Chlamydial conjunctivitis is an infectious disease characterized by damage to the eye mucosa by chlamydia. The infection provokes acute or chronic inflammation of the conjunctiva. Chlamydial conjunctivitis is characterized by swelling of the mucous membrane, pain, lacrimation, purulent discharge and follicular rashes. This is a serious disease that is difficult to recognize and treat.
The nature of chlamydia
There are fifteen species of the intracellular parasite Chlamydia trachomatis that infects humans. Due to some characteristics, it occupies an intermediate position between bacteria and viruses, which makes it difficult to diagnose and treat the conditions it causes.
Chlamydia is a pathogenic gram-negative bacteria. Chlamydia differs from other bacteria in its unique intracellular development cycle. They act on the principle of intracellular parasites. During primary infection, cells of the main barrier systems are affected.
At the initial stage of development, chlamydia attaches to sensitive cells of the mucosa, epithelium, leukocytes, monocytes and macrophages. The parasite's shell fuses with the cell membrane, and chlamydia penetrates the cytoplasm. At this time, infectivity cannot be detected. The parasite is infectious only after it has emerged from latency. After this period ends, infectivity begins to rise.
The effect of chlamydia on the organs of vision
Chlamydial conjunctivitis is also called ophthalmochlamydia or ocular chlamydia. This type of disease is diagnosed in 3-30% of cases of conjunctivitis, mainly in women 20-30 years old. As a rule, chlamydial conjunctivitis is a complication of urogenital chlamydia.
Forms of chlamydial conjunctivitis:
- trachoma;
- paratrachoma (adult conjunctivitis);
- blenorrhea (conjunctivitis of newborns);
- pool;
- epidemic;
- conjunctivitis due to Reiter's disease;
- meibomitis (zoonotic nature of conjunctivitis).
Ophthalmologists also distinguish chlamydial keratitis, uveitis, episcleritis and other types of the disease. These diseases can develop for a long time without symptoms and not bother a person in any way.
Causes of chlamydia in the eyes
Chlamydia can parasitize inside cells for a long time in an inactive state, acquiring the L-form. Under favorable conditions, chlamydia reverses from the L-form and begins to actively multiply, provoking the appearance of characteristic symptoms. The transition of chlamydia from an inactive form to an active one occurs during suppression of the immune system (during ARVI, during hypothermia, treatment with antibiotics).
There are several antigenic serotypes of chlamydia. Each of them causes different lesions. Serotypes A, B, Ba and C provoke the development of trachoma (chronic inflammation of the eye mucosa). “Genital” varieties D, E, F, G, H, I, Y and K cause adult paratrachoma (damage to the conjunctiva and genitourinary tract), epidemic chlamydial conjunctivitis and urogenital chlamydia. Serotypes L1 and L3 are the cause of the development of inguinal lymphogranulomatosis.
Chlamydial conjunctivitis, as a rule, develops against the background of chlamydia in the genitourinary system. About half of patients with ocular chlamydia also suffer from the urogenital form. In adults, chlamydia develops in the visual system due to the pathogen entering the eye through hygiene items and hands contaminated with secretions from the genitals. Sometimes chlamydial conjunctivitis develops after oral-genital sexual contact with an infected person.
At risk:
- sexually active people;
- patients with urogenital chlamydia and their sexual partners;
- family members of a patient with chlamydia;
- people with acute conjunctivitis, especially if the disease affects only one eye;
- people with recurrent conjunctivitis that is difficult to treat;
- visitors to swimming pools, saunas and baths;
- newborn children whose mothers have chlamydia.
The cause of chlamydial conjunctivitis in infants is intrauterine infection or infection during childbirth. Eye damage from chlamydia occurs in 5-10% of children immediately after birth.
Occupational infection with chlamydia is possible among obstetricians, gynecologists, venereologists, urologists, andrologists and ophthalmologists. You can become infected with chlamydia in a public pool or bathhouse through water. This form of conjunctivitis is called bath or pool conjunctivitis; it usually has the character of an epidemic outbreak.
Sometimes ocular chlamydia develops with Reiter's syndrome. This is an autoimmune disease that manifests itself in damage to the urogenital tract, joints and mucous membranes of the eye. These disorders can develop simultaneously or sequentially. The pathogenesis of ocular chlamydia in Reiter's syndrome has not been sufficiently studied.
Symptoms of chlamydial conjunctivitis
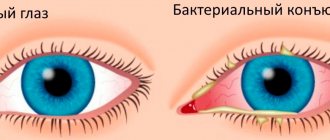
The first clinical manifestations of ocular chlamydia are observed 5-14 days after infection. This disease is characterized by damage to one eye first, and only 30% of patients have bilateral infection.
The chronic form is observed in 35% of patients. It is characterized by recurrent but sluggish conjunctivitis and blepharitis with moderate symptoms. There is slight swelling of the eyelids, redness of the conjunctiva and mucous discharge.
The acute phase of ocular chlamydia lasts from 2 weeks to 3 months. Most patients are diagnosed with an acute or subacute form of ocular chlamydia. Acute conjunctivitis and exacerbation of chronic conjunctivitis are accompanied by severe swelling, infiltration of the mucous membrane, pain, lacrimation, photophobia, copious mucopurulent or purulent discharge that sticks the eyelids together.
Characteristic symptoms of acute chlamydial conjunctivitis are regional preauricular adenopathy and eustachitis with pain and hearing loss. During the examination, the doctor identifies many follicles and fibrinous films.
In infants, in addition to eye symptoms, it is possible to develop chlamydial pneumonia, rhinitis, nasopharyngitis, otitis, and eustachitis. At an early age, the disease is dangerous due to stenosis of the nasolacrimal ducts and scarring of the conjunctiva. Symptoms of ocular chlamydia in Reiter's disease can include keratitis, conjunctivitis, iridocyclitis, choroiditis and retinitis.
Clinical manifestations
The symptoms of chlamydial conjunctivitis depend on the form in which it occurs. But they often appear at later stages of progression of the pathological process. If it has just begun, the disease can be latent, that is, completely asymptomatic.
The incubation period for the development of chlamydial conjunctivitis lasts from 6 to 14 days. Often one visual organ is affected first, but if the first signs of the pathological process are ignored, the disease can spread to the second.
Symptoms of acute chlamydial conjunctivitis can manifest themselves due to the occurrence of:
- swelling of the conjunctival sac;
- hyperemia of the eyeball;
- increased lacrimation;
- photophobia;
- swelling of the mucous membranes of the eyes;
- pain and pain in the eyes;
- discharge of sticky (purulent) eye secretion.
At later stages of development, chlamydial conjunctivitis can cause the development of eustachitis, as well as lead to hearing loss and the occurrence of noise and ringing in the ears.
The chronic form of the pathological process is considered sluggish due to the mild severity of its symptoms. However, it is no less dangerous, so treatment is necessary in any case.
How is chlamydial conjunctivitis diagnosed?
Since ocular chlamydia is infectious in nature, in addition to standard ophthalmological methods, laboratory tests are also used. Often, ophthalmologists prescribe additional consultations with a venereologist, urologist, gynecologist, otolaryngologist and even rheumatologist.
Methods for diagnosing chlamydial conjunctivitis:
- biomicroscopy (shows swelling, infiltration and new vessels of the limbus);
- ophthalmoscopy (checking the condition of the retina);
- linked immunosorbent assay;
- cytological analysis;
- PCR diagnostics;
- immunofluorescein test (helps to exclude corneal damage);
- cultural analysis.
For chlamydial conjunctivitis, it is recommended to combine different laboratory methods for examining scrapings from the conjunctiva. To be on the safe side, an examination for urogenital chlamydia is prescribed. Differential diagnosis is carried out to exclude bacterial and adenoviral conjunctivitis.
Diagnostics plays an important role in the treatment of chlamydial conjunctivitis, since it is necessary not only to identify the pathogens, but also to determine their sensitivity to antibiotics. After the first antibiotic therapy, chlamydia can survive and develop immunity to the drugs.
Diagnostics
If you suspect the presence of chlamydia in the eyes, you should contact an ophthalmologist, who will prescribe special tests and refer you for examination to other specialists: venereologist, gynecologist, urologist, otolaryngologist, rheumatologist.
Diagnosis of ophthalmochlamydia is based on a number of methods that combine visual examination of the eyes, medical history and special laboratory tests. This is the only way to guarantee an accurate diagnosis. At the present stage of development of medicine, there are several laboratory methods for diagnosing paratrachoma:
- Polymerase chain reaction. This method is characterized by short implementation times, a small amount of test material and a high degree of sensitivity - up to 100%. PCR is recommended as the preferred method for making and confirming the diagnosis of chlamydial conjunctivitis.
- Linked immunosorbent assay. This method involves the determination of antibodies (IgG, IgM, IgA) to chlamydia in the blood. The study not only identifies the causative agent of the disease, but also determines in what form ocular chlamydia occurs - acute or chronic. However, this type of diagnosis also has significant drawbacks: analysis is possible only 10–15 days after infection, when the first antibodies are produced, and its accuracy does not exceed 60%.
- Culture for chlamydia. Of all diagnostic methods, this is the most expensive and time-consuming - results have to be waited for several days. But the main advantage of the cultural method is that it also shows the sensitivity of the pathogen to a particular group of antibiotics.
- Cytology or microscopic analysis. A general smear in men is taken from the urethra, and in women, material from the vagina, urethra and cervix is simultaneously used. The method is one of the oldest, therefore it is not highly effective - the probability of determining a chlamydial infection in this way does not exceed 15%. This study can only detect the presence of an inflammatory process, which implies the need for further diagnosis.
- Immunofluorescence. During diagnosis, material from the urethra or cervical canal is stained with a special substance and then examined under a fluorescent microscope. The accuracy of this method is about 50%, and the time required does not exceed one hour. However, this method is characterized by high subjectivity in assessing the result, which significantly reduces its diagnostic value.
All tests and examinations help differentiate ocular chlamydia from other types of conjunctivitis. The outcome of treatment and the health of the patient depend on the correct diagnosis.
Differential diagnosis of different types of conjunctivitis - table
| Sign | Bacterial conjunctivitis | Adenoviral conjunctivitis | Herpesvirus conjunctivitis | Chlamydial conjunctivitis | Fungal conjunctivitis | Allergic conjunctivitis |
| Pathogen | The most common:
| Adenoviruses | Herpes simplex virus | Chlamydia | Various types of fungi:
| Allergens:
|
| General state | Norm | Possible combination with ARVI | Possible combination with ARVI | Norm | Norm |
|
| Seasonality | Not typical | Epidemic outbreaks | Not typical | Not typical | Not typical | Characteristic (depending on the allergen) |
| Flow |
| Acute |
|
| Chronic | Drug:
Pollinose:
Large papillary: chronic. |
| Fellow eye involvement | + | + | — | — | + | + |
| Main complaints |
|
|
|
|
|
|
| Character of the discharge |
|
| There is no separation | Mucopurulent discharge or its absence |
| Mucous “stringy” discharge |
| Clinical signs |
|
| Herpetic vesicles are fluid-filled blisters (on the skin of the eyelids and wings of the nose) |
|
|
|
Antibiotics for chlamydia of the eye
Chlamydia are intracellular parasites, so it is necessary to take antibiotics with etiotropic action. Chlamydia of the eye requires the prescription of tetracycline antibiotics, fluoroquinolones and macrolides. These drugs act directly on the cause of conjunctivitis. The choice of drug should be made by a doctor, taking into account the characteristics of chlamydial conjunctivitis in a particular patient, concomitant diseases, pregnancy and other factors.
The dosage of antibiotics and duration of therapy must be determined taking into account the severity of the disease. Systemic drugs are prescribed for a period of 7 to 21 days. It is recommended to choose drugs in tablets or injection solutions. Doxycycline (Vibramycin, Unidox) is commonly used to treat chlamydia. For acute damage, you need to take the medicine for two weeks, and for chronic damage, for a month. Additionally, erythromycin and azithromycin are prescribed.
Based on the results of laboratory tests, the following drugs may be prescribed:
- Ofloxacin;
- Ciprofloxacin;
- Clarithromycin;
- Tetracycline;
- Spiramycin;
- Vilprafen.
Chlamydia quickly develops resistance to mild antibiotics, making it difficult to treat the disease in the future. Eye drops and ointments should only be used as supportive therapy. The mainstay of treatment for ocular chlamydia is systemic medications.
Typically, a treatment regimen for sexually transmitted infections is used. Treatment for chlamydia takes more than 3 weeks. This is due to the fact that only during a certain period of its development chlamydia is sensitive to antibiotics. Such long-term therapy allows you to cover several cycles of their development and is guaranteed to cure ophthalmochlamydia.
Self-medication of chlamydial conjunctivitis can be dangerous. Uncontrolled use of antibiotics leads to persistent infection, that is, chlamydia remains active even after the period characteristic of the acute phase. This complicates the diagnosis and treatment of chlamydia. In addition, addiction to antibiotics is fraught with dysbacteriosis and liver overload. In women, dysbiosis can begin not only in the intestines, but also in the vagina, weakening protection against other infections.
Symptoms
The incubation period of the disease is from 5 days to 2 weeks. The primary manifestations of the disease are:
- redness of the conjunctiva, and sometimes the whites of the eyes;
- swelling of the eyelids;
- increased lacrimation;
- the appearance of mucous discharge from the eyes;
- burning in the eyes.
Later the symptoms increase:
- The mucous secretions are already developing into films that literally stick the eyelids together.
- Dense infiltrates appear in the tissues of the conjunctiva.
- Purulent secretion appears in very large quantities.
- Pain in the eyes and photophobia appear.
Subsequently, with the development of symptoms, a person observes an enlargement of the lymph node under the jaw, which indicates a further spread of the inflammatory process. By the way, it can transfer to almost any organ or system.
The clinical picture of chlamydial conjunctivitis in children may include manifestations of rhinitis, otitis media and even infectious pneumonia.
Local therapy for chlamydial conjunctivitis
It is also necessary to combat intracellular parasites with the help of antimicrobial drugs, however, exclusively local treatment of chlamydial conjunctivitis is ineffective. Often, when there is inflammation of the eyes, ophthalmologists in city clinics conduct a superficial examination and do not always assume the presence of chlamydia. This leads to the prescription of topical antibiotics, most of which are ineffective against chlamydial conjunctivitis. Improper treatment causes the disease to become chronic and spread to other organs.
It is recommended to combine eye drops and antihistamines. Local therapy for chlamydial conjunctivitis lasts 3-4 weeks. Be sure to use erythromycin and tetracycline ointments, antibacterial drops Ofloxacin and Ciprofloxacin, as well as Norfloxacin and Levofloxacin. To combat inflammation, Indomethacin or Dexamethasone drops are prescribed. The dosage and duration of use of local agents is reduced after 1-2 weeks of treatment.
In some patients, antibacterial drugs cause allergies and even poisoning, so it is additionally recommended to take corticosteroids and agents to improve tissue trophism. These are Hydrocortisone or Dexamethasone, Taufon drops, Oftagel. To prevent fungal complications, drugs with nystatin are prescribed. At the end of therapy, a prescription is issued for drugs to restore microflora (Bifiform, Acylact, Maxilak).
After 2-4 weeks of treatment, repeat studies are carried out. Cure will be indicated by regression of symptoms and negative test results. The tests are repeated three more times at monthly intervals to completely ensure that there is no infection.
If chlamydia is detected in one partner, the other is recommended to undergo testing. It is noteworthy that the treatment regimen for each may differ depending on gender, age, concomitant diseases and the presence of pregnancy.
Treatment of chlamydial conjunctivitis in adults
The basis of therapy is antibiotics:
- macrolides;
- tetracyclines;
- fluoroquinolones.
For local use, installations of antibacterial eye drops (solution of ciprofloxacin or ofloxacin), anti-inflammatory drops (solution of dexamethasone, indomethacin), ointment applications over the eyelids (erythromycin, tretracycline ointment) are prescribed.
Recovery is indicated when the symptoms of the pathology regress and laboratory tests show a negative result. The latter must be taken 2 weeks (maximum one month) after the end of the course of therapy.
HC may pass without or with consequences. If you consult a doctor in a timely manner and treat the pathology correctly, the risk of complications and relapses is minimized. Very often the disease becomes chronic and often recurs. If the pathology occurs very often, scarring of the cornea and conjunctiva may occur, which leads to decreased vision.
Treatment of ocular chlamydia in children
If there is abundant purulent discharge, it is necessary to rinse the conjunctival cavity with a 2% boric acid solution or furatsilin (nitrofural). Picloxidine or sodium colistimethate, Rolitetracycline, Chloramphenicol are applied topically up to 6 times a day, or tetracycline, ofloxacin or erythromycin ointment is applied 4-5 times a day.
If there is severe swelling or irritation, the use of antiallergic drops twice a day is justified. It is possible to combine Antazol with Tetrizoline, Naphazoline and Diphenhydramine, or use Olopatadine.
Folk remedies for conjunctivitis
Doctors question traditional methods of treating chlamydial conjunctivitis, since the causative agent of the disease is viable. Folk remedies can be included in the treatment of ocular chlamydia only with the approval of an ophthalmologist. They help strengthen the immune system and reduce the symptoms of inflammation. You can cleanse the eyes of purulent discharge using herbal decoctions.
Infusions and decoctions for washing the eyes for conjunctivitis:
- Chamomile officinalis. Take 2-3 tablespoons of chamomile per liter of boiling water and leave for an hour. The tincture should be filtered before use. You can wash your eyes with this product several times a day.
- Plantain. Take 2 teaspoons of ground plantain seeds per glass of hot water and leave for 30 minutes. The resulting product can be used to wash your eyes or make lotions.
- Elderberry, cornflower, toadflax. You need to take a tablespoon of each ingredient for 2 cups of boiling water. For complete readiness, the product should be infused for 8-10 hours.
- Hop cones, blueberry leaves. Add a tablespoon of ingredients to a glass of hot water and leave for an hour. The infusion is drunk three times a day, three sips 30 minutes before meals.
- Propolis. First, propolis is ground to a powder and filled with water (1:5). After filtration, the product is used as drops 2-3 times a day.
- Tea. You can wash your eyes to remove pus from conjunctivitis with weak black or green tea.
To eliminate inflammation, it is allowed to make lotions with tincture of calendula, chamomile or oregano. During treatment, you must give up alcohol, sweets, fatty and salty foods. You should increase the amount of vegetables, whole grain cereals and dairy products in your diet.
The first experience of using Floxal for the treatment of chlamydial conjunctivitis
for the chlamydial conjunctivitis Yu.S. Astakhov, IA Olisova, GN Loginov The study of clinical efficacy and tolerability of Floxal 0.3% eye drops was performed in 17 patients (age 18–32 years). All patients had the diagnosis of chlamydial conjunctivitis: 8 – acute and 9 – chronic. The treatment was carried out during 4–5 weeks. There was shown good tolerability and high efficacy of Floxal. Floxal could be recommended to the treatment for the chlamydial conjunctivitis. Currently, fluorinated quinolones have formed a large group of broad-spectrum antimicrobial drugs. These drugs are effective against gram-negative and gram-positive aerobic bacteria and pathogens with intracellular localization - chlamydia, mycoplasma, legionella. In general medical practice, the most studied drug from the group of fluoroquinolones is ofloxacin. According to foreign literature, the drug ofloxacin in the form of eye drops has been widely used in ophthalmology for the treatment of acute bacterial conjunctivitis and corneal ulcers since the late 1980s (J.P. Monk, D.M. Campoli-Richards, 1987; Tabbara KF et al ., 1999). In our country, ofloxacin (Floxal, manufactured by Bausch & Lomb) began to be used in ophthalmic practice relatively recently, and we have the first experience of its use. Inflammatory eye diseases and their treatment are an important social problem in practical ophthalmology throughout the world. The first place among inflammatory diseases of the anterior segment of the eyes is occupied by conjunctivitis - 66.7% (Maichuk Yu.F., 1995). In the last 10 years in Russia, as in most industrialized countries, the problem of chlamydial inflammation of the conjunctiva has become increasingly significant. According to statistics from the Moscow Research Institute of GB named after. Helmholtz, chlamydial conjunctivitis accounts for 10–14% of all inflammations of the mucous membrane of the eyes (Maichuk Yu.F. et al. 1990; Maichuk Yu.F., Vakhova E.S., 1993). In St. Petersburg, the proportion of paratrachoma is 15–19% among all conjunctivitis (Astakhov Yu.S., Olisova I.A., 2001). For the treatment of conjunctivitis of chlamydial etiology, we used the drug Floxal eye drops (0.3% ofloxacin) manufactured by Bausch & Lomb, Germany. Purpose of the work: to evaluate the effectiveness and safety of Floxal in the treatment of chlamydial conjunctivitis. Materials and methods A total of 17 patients aged from 18 to 32 years were treated. (11 men and 6 women). Of these patients, 8 were diagnosed with acute and 9 with chronic chlamydial conjunctivitis. Diagnostics, in addition to routine ophthalmological methods (determining visual acuity, biomicroscopy), included a direct immunofluorescence reaction, culture of McCoy cells, and a cytological method with Romanovsky staining. The collection of scrapings from the conjunctiva of the eyelids for a comprehensive laboratory examination was carried out using disposable Accelon Multi sampling probes (Astakhov Yu.S., Olisova I.A., 2000). Depending on the severity of the inflammatory process, Floxal was prescribed from 3 to 6 times a day in each eye. As the inflammation subsided, the frequency of instillations decreased. For acute chlamydial conjunctivitis, Floxal was used 6 times a day for the first 7 days, then 4 times a day for 2 weeks. From the third week, instillations of 0.1% dexamethasone drops 3 times a day were additionally prescribed. Antihistamine eye drops were used during the first week of illness. As a rule, the drug spersallerg was used. Instillations of spersallerg were prescribed 2–4 times a day, depending on the severity of the inflammatory process. In cases of chronic paratrachoma, Floxal was used 3–4 times a day in the 1st week, then, as the inflammatory process subsided, the frequency of instillations was reduced to 2–3 times a day. Just as with acute paratrachoma, from the 3rd week drops of 0.1% dexamethasone were prescribed 2 times a day. During treatment, all patients were observed on an outpatient basis, the conjunctiva of the eyelids and eyeball, the cornea were examined, and an intermediate laboratory examination of patients was carried out using a direct immunofluorescence reaction to study the therapeutic effectiveness of the therapy (on the 6th and 14th days of treatment and after the end of therapy). Local treatment of acute and chronic paratrachoma continued until chlamydial antigen was detected in scrapings from the conjunctiva. The final assessment of the effect of the drug for the treatment of paratrachoma was carried out according to the following characteristics: not effective, moderately effective, good, excellent. The criteria for assessing therapeutic effectiveness included: terms of subjective and objective (reduction of hyperemia and edema of the conjunctiva, terms of resorption of infiltration and follicles of the conjunctiva, improvement in the condition of the upper limbus and cornea) recovery. When analyzing the tolerability of the drug, we took into account that the appearance or intensification of a toxic-allergic reaction may be associated with the use of other drugs, and the increase in inflammatory phenomena may be associated with a complication of the underlying disease (paratrachoma). If adverse events occurred, we graded them according to severity: mild (symptom easily tolerated), moderate (impairment of daily activities), severe (impossibility of daily activities). All patients were prescribed systemic antibiotic therapy simultaneously with local antibiotic therapy. Ofloxacin 200 mg 2 times a day was used for 10 days. Results Treatment of patients with acute chlamydial conjunctivitis lasted an average of 4 weeks, and with chronic paratrachoma - 5 weeks (this increase is most likely due to the use of inadequate local therapy previously prescribed in other medical institutions). In cases of acute paratrachoma, when treated with Floxal, conjunctival hyperemia decreased on average in 4 days, resorption of conjunctival infiltration occurred in 14 days, follicles in 25–30 days, and corneal and limbal infiltrates in 14–17 days. Recovery was confirmed not only by subjective and objective improvement, but also by the absence of chlamydia antigens in scrapings from the conjunctiva. All patients tolerated treatment with Floxal well, and none of them reported adverse events during treatment.
Conclusions Floxal is an effective drug in the treatment of chlamydial conjunctivitis, and it can be recommended for the treatment of chlamydial conjunctivitis of varying severity. Floxal is well tolerated by patients even with long-term use.
Prognosis and prevention
The consequences of chlamydia in the eyes vary. With timely consultation with a doctor and proper treatment, the disease can be cured completely, but chlamydial conjunctivitis often recurs. The recurrent form is dangerous due to scarring of the conjunctiva and cornea, which is a common cause of visual impairment.
Prevention of ophthalmochlamydia lies in timely detection and complete treatment of urogenital chlamydia. It is important to observe the rules of personal hygiene. When visiting the pool, you need to protect your eyes with special goggles. Women should only use their own cosmetics. It is prohibited to exchange underwear and try it on a naked body in stores.
When planning a pregnancy, it is important to undergo a complete examination. This need is due to the fact that pregnant women cannot use antibacterial drugs that are prescribed to combat chlamydia. In addition, intracellular parasites can affect the development of the child.
Chlamydia of the eye is a dangerous disease that is difficult to treat. Only complete diagnosis and long-term therapy help get rid of chlamydia and prevent relapse of the disease. Local treatment for eye damage from chlamydia is ineffective; a systemic effect on the body is required.
Sources used:
- New standards for providing ophthalmological care on an outpatient basis. Textbook / A.N. Amirov, R.N. Tokinova, E.I. Mingazova. — M.: Smart Doctor, 2015.
- Atlas of ophthalmology / G.K. Kriglstein et al. - M.: Medical Information Agency, 2009.
- Dry eye syndrome and ocular surface diseases. Clinic, diagnosis, treatment / V.V. Brzhesky, G.B. Egorova, E.A. Egorov. - M.: GEOTAR-Media, 2021.
- FSBI "National Medical Research Center GB named after. Helmholtz" of the Ministry of Health of Russia
Prevention
To avoid infection with this parasite, it is advisable to take timely precautions. To do this, you should follow simple rules:
- Strengthen the body's defense mechanisms;
- Always keep your hands clean;
- Refuse to rub your eyes with your hands;
- Do not use other people's cosmetics or intimate household items;
- Use only personal hygiene products and medical supplies;
- Have sexual intercourse only with a regular partner;
- Use contraception;
- Check for chlamydia.
Prevention measures require timely detection and treatment, ensuring safety when visiting medical institutions, and ensuring eye protection while swimming with goggles.