In ophthalmology, the most dangerous disease is ocular retinoblastoma (RB), a malignant tumor that affects the inner lining of the eye. This disease was discovered in 1926. Scientist Verlhof discovered that the neoplasm is formed from retinoblasts - cells that form the retina in the prenatal period. However, if a malfunction occurs in the process, the cells begin to rapidly divide and give rise to a tumor.
The diagnosis of retinoblastoma is made mainly in childhood. The main danger of the disease is that the initial stage is practically asymptomatic. This leads to serious consequences, including loss of vision and removal of the affected eyeball.
To avoid this, you should know how the disease manifests itself at the very beginning, what its causes are, and how it can be diagnosed. After all, a timely diagnosis in 95% of cases helps to completely cure the child, preserving his vision.
Causes of pathology
The development of retinal cancer is in most cases hereditary. It is based on a mutation at the gene level. The RB1 protein prevents cells from dividing excessively, but at some point it becomes inactive. Subsequently, the defective gene is passed on from generation to generation, which is the cause of the development of retinoblastoma.
Most cases of bilateral eye cancer are hereditary. The diagnosis is made before the age of 2.5 years, and the presence of the mutated gene is confirmed in 90% of cases. The first symptoms of the disease can be noticed already in the first year of a child’s life. A congenital tumor can lead to the development of glaucoma.
There is a sporadic (non-hereditary) form of retinoblastoma, which occurs due to random glitches in the gene program and mutations. It is detected in adolescence. Provoking factors are the late age of parents, their employment in hazardous industries, and unfavorable ecology. This pathology of the retina is unilateral and develops locally.
In adults, cancer of this form is extremely rare, and its causes remain unidentified.
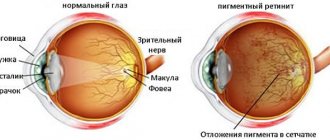
Causes of retinal dystrophy
Experts attribute the following factors to the reasons for the development of retinal dystrophy:
- Disruption of the ocular vascular system. This pathology causes patients to begin a scarring process in their retina;
- Impaired immune system function can also lead to the onset of scarring of the layers of the retina;
- Unbalanced diet. Many doctors believe that retinal dystrophy can develop due to the consumption of low-quality foods and poor diet;
- Tobacco smoking negatively affects all internal organs and systems of the human body, but the organs of vision, in particular the retina, are especially affected by nicotine;
- Systematic consumption of alcoholic beverages can also provoke retinal dystrophy;
- Previous viral infections, during the treatment of which qualified medical care was not received;
- Chronic diseases such as diabetes, heart disease, endocrine system, hypertension;
- Previous eye surgery;
- Disorders of metabolic processes in the human body, which lead to obesity.
Classification of the disease
In ophthalmology, there are several broad classifications of this pathology.
According to the prevalence of the oncological process, the following are distinguished:
- Monocular, which affects only one eye.
- Bilateral (bilateral) is detected on the membranes of both eyes.
By type of growth:
- Endophytic. It spreads to the central part, affecting the orbit of the eye, nerves, and also the macula (the yellow spot in the very center of the retina). The surface of the tumor is lumpy.
- Exophytic. The tumor grows towards the retina. Its further spread leads to an increase in the amount of intraocular fluid, increased intraocular pressure and retinal detachment. In this case, blood vessels can be damaged, hemorrhages occur, which is why the tumor acquires a pinkish tint.
Depending on the size and location of the pathological process, the following stages of retinoblastoma are distinguished:
- the most unfavorable, in which there is a widespread spread of metastases. The disease affects all tissues, nerves, orbit and retina.
- Unfavorable - the process has affected more than 50% of the retina of the eye, and multiple pathological foci are diagnosed on the vitreous body.
- Doubtful - the size of the tumor does not exceed 10 mm (disc diameters), it is located anterior to the ocular equator. Another option is that the diameter of the neoplasm is more than 10 mm, but it is localized posterior to the equator. Here various degrees of protrusion of the eyeball occur.
- Favorable - a lesion measuring 4-10 mm, located behind the equator of the eye.
- The most favorable. The size of the tumor does not exceed 4 mm. Lesions are single or multiple, located behind the equator line of the eye or directly on this line.
Retinoblastoma of the eye in children of stages 1 and 2 of development can extend beyond the eye orbit. Metastases of neuroblastoma first affect regional lymph nodes, then penetrate the brain and spinal cord. It is important to detect an insidious disease in time in the first stages.
Forecast
The prognosis for life depends on a number of factors, including the presence of multiple growth foci, the location of retinoblastoma anterior to the dentate line, the diameter of the node is more than 15 mm, the volume of the lesion exceeds half of the eyeball, the spread of the process into the vitreous substance, optic nerve fibers, and the choroid. When the tumor spreads into the orbit, the risk of metastasis increases to 78%. Risk factors also include family history. With the hereditary form of the disease, mortality increased from 2.9% to 9%, and with the sporadic form it decreased from 1.9% to 1%.
In order to timely detect recurrence of retinoblastoma after enucleation, you should regularly examine the child. If the retinoblastoma was unilateral, then examinations are carried out every three months for two years. For bilateral lesions, the observation period is increased to three years.
In children older than one year, a CT scan of the head is performed every 12 months, which helps to assess the condition of the orbital tissue and exclude metastasis to the brain. Even after treatment, children with retinoblastoma require lifelong clinical monitoring.
Symptoms of the disease
The initial stage occurs quite early - up to 12 months. At this age, the child cannot complain of decreased visual acuity or blindness. In this case, parental attentiveness is extremely important.
The most noticeable external sign is strabismus. This defect should not be ignored; it is better to consult an ophthalmologist. As the tumor enlarges and when bright light hits it, a white pupillary reflex appears (the tumor is visible through the pupil). In medicine, this symptom is called “cat's eye”. The effect is clearly visible in flash photographs.
When inflammation and/or swelling occurs, pain, photophobia appear, and glaucoma develops. As a result of damage to the retina, the eye may stop responding to light, vision becomes cloudy, and blindness may occur.
Next, retinoblastoma destroys the walls of the orbit and extends beyond the eye. Exophthalmos (“bulging” of the eye) of varying severity appears.
In the later stages of eye cancer, when metastases have affected the optic nerve and spread to the brain, migraine attacks, vomiting, nausea appear, and general intoxication develops.
Astrocytoma
Astrocytic hamartoma of the retina - astrocytoma - grows from astrocytes of the sensory part of the retina, often occurs against the background of tuberous sclerosis, which is characterized by neuroectodermal dysplasia (seborrheic adenoma of the facial skin, neurofibromatosis).
The disease is inherited in an autosomal dominant manner. A tumor in the fundus of the eye in tuberous sclerosis was first described in 1921 by I. Van der Hoeva. However, later F. Schwab showed that tumors in the fundus appear in only 20% of patients with tuberous sclerosis. It should be borne in mind that astrocytoma can be represented by a solitary node in the retina in practically healthy individuals of young or childhood.
Clinic
In the fundus, as a rule, a well-circumscribed, round or oval-shaped prominent tumor of a grayish-white or yellowish color is accidentally detected. The tumor is localized both in the central zone, on the optic nerve head, and at the extreme periphery in the area of the sensory retina (Fig. 7.5; 7.6).
Fig. 7.5. Nodular astrocytoma on the periphery of the fundus in a 15-year-old girl
Rice. 7.6. Astrocytoma in the optic disc region in a 7-year-old boy
Astrocytoma lies in the layer of nerve fibers; retinal vessels can pass on its surface and under it. There may be calcifications in the tumor. Its dimensions do not exceed one or two diameters of the optic nerve head, the boundaries are uneven, but quite clear. In young children, cysts may develop in the astrocytoma as they grow older. This makes the tumor look like a mulberry.
When a cyst spontaneously ruptures, its contents spill into the vitreous, which leads to clouding and decreased visual acuity. As a rule, the tumor practically does not progress. However, in young children, the tumor may enlarge, which leads to the appearance of intraretinal and subretinal exudate and decreased visual acuity.
Morphology
The tumor is represented by well-differentiated elongated cells with light eosinophilic cytoplasm and round and oval nuclei.
Fibrillar processes of glial cell bodies form a thick matrix. J.Shields (1984) observed rare mitoses in astrocytoma. The tumor is located in the inner layers of the retina; as its size increases, it may spread to the outer layers. The surface of the tumor is covered with a delicate network of newly formed vessels. The diagnosis is made on the basis of direct, indirect ophthalmoscopy. Biomicroophthalmoscopy provides more information. FA and ultrasound scanning help in diagnosing large tumors. Sometimes the diagnosis of astrocytoma is so difficult that a fine-needle aspiration biopsy ( FNA)
.
Differential diagnosis of astrocytoma is difficult due to the commonality of ophthalmoscopic symptoms with many diseases. First of all, differentiation from retinoblastoma, non-pigmented uveal melanoma, cavernous choroidal hemangioma, and retinal capillary hemangioma is required. chronic retinal granuloma, myelial fibers, optic disc drusen, retinal gliosis.
Treatment
Small, well-circumscribed astrocytomas do not require treatment.
If signs of an increase in formation or retinal detachment appear, limiting laser coagulation or cryopexy is recommended in order to localize the pathological process. The prognosis for vision with small astrocytomas is good. Large tumors accompanied by exudative retinal detachment can lead to decreased vision. The prognosis for life is good.
A.F. Brovkina, V.V. Valsky, G.A. Gusev
Published by Konstantin Mokanov
Diagnosis of eye tumor
An ophthalmologist can detect single small tumors during a preventive appointment. However, diagnostics in ophthalmology also includes hardware techniques.
A detailed examination of the structures of the eye in ophthalmology is carried out using:
- Retinal camera (fundus camera). It can be used to photograph the fundus of the eye to identify pathological changes.
- Ultrasound.
- Biomicroscopy of the eye - examination of the tissues of the eyeball using a slit lamp. For young children, it is performed under general anesthesia.
- X-ray of the orbit - allows you to assess the extent of the tumor.
- CT allows you to see the exact contours of the tumor and determine the spread of metastases.
- An additional research method is MRI.
If retinoblastoma is suspected, cerebrospinal fluid sampling and examination is prescribed. In all cases of eye cancer detection, genetic diagnosis is carried out, and the medical history of all family members is collected.
Only after a full course of diagnostic measures can the stage of the disease be accurately determined and a method for combating the disease determined.
Diagnostics
If serious symptoms are detected, you should immediately contact a specialist.
Recognition of neoplasms occurs sequentially. First of all, the ophthalmologist conducts a consultation and examines the medical history. Then the eye is examined using a special lamp.
The slit lamp makes it possible to see in detail both the anterior and posterior parts of the organ. For different magnifications, a microscope is located inside its body.
The doctor must check the boundaries of the field of vision and its quality. To establish the general level of health, the patient needs to undergo several tests: blood sugar levels, the presence of hepatitis and syphilis, and a general blood test. The child must be examined by a pediatrician.
If other diseases are detected, the patient is referred to the right specialist.
Biopsy examination
It is carried out when identifying neoplasms of the eyelids. It consists of collecting material from the affected area with a syringe for subsequent detailed examination in the laboratory. The analysis shows the presence or absence of a tumor, and if pathology is detected, determines its nature.
Ultrasound
One of the main diagnostic methods. Helps determine the location of the tumor and makes it possible to measure it; the information obtained is displayed on the monitor. The process is based on echolocation and occurs painlessly.
Optical coherence tomography (OCT)
This diagnostic method allows for a thorough scan of the retina, choroid and epithelium. One OCT session is not enough; a cancer patient regularly undergoes this examination in order to monitor the development of the disease and the effectiveness of treatment.
In many cases, additional X-rays, computed tomography and MRI are performed.
MRI of the head for humans
Methods of organ-preserving treatment:
- Local chemotherapy for retinal cancer is designed to reduce the pathological focus. In this case, the drug can be injected both into the vitreous body and into the artery of the eye.
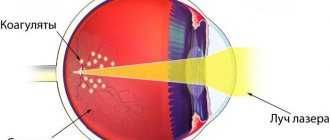
- Laser coagulation is used only for tumor sizes up to 1.5 mm.
- External radiation therapy. Children are undergoing anesthesia with mandatory head fixation. Typically, this method is used for tumors that are located far from the center of the eye. Radiation therapy with chemotherapy gives a positive result in 75% of cases.
- Cryodestruction, or cauterization of the tumor with liquid nitrogen.
In case of significant tumor growth, the presence of metastases, glaucoma, or loss of vision, surgical removal of the eyeball (enucleation) is performed. To avoid the development of complications, such as macular edema of the retina, treatment is combined with subsequent chemotherapy. This also helps reduce the risk of recurring tumors. The operation is performed as a last resort if there is a risk to the patient's life. More often this method is prescribed up to 3 years. Subsequently, eye prosthetics are performed.
Cavernous hemangioma
The tumor occurs in the retina as an independent disease or can be a symptom of a common malformation affecting the central nervous system, facial skin, and nasopharyngeal mucosa.
Women are more often affected (60%), usually the tumor is one-sided. R.Levis (1975), when observing 37 cases of cavernous retinal hemangioma, noted bilateral lesions in only 3 patients. When studying pedigrees, K. Moffat (1988) noted an autosomal dominant mode of inheritance with varied expression and incomplete penetrance. It is usually discovered by chance if the tumor is located outside the macular zone.
Clinic
Clinically, the tumor is asymptomatic for a long time, but there may be complaints of floaters or decreased central vision.
In the fundus of the eye near or on the optic nerve head, a local tumor is found, consisting of individual numerous thin-walled vascular nodules associated with a dark-colored aneurysmal dilated vein. The color of the tumor is crimson with a bluish tint. Sometimes the tumor node and the vein approaching it are covered with thin whitish fibrous tissue. In the retina, hemangioma is located in its layers. The appearance of the tumor resembles a “bunch of grapes”. The caliber of retinal vessels approaching and leaving the tumor remains unchanged. In the area of vascular growths, as a rule, there are no exudative changes.
The tumor is stationary in size during long-term observation. Almost the only complication of cavernous retinal hemangioma can be vitreous hemorrhage, but this is uncommon.
A. Reese (1976) formulated the following signs that are most often found in cavernous retinal hemangioma:
1) the tumor is represented by aneurysmal vessels; 2) the tumor is often drained by a large retinal vessel of unchanged caliber; 3) there is no exudative retinal detachment; 4) hemorrhages into the vitreous rarely occur; 5) in many cases, the surface of the tumor is covered with grayish glial tissue; 6) exceptionally low fluorescein filling of tumor vessels during fluorescein angiography; 7) possible combination of retinal cavernous hemangioma with vascular brain tumors.
Morphology
Tumor growth is detected in the inner layers of the retina.
A large tumor can occupy the entire thickness of the retina and consists of aneurysmal veins with an endothelial lining, connected to each other by narrow channels. With prolonged existence under the tumor in the outer layers of the retina, cystic degeneration occurs. The diagnosis is established on the basis of ophthalmoscopic examination and FA. In case of hemorrhoids, ultrasound scanning is informative, as it allows identifying an area of thickened retina, while the choroidal excavation typical of uveal melanoma is absent.
Differential diagnosis includes Coats' disease, capillary retinal hemangioma, retinal telangiectasias (especially when they are peripherally localized), retinal vein occlusion, diabetic retinopathy, choroidal melanoma and retinoblastoma.
Treatment
For early detected tumors, laser coagulation and cryodestruction are effective.
Laser photocoagulation can be easily performed when the tumor is localized in the post-equatorial zone. The absence of retinal detachment and an increase in the caliber of the feeding vessels allows coagulation of a tumor with a spot size of 250-500 microns, radiation power of 350-600 mW and laser exposure of 0.2-0.5 s. Coagulates should be applied in a tiled manner until an intense white color appears on the surface of the hemangioma. To avoid hemorrhages, the tumor should be destroyed in stages.
The prognosis for vision is usually good. When hemorrhages appear in the vitreous body, there may be a decrease in visual acuity, but when the latter resolves, vision is restored. With local hemangioma in the retina, the prognosis for life is good. When combined with vascular brain tumors, the prognosis is aggravated by possible intracerebral hemorrhages,
Retinal cancer in a child: the main subtleties
This diagnosis, according to statistics, occurs in only one newborn out of 15-22 thousand worldwide. In 80-90% of cases, the diagnosis is established before the child reaches 3 years of age. Hereditary retinoblastoma always affects both eyes, and its first signs appear already in the first year of a baby’s life.
Children who have had retinal cancer should undergo examinations every six months after treatment. They are registered with the dispensary for life. If they want to start a family, such patients are required to visit a geneticist and get advice, since most often the pathology is inherited.
Children with this diagnosis are at high risk of developing other types of cancer.
Retinoblastoma (retinal cancer)
Currently, the following methods are used in the treatment of retinoblastoma: surgery, radiation and chemotherapy. The correct combination of the proposed methods makes it possible to obtain good results. Therefore, when planning treatment, the following fundamental points are of great importance:
- the lesion is unilateral or bilateral;
- vision is preserved and there is a possibility of its preservation;
- the lesion is only intraocular or the process has already spread to the optic nerve;
- whether the process spreads to the orbit, to the central nervous system, or the presence of distant metastases.
The current trend is towards conservative treatment as much as possible. Cryotherapy and photocoagulation are two excellent methods of treating retinoblastomas, allowing you to save the eye and vision and with virtually no complications. In case of relapse of the disease, treatment may be repeated. However, conservative treatment is effective only for small tumors. Cryotherapy is indicated for lesions of the anterior retina, photocoagulation for lesions of the posterior retina. Surgical method The most common type of surgery for retinoblastoma is enucleation. Indications for enucleation are the massive nature of the intraocular lesion; glaucoma caused by the proliferation of tumor vessels, lack of vision and the impossibility of its restoration. The most important point of this operation is to cut off the optic nerve as far as possible. 6 weeks after this operation, prosthetics are already possible. Enucleation is the best treatment method and provides the best survival results. Mortality after enucleation is minimal. After this operation, regular examinations under anesthesia are not required in the future. However, since this operation is most often performed before the age of three, it entails large cosmetic defects, since by this age the orbit has not yet fully formed; after the operation, due to the absence of an eye, the bones that form the orbit grow more actively, which causes cosmetic defect. The removed eye must be subjected to careful histological examination. The main factors determining a poor prognosis are invasion of the optic nerve, especially at the level of the resected edge, intense invasion of the choroid, and extrascleral invasion. In cases of extraocular spread of the tumor process, orbital exenteration is indicated - an operation even more crippling than enucleation. Radiation treatment. In an attempt to preserve vision, radiation is becoming the treatment of choice for patients with retinoblastoma. The goal of radiation treatment is cure while preserving vision. However, the benefits of choosing this method must be weighed and compared with possible immediate and long-term complications. If vision can be preserved, radiation therapy should be preferred over enucleation. There are several methods of radiation therapy, but external irradiation with two lateral fields is most often used. Since most patients have multiple tumors in one or both eyes, and these tumors are multifocal in origin, the irradiation field should include the entire retina, the anterior border of which is the ora serrata. The irradiation field should also include the vitreous body and 10 mm of the anterior part of the optic nerve. Doses of radiation therapy should be high - from 3500 Gy in patients of groups I-III, to 4500 Gy in patients of groups IV-V. It is recommended to use special blocks for the lens to avoid the development of post-radiation cataracts. Some authors criticize lateral fields because recurrences in the anterior retina are possible. In practice, this rarely happens, but in the case of such a localization of the tumor, additional cryotherapy is indicated. Since patients with retinoblastoma are predominantly children under three years of age, radiation therapy often requires anesthesia and a special table to immobilize the patient. Retinoblastoma is a tumor that is extremely sensitive to radiation treatment. By receiving radiation therapy alone, 75% of patients can be cured, and when cryotherapy is added, the cure rate may be higher. For optimal radiation treatment, the participation of a group of specialists is necessary, which includes a nurse, doctors of various specialties, and anesthesiologists who know this pathology well. In some cases, it is possible to use radioactive plates, but their use is limited, since the radiation dose is unevenly distributed and is high only at the implantation site. Such a high dose of radiation can lead to vascular damage and subsequent bleeding. Therefore, this radiation treatment technique is indicated only for very small tumors located outside the optic disc. Also, this technique is not indicated for children with hereditary retinoblastoma, since in this case the multifocal nature of the lesion is most likely. Chemotherapy. The surgical method and radiation therapy can provide a cure in almost 80-90% of cases. CT should be used in cases of massive intraocular lesions, with invasion of the optic nerve, especially if there is invasion of the resected edge of the nerve, with orbital lesions, with regional metastases. Retinoblastoma is highly sensitive to a number of chemotherapy drugs. The treatment uses a combination of several cytostatics. The combination of vincristine, carboplatin, and Vepeside is the most effective currently. Vincristine, cyclophosphamide, and doxorubicin are also effective, but recently the first combination has been preferred due to the fact that cyclophosphamide increases the risk of developing second tumors and leads to sterilization of patients. In recent years, in developed countries, due to good diagnosis, an increase in the number of patients with early stages of the disease has been noted. In these cases, cryotherapy, photocoagulation and radiation therapy may be sufficient to cure the patient.
Prevention and prognosis of retinoblastoma
The best way to prevent the disease is to conduct DNA diagnostics at the stage of pregnancy planning. If a mutation in the RB1 gene is detected, IVF should be used.
Preventive examinations by an ophthalmologist in the first years of a child’s life will help identify the disease at an early stage. A child's eyes should be monitored more closely if a family member is known to have the mutated gene.
If the disease is detected early, the prognosis is favorable. Even when cancer is detected in late stages, remission is achieved in 47% of patients. Modern methods practically eliminate death that occurs due to extensive metastases. In most cases, it is possible to save the eye and vision of a small patient, which contributes to his further harmonious and versatile development.
Treatment
Removal of tumors occurs microsurgically. For this use:
- Laser evaporation – tumor tissue is evaporated by a laser beam.
- Electroexcision is the removal of tissue using an electric knife. With this method, tissues are restored without suppuration.
- Cryosurgery is the instant freezing of tissue for the purpose of necrosis.
- For vascular tumors, chemicals are injected and then the tumor is surgically removed.
If a tumor occurs in distant parts of the eye, surgical treatment is indispensable. The eyeball must be removed and replaced with a prosthesis. If the tumor is malignant, radiotherapy is used.
Symptoms
Because there are many types of cancer (see above), symptoms may vary.
Symptoms of eye cancer depend on the type of pathology. Main clinical manifestations:
- deterioration of visual function up to complete loss;
- increase in dark spots around the arch of the eye;
- the appearance of sudden rather severe pain;
- bulging eyes or bulging eyes;
- displacement of the eyeball;
- development of strabismus;
- flashes before the eyes.
Strabismus as a symptom of cancer
In some patients, a mole or nevus forms on the eye. It can also appear as a pterygium or pinguecula. These formations are harmless, and in most cases are not related to oncology, but doctors do not exclude this possibility. The same applies to conjunctival cysts.
Usually, nevi do not interfere with a person in any way, but the appearance of sudden pain is sufficient reason to immediately consult a doctor. Also, with eye cancer, the general condition can worsen - vitality drops, a person quickly gets tired, loses appetite. Pathology is diagnosed only in late stages or by pure chance - for example, as part of a general examination.
Nevus of the eye