorrhage into the cornea. Kaiser-Fleischer ring Krukenberg spindle. Stagley Line If it is necessary to identify the drug that caused the lesion, use an additional external cause code (class XX). H18.1 Bullous keratopathy H18.2 Other corneal edema H18.3 Changes in the membranes of the cornea Fold } Rupture } of Descemet's membrane H18.4 Degeneration of the cornea. Senile arc. Band keratopathy Excludes: Moray ulcer ( H16.0 ) H18.5 Hereditary corneal dystrophies Dystrophy: • corneas: • epithelial • granular ethmoid • macular • Fuchs H18.6 Keratoconus H18.7 Other deformations of the cornea Corneas: • ectasia • staphyloma Descemetocele Excludes: congenital malformations of the cornea ( Q13.3 - Q13.4 ) H18.8 Other specified diseases of the cornea Anesthesia } Hypesthesia } of the cornea Recurrent erosion } H18.9 Disease of the cornea, unspecified
H19* Lesions of the sclera and cornea in diseases classified elsewhere
H19.0 * Scleritis and episcleritis in diseases classified elsewhere Syphilitic episcleritis ( A52.7 +) Tuberculous episcleritis ( A18.5 +) Scleritis (in herpes zoster) ( B02.3 +) H19.1 * Keratitis caused by a virus herpes simplex, and keratoconjunctivitis ( B00.5 +) Tree, discoid and card-shaped keratitis H19.2 * Keratitis and keratoconjunctivitis in other infectious and parasitic diseases classified elsewhere. Infectious keratoconjunctivitis ( B30.0 +) Keratitis and keratoconjunctivitis (interstitial) (stromal) with: • acanthamoebiasis ( B60.1 +) • measles ( B05.8 +) • syphilis ( A50.3 +) • tuberculosis ( A18.5 +) • herpes zoster ( B02.3 +) H19.3 * Keratitis and keratoconjunctivitis in diseases classified elsewhere Keratoconjunctivitis sicca ( M35.0 +) H19.8 * Other lesions of the sclera and cornea in diseases classified classified in other sections Keratoconus in Down's disease ( Q90 . -+)
H20 Iridocyclitis
H20.0 Acute and subacute iridocyclitis Anterior uveitis } Cyclitis } acute recurrent or subacute Iritis } H20.1 Chronic iridocyclitis H20.2 Lens-induced iridocyclitis H20.8 Other iridocyclitis H20.9 Iridocyclitis, unspecified
H21 Other diseases of the iris and ciliary body
Excludes: sympathetic uveitis ( H44.1 ) H21.0 Hyphema Excludes: traumatic hyphema ( S05.1 ) H21.1 Other vascular diseases of the iris and ciliary body Neovascularization of the iris or ciliary body. Rubeosis of the iris H21.2 Degeneration of the iris and ciliary body Degeneration of: • iris (pigmented) • pupillary margin Iridoschisis. Iris atrophy (essential) (progressive) Miotic cyst of the pupil. Transillumination of the iris H21.3 Cyst of the iris, ciliary body and anterior chamber of the eye Cyst of the iris, ciliary body and anterior chamber: • NOS • exudative • implantation • parasitic Excludes: miotic cyst of the pupil ( H21.2 ) H21.4 Pupillary membranes. Bombardment of the iris Pupillary: • fusion • fusion H21.5 Other types of adhesions and ruptures of the iris and ciliary body Goniosynechia. Iridodialysis. Deepening of the angle of the chamber of the synechia (iris): • NOS • anterior • posterior Excludes: corectopia ( Q13.2 ) H21.8 Other specified diseases of the iris and ciliary body H21.9 Disease of the iris and ciliary body, unspecified
H22* Lesions of the iris and ciliary body in diseases
classified elsewhere
H22.0 * Iridocyclitis in infectious diseases classified in other headings Iridocyclitis in: • gonococcal infection ( A54.3 +) • herpes virus infection ( B00.5 +) • syphilis (secondary) ( A51.4 +) • tuberculosis ( A18 .5 +) • herpes zoster ( B02.3 +) H22.1 * Iridocyclitis in diseases classified elsewhere Iridocyclitis in: • ankylosing spondylitis ( M45 +) • sarcoidosis ( D86.8 +) H22.8 * Other lesions of the iris and ciliary body in diseases classified elsewhere
Contraindications for pseudophakia
Contraindications for pseudophakia exist in the following cases:
The list contains relative and absolute contraindications, so you should definitely undergo an examination before the operation. After reviewing the results, the ophthalmologist will allow or prohibit the installation of the implant.
DISEASES OF THE LENS (H25-H28)
H25 Senile cataract
Excludes: capsular glaucoma with false lens detachment ( H40.1 ) H25.0 Initial senile cataract Senile cataract: • coronal • cortical • punctate Subcapsular polar senile cataract (anterior) (posterior). Water gaps H25.1 Senile nuclear cataract. Brown cataract. Nuclear sclerotic cataract H25.2 Senile blinking cataract. Senile overripe cataract H25.8 Other senile cataracts. Combined forms of senile cataract H25.9 Senile cataract, unspecified
H26 Other cataracts
Excludes: congenital cataract ( Q12.0 ) H26.0 Childhood, juvenile and presenile cataract H26.1 Traumatic cataract If necessary to identify the cause, use an additional code for external causes (Class XX). H26.2 Complicated cataract. Cataract in chronic iridocyclitis Secondary cataract in eye diseases. Glaucomatous flecks (subcapsular) H26.3 Drug-induced cataracts If it is necessary to identify the drug causing the lesion, use an additional external cause code (Class XX). H26.4 Secondary cataract. Secondary cataract. Semmering's ring H26.8 Other specified cataract H26.9 Cataract, unspecified
H27 Other lens diseases
Excludes: congenital lens defects ( Q12.- ) mechanical complications associated with an implanted lens ( T85.2 ) pseudophakia ( Z96.1 ) H27.0 Aphakia H27.1 Lens luxation H27.8 Other specified lens diseases H27.9 Lens disease unspecified
H28* Cataracts and other lesions of the lens in diseases classified elsewhere
H28.0 * Diabetic cataract ( E10 - E14 + with a common fourth sign .3) H28.1 * Cataract in other diseases of the endocrine system, nutritional disorders and metabolic disorders classified elsewhere Cataract in hypoparathyroidism ( E20 . -+) Cataract with malnutrition and dehydration ( E40 - E46 +) H28.2 * Cataracts in other diseases classified elsewhere Myotonic cataract ( G71.1 +) H28.8 * Other lens lesions in diseases classified elsewhere
Diagnostics
Physical examination reveals a decrease in the transparency of the anterior segment of the eyes, which may be combined with signs of traumatic injury. When the eyes move, phacodonesis develops, which is detected by an ophthalmologist under focal lighting. When performing a test with mydriatics, no reaction of the pupils is observed. Special diagnostic methods include the use of: • Non-contact tonometry.
When measuring intraocular pressure, it is possible to diagnose its increase.
IOP reaches critical values only when the outflow of aqueous humor is impaired. A mobile dislocation causes a slight increase in ophthalmotonus. • Visometry.
Visual acuity decreases sharply, regardless of the degree of transparency of the lens.
With the additional use of computer refractometry, it is possible to diagnose the myopic type of clinical refraction. • Ultrasound of the eye.
An ultrasound examination reveals a dislocation in the anterior chamber area or the vitreous body.
A unilateral or bilateral rupture of the ligament of Zinn is determined. The vitreal cavity has a non-homogeneous structure. When the lens is fixed to the retina, retinal detachment occurs. The anteroposterior axis is shifted. When completely ruptured, the capsule with the main substance acquires a spherical shape. • Biomicroscopy of the eye.
With the traumatic genesis of the disease, injection of conjunctival vessels and foci of hemorrhage are visualized.
The transparency of optical media is reduced. Secondary changes in the cornea are represented by microerosive defects. • Gonioscopy.
When the displacement vector is directed anteriorly, the volume of the eye chamber is sharply reduced.
In patients with an incomplete form of pathology, the space limited by the iris and cornea is deep, without pathological changes. The anterior chamber angle (ACA) has an uneven structure. • Optical coherence tomography (OCT).
The study makes it possible to determine the nature of the location of the luxated lens and the type of damage to the ligament of Zinn.
OCT is used immediately before surgery to select the optimal surgical tactics. • Ultrasonic biomicroscopy.
In the case of a congenital variant of the disease, the technique makes it possible to detect defects in the ciliary ligament over a range of 60° to 260°. The lens is displaced in the horizontal and vertical planes. The depth of corneal damage is measured. In case of traumatic origin of the disease, patients are additionally prescribed radiography of the orbits in direct and lateral projection. In the early postoperative period, IOP measurement using a non-contact method is indicated. To study the nature of the circulation of the intraocular fluid 5-7 days after surgery, electron tonography is used. The study determines the risk of developing glaucoma.
DISEASES OF THE VACUUM AND RETINA (H30-H36)
H30 Chorioretinal inflammation
H30.0 Focal chorioretinal inflammation Focal: • chorioretinitis • choroiditis • retinitis • retinochoroiditis H30.1 Disseminated chorioretinal inflammation Disseminated: • chorioretinitis • choroiditis • retinitis • retinochoroiditis Excludes: exudative retinopathy ( H35.0 ) H30.2 Posterior cyclitis. Pars planitis H30.8 Other chorioretinal inflammations. Harada disease H30.9 Chorioretinal inflammation, unspecified Chorioretinitis } Choroiditis } Retinitis } NOS Retinochoroiditis }
H31 Other diseases of the uvea
H31.0 Chorioretinal scars Macular scars of the posterior pole (post-inflammatory) (post-traumatic). Solar retinopathy H31.1 Degeneration of the choroid Atrophy } Sclerosis } of the choroid Excluded: angioid streaks ( H35.3 ) H31.2 Hereditary dystrophy of the choroid. Choroiderma Choroidal dystrophy (central-areolar) (generalized) (peripapillary) Ring-shaped atrophy of the choroid Excludes: ornithinemia ( E72.4 ) H31.3 Hemorrhage and rupture of the choroid Choroidal hemorrhage: • NOS • expulsive H31.4 Detachment of the choroid eyes H31.8 Other specified diseases of the choroid H31.9 Disease of the choroid, unspecified
H32* Chorioretinal disorders in diseases classified elsewhere
H32.0 * Chorioretinal inflammation in infectious and parasitic diseases classified elsewhere Chorioretinitis: • late syphilitic ( A52.7 +) • toxoplasmosis ( B58.0 +) • tuberculous ( A18.5 +) H32.8 * Other chorioretinal disorders in diseases classified elsewhere
H33 Retinal detachment and tears
Excludes: retinal pigment epithelial detachment ( H35.7 ) H33.0 Retinal detachment with retinal break. Retinal detachment due to rupture H33.1 Retinoschisis and retinal cysts. Serrated margin cyst. Parasitic retinal cyst. Retinal pseudocyst Excludes: congenital retinoschisis ( Q14.1 ) microcystic retinal degeneration ( H35.4 ) H33.2 Serous retinal detachment Retinal detachment: • NOS • without retinal break Excludes: central serous chorioretinopathy ( H35.7 ) H33.3 Retinal breaks without retinal detachment Horseshoe break } Round hole } retina without detachment Operculum Retinal tear NOS Excludes: chorioretinal scars after surgery for retinal detachment ( H59.8 ) peripheral retinal degeneration without break ( H35.4 ) H33.4 Tractional retinal detachment. Proliferative vitreoretinopathy with retinal detachment H33.5 Other forms of retinal detachment
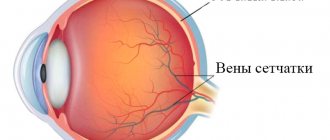
H34 Retinal vascular occlusions
Excludes: transient blindness ( G45.3 ) H34.0 Transient retinal arterial occlusion H34.1 Central retinal arterial occlusion H34.2 Other retinal arterial occlusions Hollenhorst patch Retinal: • arterial occlusion: • branches • partial • microembolism H34.8 Other retinal vascular occlusions Retinal venous occlusion: • central • initial • partial • branch venous H34.9 Retinal vascular occlusion, unspecified
H35 Other retinal diseases
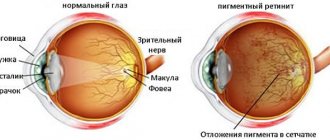
H35.0 Background retinopathy and retinal vascular changes Changes in the retinal vascular pattern Retinal: • microaneurysms • neovascularization • perivasculitis • varices • vascular sheaths • vasculitis Retinopathy: • NOS • background NOS • Coates • exudative • hypertensive H35.1 Pre-retinopathy. Retrolental fibroplasia H35.2 Other proliferative retinopathy. Proliferative vitreoretinopathy Excludes: proliferative vitreoretinopathy with retinal detachment ( H33.4 ) H35.3 Macular and posterior pole degeneration Angioid streaks } Cyst } Drusen (degenerative) } Macula Hole } Wrinkling } Kunta-Junius degeneration Senile macular degeneration (atrophic) (exudative Naya ). Toxic maculopathy If it is necessary to identify the drug causing the lesion, use an additional external cause code (Class XX). H35.4 Peripheral retinal degenerations Retinal degeneration: • NOS • latticework • microcystic • palisade • cobblestone • reticular Excludes: with retinal break ( H33.3 ) H35.5 Hereditary retinal dystrophies Dystrophies: • retinal (albipunctate) ( pigmentosa) (yolk-like) • taperetinal • vitreoretinal Retinitis pigmentosa. Stargardt disease H35.6 Retinal hemorrhage H35.7 Splitting of the layers of the retina. Central serous chorioretinopathy. Retinal pigment epithelial detachment H35.8 Other specified retinal disorders H35.9 Disease of the retina, unspecified
H36* Retinal lesions in diseases classified elsewhere
H36.0 * Diabetic retinopathy ( E10 - E14 + with a common fourth character .3) H36.8 * Other retinal disorders in diseases classified elsewhere Atherosclerotic retinopathy ( I70.8 +) Proliferative sickle cell retinopathy ( D57 . - +) Retinal dystrophy in lipid storage diseases ( E75 . -+)
Dislocation of the artificial eye lens (IOL)
If the degree of displacement of the intraocular lens is insignificant, then this most often does not affect visual acuity and does not require re-operation.
Typically, the causes of dislocation are incorrect placement of the lens during surgery, intraoperative damage to the ligamentous-capsular apparatus of the lens, and asymmetric placement of the lens haptics. Severe IOL displacement occurs in 0.2-2.8% of cases. This requires surgical correction and reoperation. Due to the introduction of phacoemulsification into clinical practice, the incidence of serious lens dislocation has increased. There are also descriptions of IOL dislocation during laser capsulotomy using an Nd:YAG laser.
The main reason for severe IOL dislocation is damage during surgery or in the postoperative period of SCA. At the same time, during surgery the SCAH is damaged in 1-2% of cases.
However, it is almost always possible to implant a posterior chamber IOL into the capsular bag or ciliary sulcus. To do this, use the remaining fragments of the capsular bag as a support.
At the same time, anterior vitrectomy or implantation of intracapsular rings is performed.
If the remaining supporting parts of the SCAH are incorrectly assessed or the listed manipulations are not fully performed, then dislocation of the IOL into the vitreous substance or onto the surface of the fundus may occur. Less commonly, lens displacement leads to the development of hemophthalmos, sluggish uveitis, proliferating vitreoretinopathy, retinal detachment, and chronic macular edema.
our doctor on the topic
Depending on the degree of dislocation of the artificial lens, the doctor chooses one or another surgical approach. The presence of concomitant complications is also taken into account, for example, macular edema, retinal detachment, lenticular masses in the fundus or vitreous.
There are two types of access: anterior, or corneal, and posterior, carried out through the flat part of the ciliary body.
The corneal approach is most often used when the lens or its haptics are located in the surgeon's field of vision, and he can capture from transpupillary.
The indication for a posterior approach is complete dislocation of the IOL into the vitreous substance or into the plane of the fundus. This operation belongs to the section of vitreoretinal surgery. The posterior approach helps to perform all necessary vitreoretinal manipulations.
If the IOL is dislocated, you can replace the posterior chamber lens model with an anterior chamber one, reposition the posterior chamber lens, and remove the IOL without implanting another lens. When replacing a posterior chamber IOL with an anterior chamber one, it is carried out if the structure of the lens is such that it is impossible to carry out its reposition and suture fixation.
Modern models of anterior chamber lenses are used to replace posterior chamber devices. In this case, implantation is safe, and suture fixation is not required. In this case, the percentage of specific complications is very small. The resulting visual acuity is comparable to that obtained with posterior chamber lens reimplantation.
Sometimes it even exceeds this figure.
When repositioning the posterior chamber IOD, a number of manipulations are performed:
- Placement of the lens in the ciliary sulcus and its transscleral suture fixation, including endoscopic control.
- Placement of the lens in the ciliary sulcus using the remaining fragments of the capsular bag (without suture fixation).
- Suture fixation of the lens to the iris.
- Moving the IOL into the anterior chamber (very rarely performed).
Most often, a posterior capsular IOL is placed in the ciliary sulcus and then additionally secured with suture material through a transscleral approach.
This type of operation is technically quite difficult to perform, since there is a high risk of complications (endophthalmitis, hemophthalmos, sluggish chronic uveitis, scleral fistulas, vitreous entrapment, re-dislocation of the IOL, retinal detachment).
Also, when conducting ultrasound biomicroscopy after surgery, it was found that less than half of the interventions (37-40%) led to the correct position of the IOL in the ciliary sulcus. In other cases, the haptic part of the lens shifts anteriorly or posteriorly relative to the ciliary groove.
It should be noted once again that dislocation of the artificial lens is a rather rare, but very serious complication of surgical treatment of cataracts. Depending on the presence of remnants of the capsular bag, the model of the dislocated lens, and associated complications, further treatment tactics change. With the right approach, excellent functional and anatomical results can be achieved.
Treatment prices
The cost of manipulations with an intraocular lens (centration, suturing, dissection of adhesions, capsules, etc.) in our ophthalmology center is 50,000 rubles (for 1 eye). The choice of method is determined after examination by an ophthalmologist.
Source: https://moscoweyes.ru/catatakta-glaza/dislokatsiya-iskusstvennogo-khrustalika-glaza-iol
GLAUCOMA (H40-H42)
H40 Glaucoma
Excluded: absolute glaucoma ( H44.5 ) congenital glaucoma ( Q15.0 ) traumatic glaucoma due to birth injury ( P15.3 ) H40.0 Suspicion of glaucoma. Ocular hypertension H40.1 Primary open-angle glaucoma Glaucoma (primary) (residual stage): • capsular with false lens detachment • chronic simple • with low pressure • pigmentary H40.2 Primary angle-closure glaucoma Closed-angle glaucoma (primary) (residual stage): • acute • chronic • intermittent H40.3 Secondary post-traumatic glaucoma If necessary, use an additional code to identify the cause. H40.4 Glaucoma secondary to inflammatory disease of the eye Use an additional code if necessary to identify the cause. H40.5 Glaucoma secondary to other eye diseases Use an additional code if necessary to identify the cause. H40.6 Secondary drug-induced glaucoma When it is necessary to identify the drug causing the lesion, use an additional external cause code (Class XX). H40.8 Other glaucoma H40.9 Glaucoma, unspecified
H42* Glaucoma in diseases classified elsewhere
H42.0 * Glaucoma in diseases of the endocrine system, nutritional disorders and metabolic disorders Glaucoma in: • amyloidosis ( E85 . -+) • Lowe's syndrome ( E72.0 +) H42.8 * Glaucoma in other diseases classified elsewhere Glaucoma for onchocerciasis ( B73 +)
Symptoms
The pathology is characterized by a severe course. In the congenital form of the disease, parents note a whitish-gray clouding of the anterior part of the eyeball in the child. Severe visual dysfunction is observed, only the ability to perceive light is preserved. If there is a genetic predisposition, symptoms may develop in later life. Patients associate the occurrence of clinical manifestations with minor physical activity or minor trauma. Accommodative ability is sharply impaired. Attempts to fixate the gaze lead to rapid fatigue and headaches. Associated symptoms: Swelling of the eyes.
DISEASES OF THE VITROUS AND EYEBALL (H43-H45)
H43 Vitreous diseases
H43.0 Vitreous prolapse (prolapse) Excludes: vitreous syndrome after cataract surgery ( H59.0 ) H43.1 Vitreous hemorrhage H43.2 Crystalline deposits in the vitreous H43.3 Other vitreous opacities H43.8 Other diseases of the vitreous Vitreous: • degeneration • detachment Excludes: proliferative vitreoretinopathy with retinal detachment ( H33.4 ) H43.9 Disease of the vitreous, unspecified
H44 Diseases of the eyeball
Includes: disorders affecting multiple structures of the eye H44.0 Purulent endophthalmitis. Panophthalmitis. Vitreous abscess H44.1 Other endophthalmitis. Parasitic endophthalmitis NOS. Sympathetic uveitis H44.2 Degenerative myopia H44.3 Other degenerative diseases of the eyeball. Chalkosis. Siderosis of the eye H44.4 Hypotony of the eye H44.5 Degenerative conditions of the eyeball. Absolute glaucoma Atrophy of the eyeball. Wrinkling of the eyeball H44.6 Unremoved (long-standing in the eye) magnetic foreign body Preserved old magnetic foreign body in: • anterior chamber • ciliary body • • lens • posterior wall of the eyeball • vitreous body H44.7 Unremoved (long-standing in the eye) magnetic foreign body eye) non-magnetic foreign body Unremoved (non-magnetic) (old) foreign body in: • anterior chamber • ciliary body • iris • lens • posterior wall of the eye • vitreous body H44.8 Other diseases of the eyeball. Hemophthalmos. Luxation of the eyeball H44.9 Disease of the eyeball, unspecified
H45* Lesions of the vitreous body and eyeball in diseases classified elsewhere
H45.0 * Hemorrhage into the vitreous body in diseases classified in other headings H45.1 * Endophthalmitis in diseases classified in other headings Endophthalmitis in: • cysticercosis ( B69.1 +) • onchocerciasis ( B73 +) • toxocariasis ( B83 . +) H45.8 * Other lesions of the vitreous body and eyeball in diseases classified elsewhere
Types of IOLs
Size and installation method divides intraocular lenses into several types:
- anterior chamber;
- posterior capsule;
- pupillary;
- toric;
- posterior chamber.
Anterior chamber IOLs
implanted into the space between the cornea and iris, after making an incision.
Used for the following diseases:
- myopia;
- astigmatism;
- hypermetropia.
Anterior chamber implants
implanted in people with significant contraindications to laser correction. The use of LPO significantly simplifies the surgical technique; some types can cause complications. Anterior chamber lenses are made of polymethyl methacrylate and have a service life of about 100 years.
Posterior capsular IOLs
Use only when the lens is completely removed. They are implanted into a capsule. STAAR is the only company that produces substitutes that meet international requirements.
Pupil lenses
available for secondary installation. For installation, use an injector, a cartridge, inserting it through an incision. Implants have a lot of disadvantages, such as instability and a tendency to move. They do not create pressure on the cornea.
Toric implants
combine the advantages of cylindrical and spherical varieties. Such lenses are installed for cataracts, astigmatism, all kinds of corneal pathologies and other diseases. Toric lens substitutes are contraindicated in severe diabetes mellitus, iritis, iridocyclitis, and siderosis.
Posterior chamber implants
used in 90% of ophthalmic surgeries. They are notable for the fewer side effects they cause. Lenses of this type are visually invisible to an outsider and imperceptible to the patient. It can be installed after removing the natural nucleus into the lens bag, the posterior chamber. IOL prevents retinal detachment and glaucoma.
The choice of a specific type of lens is based on the type of pathology, research results, the condition of the cornea, and the financial capabilities of the patient.
All lens substitutes are divided into groups:
- Spherical, aspherical.
The latter type guarantees a contrast image, a wide viewing angle, and no glare. - Monofocal, multifocal.
The latter ensure normal focusing of vision and correct presbyopia. There are toric varieties for the correction of astigmatism. - Accommodating.
A pair of parallel lenses that move due to muscle tension, changing the distance to the focal point. - With protective functions they are the most expensive and protect against ultraviolet rays.
They come in yellow or blue. The choice of one or the other does not affect the perception of the color scheme.
{banner_horizontalnyy2}
DISEASES OF THE OPTIC NERVE AND VISUAL PATHWAY (H46-H48)
H46 Optic neuritis
Optic(ies): • neuropathy other than ischemic • papillitis Retrobulbar neuritis NOS Excludes: ischemic optic neuropathy ( H47.0 ) optic neuromyelitis [Devika] ( G36.0 )
H47 Other diseases of the optic [2nd] nerve and visual pathways
H47.0 Diseases of the optic nerve, not elsewhere classified Compression of the optic nerve. Hemorrhage into the optic nerve sheath. Ischemic optic neuropathy H47.1 Papilledema, unspecified H47.2 Optic nerve atrophy. Pallor of the temporal half of the optic nerve head H47.3 Other diseases of the optic nerve head Growth on the optic nerve head. False papilledema H47.4 Lesions of the optic chiasm H47.5 Lesions of other parts of the visual pathways Diseases of the optic tract, geniculate nucleus and optic radiation area H47.6 Lesions of the visual cortical area H47.7 Diseases of the visual pathways, unspecified
H48* Disorders of the optic [2nd] nerve and visual pathways in diseases classified elsewhere
H48.0 * Optic nerve atrophy in diseases classified in other headings Optic nerve atrophy in late syphilis ( A52.1 +) H48.1 * Retrobulbar neuritis in diseases classified in other headings Retrobulbar neuritis in: • late syphilis ( A52. 1 +) • meningococcal infection ( A39.8 +) • multiple sclerosis ( G35 +) H48.8 * Other lesions of the optic nerve and visual pathways in diseases classified elsewhere
Are there any complications?
Like any medical procedure, pseudophakia can be accompanied by health complications and abnormalities. The most common problem that patients face after surgery is deterioration in visual acuity in the second eye. If similar symptoms are observed, it is recommended to perform a second operation to insert an implant into the second eye.
| Deviations can be caused by an incorrectly installed lens or an incorrectly selected artificial lens. In this case, you should immediately contact an ophthalmologist. |
If after pseudophakia vision improved, but after some time the signs of pathology returned again, and the eye began to see worse, most likely a protein film has formed on it. It does not pose a threat to health or life; you just need to clean the implant. Also, the operated patient may encounter problems such as:
- Keratitis;
- Secondary glaucoma;
- Formation of adhesions in the chamber of the eye;
- Lens falls out.
DISEASES OF THE EYE MUSCLES, DISORDERS OF CONSOLIDATED EYE MOVEMENT, ACCOMMODATION AND REFRACTION (H49-H52)
Excludes: nystagmus and other involuntary eye movements ( H55 )
H49 Paralytic strabismus
Excludes: ophthalmoplegia: • internal ( H52.5 ) • intranuclear ( H51.2 ) • supranuclear progressive ( G23.1 ) H49.0 3rd [oculomotor] nerve palsy H49.1 4th [trochlear] nerve palsy H49. 2 Palsy of the 6th [abducens] nerve H49.3 Complete (external) ophthalmoplegia H49.4 Progressive external ophthalmoplegia H49.8 Other paralytic strabismus. External ophthalmoplegia NOS. Kearns-Sayre syndrome H49.9 Paralytic strabismus, unspecified
H50 Other forms of strabismus
H50.0 Convergent concomitant strabismus. Esotropia (alternating) (monocular), except intermittent H50.1 Concomitant divergent strabismus. Exotropia (alternating) (monocular), except intermittent H50.2 Vertical strabismus H50.3 Intermittent heterotropia Intermittent: • esotropia } • exotropia } alternating (monocular) H50.4 Other and unspecified heterotropia. Concomitant strabismus NOS Cyclotropia. Hypertropia. Hypotropia. Microtropia. Monofixation syndrome H50.5 Heterophoria. Alternating heterophoria. Esophoria. Exophoria H50.6 Mechanical strabismus. Brown's capsule syndrome. Strabismus due to adhesions Traumatic limitation of elasticity of the eye muscle H50.8 Other specified types of strabismus. Duane's syndrome H50.9 Strabismus, unspecified
H51 Other concomitant eye movement disorders
H51.0 Gaze palsy H51.1 Convergence insufficiency [convergence insufficient and excessive] H51.2 Intranuclear ophthalmoplegia H51.8 Other specified concomitant eye movement disorder H51.9 Concomitant eye movement disorder, unspecified
H52 Impairments of refraction and accommodation
H52.0 Hypermetropia H52.1 Myopia Excludes: malignant myopia ( H44.2 ) H52.2 Astigmatism H52.3 Anisometropia and aniseikonia H52.4 Presbyopia H52.5 Disorders of accommodation Internal ophthalmoplegia (complete) (total) Paresis } Spasm } accommodation H52 .6 Other refractive errors H52.7 Refractive error, unspecified
VISUAL DISORDERS AND BLINDNESS (H53-H54)
H53 Visual impairment
H53.0 Amblyopia due to anopsia Amblyopia caused by: • anisometropia • visual deprivation • strabismus H53.1 Subjective visual disorders Asthenopia. Day blindness. Hemeralopia. Metamorphopsia. Photophobia. Atrial scotoma. Sudden loss of vision Visual iris rings Excludes: visual hallucinations ( R44.1 ) H53.2 Diplopia. Image doubling H53.3 Other disturbances of binocular vision. Retinal image inconsistency Image fusion due to stereoscopic defect. Simultaneous visual perception without image fusion Depression of binocular vision H53.4 Visual field defects. Extended blind spot. Generalized narrowing of the visual field Hemionopsia (opposite) (same name). Quadrant anopsia Scotoma: • arcuate • Bjerrum • central • ring-shaped H53.5 Anomalies of color vision. Achromatopsia. Acquired color vision deficiency. Color blindness Deuteranomaly. Deuteranopia. Protanomaly. Protanopia. Tritanomaly. Tritanopia Excludes: day blindness ( H53.1 ) H53.6 Night blindness
Excluded: due to vitamin A deficiency ( E50.5 )
H53.8 Other visual disturbances
H53.9 Visual impairment, unspecified
H54 Blindness and decreased vision
Note • For categories of visual impairment, see the following table. Excludes: transient blindness ( G45.3 ) H54.0 Blindness in both eyes. Visual impairment category 3, 4, 5 in both eyes H54.1 Blindness in one eye, reduced vision in the other eye Visual impairment category 3, 4, 5 in one eye and category 1 or 2 in the other eye H54.2 Reduced vision in both eyes. Category 1 or 2 visual impairment in both eyes H54.3 Unspecified loss of vision in both eyes. Visual impairment category 9 in both eyes H54.4 Blindness in one eye. Visual impairment categories 3, 4, 5 in one eye [normal visual acuity in the other eye] H54.5 Reduced vision in one eye. Category 1 or 2 visual impairment in one eye [normal visual acuity in the other eye] H54.6 Unspecified loss of vision in one eye. Category 9 visual impairment in one eye [normal visual acuity in the other eye] H54.7 Unspecified vision loss. Visual impairment category 9 NOS Note • The following table shows the classification of the degree of visual impairment recommended by the WHO Scientific Group on the Prevention of Blindness, Geneva, 6-10 November 1972 ( WHO Technical Report Series, N51 8, 1974). The term “low vision” in H54 covers categories 1 and 2 of the table, the term “blindness” covers categories 3, 4 and 5, and the term “unspecified vision loss” covers category 9. If the limits of the visual field are also taken into account, patients with a visual field of no more than 10 degrees, but more than 5 degrees around the central visual axis, should be classified as category 3, and patients with a visual field of no more than 5 degrees around the central axis should be classified as category 4, even if central visual acuity is not broken.
Category Visual acuity with the best possible correction of visual impairment maximum value minimum value less than equal to or more than 1 6/18 6/60 3/10 (0.3) 1/10 (0.1) 20/70 20/200
2 6/60 3/60 1/10 (0,1) 1/20 (0,5) 20/200 20/400
3 3/60 1/60 (counting fingers at a distance of 1 m) 1/20 (0.05) 1/50 (0.02) 20/400 5/300 (20/1200)
4 1/60 (counting fingers at a distance of 1 m) Light perception 1/50 (0.02) 5/300 5 No light perception 9 Unspecified or unspecified
Advantages of the method
Compared to other methods of restoring visual acuity, pseudophakia has a number of undeniable advantages:
- No additional adjustments are required after the operation. The patient may forget about glasses and contact lenses;
- The implantation does not affect visual vision in any way; it remains at the same level;
- All objects acquire a clear and regular outline and are located at the distance at which you see them;
- All visual fields are preserved.
The operation is not very complicated and lasts approximately one hour and is performed under local anesthesia.
OTHER DISEASES OF THE EYE AND ITS ACCIDENTAL APPARATUS (H55-H59)
H55 Nystagmus and other involuntary eye movements
Nystagmus: • NOS • congenital • as a result of visual deprivation • dissociated • latent
H57 Other diseases of the eye and its adnexa
H57.0 Abnormalities of pupillary function H57.1 Eye pain H57.8 Other unspecified diseases of the eye and adnexa H57.9 Disorder of the eye and adnexa, unspecified
H58* Other lesions of the eye and its adnexa in diseases classified elsewhere
H58.0 * Abnormalities of pupillary function in diseases classified elsewhere Argyll Robertson syphilitic phenomenon or pupil ( A52.1 +) H58.1 * Visual impairment in diseases classified elsewhere H58.8 * Other disorders of the eye and its appendages apparatus for diseases classified in other headings Syphilitic oculopathy NCDR: • congenital • early ( A50.0 +) • late ( A50.3 +) • early (secondary) ( A51.4 +) • late ( A52.7 +)
H59 Lesions of the eye and its adnexa after medical procedures
Excludes: mechanical complication from: • intraocular lens ( T85.2 ) • other ocular prosthetic devices, implant and graft ( T85.3 ) pseudophakia ( Z96.1 ) H59.0 Vitreous syndrome after cataract surgery H59.8 Other lesions of the eye and its adnexa after medical procedures Chorioretinal scars after surgery for retinal detachment H59.9 Damage to the eye and its adnexa after medical procedures, unspecified
Treatment
Aphakia is corrected using glasses, contact and intraocular lenses. The indication for spectacle vision correction is a bilateral form of the disease. For unilateral aphakia, glasses are recommended only if contact methods of correction are intolerant. The choice of glass for an emmetropic eye is difficult, because even glass of +10 diopters is not comparable to the refractive power of the lens, which is 19 diopters. This is due to the fact that the refractive index of the liquid that surrounds the lens is higher than that of the air surrounding the glass. The optical power of a glass lens depends on the patient's refraction. For hyperopia, it is necessary to choose glasses with stronger optics than for myopia. There is no need to prescribe vision correction methods to patients with high degrees of myopia before lens removal. Due to the lack of accommodation ability, the patient should be prescribed glasses for near vision that are 3.0 diopters stronger than for distance vision. Contact or intraocular vision correction is indicated for patients with monocular aphakia. Prescribing glasses to patients with this form of the disease will worsen aniseikonia. During surgery (intraocular correction), an artificial lens with individually selected optical power is implanted. The most preferred treatment option is the use of posterior chamber lenses, as they are localized at the location of the natural lens and provide high quality vision. Congenital aphakia can be corrected using this technique only after the child reaches two years of age.