general description
Lens luxation is a complete or partial (dislocation or subluxation) dislocation of the lens from its normal location.
Lens dislocation can be congenital or acquired. Congenital disorder of the location of the lens is a consequence of insufficient development, partial absence of the zonules of Zinn. An acquired disorder of the location of the lens develops as a result of rupture of the zonular ligaments due to blunt trauma to the eye or degenerative changes in the ligaments and vitreous body (cyanyl, high myopia, inflammatory processes). Congenital heterotopia lens is usually bilateral in nature and is often a stigma of connective tissue dysplasia.
Pathogenesis
In the mechanism of development of the congenital variant of the disease, the leading role is played by weakness, partial or complete absence of the ciliary ligament. The vast majority of patients with a genetic predisposition are characterized by a defect in the synthesis of collagen or elastin and a disorder of protein metabolism. In case of partial rupture of the ciliary girdle, the lens remains fixed to the parietal layers of the vitreous body; in case of complete rupture, it moves freely in the vitreal cavity. Dilation of the pupillary opening causes dislocation into the anterior chamber region, usually occurring in the “face down” position.
Violation of the attachment of the biological lens to the ciliary band during cataracts entails dysfunction of the ligamentous apparatus. In case of farsightedness, overstretching of the ligament of Zinn leads to its partial damage. An increase in ophthalmotonus or performing a slight load potentiates the rupture of the ciliary band and the occurrence of ectopia. When the eyeball is injured, the ciliary band is the weakest point, vulnerable to damage. This is due to the fact that the shock wave does not lead to rupture of the capsule, but to deformation and tension of the fibers of the ligament of Zinn. Involutional changes in the lens masses and ligamentous apparatus provoke ectopia in elderly patients.
Clinical picture
- Reduction of the anterior chamber on the side of displacement.
- Iridodonesis.
- Determination of the edge of the lens when examined in transmitted light in the form of an arcuate dark line.
- Double image of the fundus during ophthalmoscopy.
- When examined through a lens, the refraction changes towards myopia, and when examined through the area of the pupil devoid of a lens, towards hyperopia. Refractive errors are common.
- Visa depression.
- Aphakia due to dislocation of the lens into the vitreous body.
Dislocation of the lens into the vitreous body is fraught with such serious complications as iridocyclitis, secondary glaucoma, and retinal detachment. If the dislocation occurs after an eye injury, then complications such as inversion of the iris, uveitis, hemophthalmos, and retinal detachment are possible.
Prognosis and prevention
Timely lensectomy in 2/3 of cases makes it possible to completely restore visual acuity and normalize the circulation of intraocular fluid. 30% of patients develop severe postoperative complications. Specific methods of prevention have not been developed. Non-specific preventive measures include the use of personal protective equipment when working in production conditions (goggles, masks). To reduce the likelihood of dislocation, patients with hypermetropic refraction are advised to correct visual dysfunction using glasses or contact lenses.
LiveJournal
Treatment of lens luxation
- In case of lens subluxation, phacoemulsification, surgical extraction of the lens with implantation of its artificial analogue.
- In case of dislocation in the anterior chamber, extraction of the lens with implantation of its artificial analogue is performed.
- In case of dislocation into the vitreous body, vitrectomy with extraction of the lens and implantation of its artificial analogue is performed.
The prognosis is favorable in most cases. The development of complications depends on the effectiveness of the treatment and the level of pathological changes in the retina and optic nerve.
Diagnostics
Physical examination reveals a decrease in the transparency of the anterior segment of the eyes, which may be combined with signs of traumatic injury. When the eyes move, phacodonesis develops, which is detected by an ophthalmologist under focal lighting. When performing a test with mydriatics, no reaction of the pupils is observed. Special diagnostic methods include the use of:
- Non-contact tonometry
. When measuring intraocular pressure, it is possible to diagnose its increase. IOP reaches critical values only when the outflow of aqueous humor is impaired. A mobile dislocation causes a slight increase in ophthalmotonus. - Visometry
. Visual acuity decreases sharply, regardless of the degree of transparency of the lens. With the additional use of computer refractometry, it is possible to diagnose the myopic type of clinical refraction. - Ultrasound of the eye
. An ultrasound examination reveals a dislocation in the anterior chamber area or the vitreous body. A unilateral or bilateral rupture of the ligament of Zinn is determined. The vitreal cavity has a non-homogeneous structure. When the lens is fixed to the retina, retinal detachment occurs. The anteroposterior axis is shifted. When completely ruptured, the capsule with the main substance acquires a spherical shape. - Biomicroscopy of the eye
. With the traumatic genesis of the disease, injection of conjunctival vessels and foci of hemorrhage are visualized. The transparency of optical media is reduced. Secondary changes in the cornea are represented by microerosive defects. - Gonioscopy
. When the displacement vector is directed anteriorly, the volume of the eye chamber is sharply reduced. In patients with an incomplete form of pathology, the space limited by the iris and cornea is deep, without pathological changes. The anterior chamber angle (ACA) has an uneven structure. - Optical coherence tomography (OCT)
. The study makes it possible to determine the nature of the location of the luxated lens and the type of damage to the ligament of Zinn. OCT is used immediately before surgery to select the optimal surgical tactics. - Ultrasound biomicroscopy
. In the case of a congenital variant of the disease, the technique makes it possible to detect defects in the ciliary ligament over a range of 60° to 260°. The lens is displaced in the horizontal and vertical planes. The depth of corneal damage is measured.
In case of traumatic origin of the disease, patients are additionally prescribed radiography of the orbits in direct and lateral projection. In the early postoperative period, IOP measurement using a non-contact method is indicated. To study the nature of the circulation of the intraocular fluid 5-7 days after surgery, electron tonography is used. The study determines the risk of developing glaucoma.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 10 | 20 | 20 | 20 | 20 | 20 | 20 | 10 | 20 | 20 | 20 | 20 | 20 | 20 |
Causes of injury
Pathology has a large number of progression factors. A person may be born with a lens shift due to a hereditary predisposition in people with pathologies:
- Marfana;
- Knista;
- Ehlers-Danlos.
Genetic hyperlysinemia and lack of sulfite oxidase can also provoke this condition. One of the most common causes of the problem is a negative effect on the eyes. These can be blunt trauma or penetrating trauma. The damage may be accompanied by cataracts, malformation of the ciliary ligament and vision.
Symptoms
One of the clear signs of lens luxation is twitching of the iris film. The open chamber of the eye becomes uneven and spasmodic, more narrowed in the direction where the lens is shifted. But only a specialist can distinguish such changes. The person himself will only notice decreased vision or double vision.
The noncongenital form is characterized by paroxysmal pain from the moment of displacement, a sharp decrease in the ability of the organ of vision to observe two points separately. Over time, the pain only intensifies. The conjunctiva begins to turn red, and the patient begins to experience severe discomfort. Complications of the pathology can provoke secondary glaucoma. Absolute loss of vision is possible.
Why is deviation dangerous?
In severe cases of pathology or in case of untimely treatment, the following complications develop:
- Secondary glaucoma. It is expressed in a persistent increase in intraocular pressure.
- Iridocyclitis. Occurs when pathogenic microorganisms enter the iris and ciliary body. The danger of the disease is the spread of bacteria to all structures of the eye, as well as fusion of the pupil.
- Retinal detachment. With this pathology, the retina is rejected from the choroid and there is a danger of complete loss of vision.
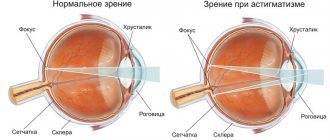
A complication of lens subluxation is often a vitreous hernia, which is formed as a result of a defect in the structures located near the VT. May cause clouding of the cornea and decreased vision. Severe consequences often develop after surgery. These include intraocular lens displacement, postoperative astigmatism, and corneal edema.
Changes in shape, size and other abnormalities of the lens
Lenticonus
is a change in the shape of the surface of the lens, is rare and is predominantly a congenital anomaly, however, cases of lenticonus of traumatic etiology are known. It can be anterior, posterior and internal (Fig. 100), and is predominantly one-sided. Anterior lenticone is a cone-shaped, less often spherical, protrusion of the anterior surface of the lens into the anterior chamber. In posterior lenticonus, a similar protrusion of the posterior surface of the lens faces the vitreous. The internal lenticone is characterized by a cone-shaped protrusion facing into the thickness of the lens.
Rice. 100. Lenticonus: a - anterior; b - rear; in - internal
The pathogenesis of the anomaly is not well understood. In the origin of anterior lenticonus, importance is attached to defects in lens lacing, weak resistance of the anterior lens bag, abnormal attachment of zonular fibers or their absence, and adhesion of the lens to the posterior surface of the cornea. The development of posterior lenticonus is associated with tension or rupture of the posterior capsule of the lens during the reverse development of the embryonic vitreous artery. The inflammatory genesis of the anomaly cannot be excluded.
The degree of protrusion of the lenticonus and the diameter of its base are different. The protruding portion of the lens is transparent in most cases. In transmitted light in these cases, changes are visible that resemble a drop in oil, kaleidoscopic phenomena. With a clouded lenticonus, a dark-colored disk is detected in transmitted light against the background of a red reflex from the fundus. The rest of the lens is transparent.
When the eye moves, the anterior lenticone moves in the direction of movement, the posterior one in the opposite direction. The anterior figures of Purkinje are characteristically shaded. Refraction in the lenticonus region is high myopia, along the periphery of the lens is emmetropic refraction, farsightedness or high myopia. The anomaly is usually accompanied by decreased visual acuity and may cause amblyopia.
The diagnosis of lenticonus is established on the basis of decreased visual acuity and a characteristic clinical picture. Anterior and posterior lenticones should be differentiated from anterior and posterior polar cataracts.
Therapeutic measures are limited to preventing the development of amblyopia (pupil dilation, training exercises). With significant size of the lenticone and a sharp decrease in visual acuity, it may be necessary to remove the lens.
Coloboma of the lens
- a rare congenital anomaly of the lens, characterized by the presence of a notch along its equatorial edge (Fig. 101).
Rice. 101. Lens coloboma
The pathogenesis of lens colobomas has not been fully elucidated. It is believed that the main cause of this anomaly is the complete or partial absence of the ciliary band in the area where coloboma is formed. The possibility of the development of lens colobomas in the postnatal period due to the mechanical pressure of various dense formations (cysts, tumors) on the ciliary band is not excluded.
Lens colobomas can form in one or both eyes at the same time; they are most often located in the lower or lower inner quadrant and have an elliptical, crescent-shaped or triangular shape. More often there is one notch, much less often there are two. The transparency of the lens is preserved in most cases.
In the area of coloboma there is no ciliary band, the ciliary processes are changed. Coloboma of the lens can be an isolated anomaly, but is more often found in combination with other congenital eye defects: microphthalmia, coloboma of the iris and choroid. Small lens colobomas themselves may not affect visual acuity. In the presence of other changes in the eye, vision is reduced to varying degrees. With large colobomas, as a rule, lens astigmatism is observed, and refraction is often myopic.
Diagnosis of lens coloboma
established on the basis of a characteristic clinical picture when examined in transmitted light and biomicroscopy. In most cases, the anomaly is detected with a dilated pupil.
Therapeutic measures for lens colobomas are limited to correction of refractive error, if any, and, if indicated, amblyopia is treated.
Microphakia
- a congenital anomaly manifested in a decrease in the size of the lens associated with a stop in its growth. Most authors believe that it is always combined with spherophakia, but cases of isolated true microphakia are known. Bilateral damage is typical. Microphakia can be observed as an isolated ocular abnormality or combined with general constitutional abnormalities. Spheromicrophakia is one of the manifestations of Marchesani and Marfan syndromes.
The anomaly is of a family hereditary nature. The occurrence of microphakia is associated with a primary defect in the development of the ciliary girdle, stretching and degeneration of zonular fibers.
Signs of microphakia are:
reduction in the size of the lens, which has a spherical shape, excessively close attachment of thinned fibers of the ciliary girdle to the equator, iridodonesis. With a dilated pupil, the equatorial edge of the lens in the form of a golden ring is visible throughout. Cloudiness of the lens is often observed. Myopic refraction of the eye is characteristic.
With microphakia, the lens is easily pinched in the pupillary opening or falls out into the anterior chamber, which leads to a sharp increase in intraocular pressure, accompanied by pain. In such cases, urgent removal of the dislocated lens is indicated.
Spherophakia
- a spherical lens, in most cases combined with microphakia, dislocations, as well as general constitutional anomalies. It is a congenital family-hereditary anomaly, the occurrence of which is associated with defects in the development of the ciliary girdle.
Clinical manifestations of spherophakia are a spherical shape of the lens, a deep anterior chamber of the eye, iridodonesis, and myopia. Secondary glaucoma, subluxations and dislocations of the lens may occur.
Spherophakia cannot be treated. If complications occur (glaucoma, dislocations), surgical intervention is required - antiglaucomatous surgery, removal of the displaced lens.
Double lens
- a congenital anomaly in which there are two lenses of different sizes, located in the frontal or sagittal plane. The anomaly is extremely rare. The occurrence of biphakia is explained by a delay in the reverse development of capsulopupillary vessels, which exert pressure on the lens in the prenatal period.
Indentations on the surface of the lens
- A rare anomaly characterized by the presence of eccentric pit-shaped depressions on the posterior surface of the clear lens.
Congenital aphakia
- congenital absence of the lens and its traces. The anomaly is extremely rare and is a consequence of disturbances in the process of lens lacing in the early stages of embryogenesis; in this case, differentiation of the integumentary ectoderm does not occur, and the lens rudiment is absent. Congenital aphakia is usually combined with other eye defects, as well as constitutional anomalies.
Secondary congenital aphakia, which is a consequence of early intrauterine resorption of the lens, is distinguished from true congenital absence of the lens. In these cases, when examining the area of the pupil, it is usually possible to detect the remains of the capsule and connective tissue formations.
Treatment of congenital aphakia
consists in its possible earlier optical correction and treatment of amblyopia.
Changes in the lens due to the presence of remnants of the vascular capsule are observed very often; they are a consequence of a disruption in the process of reverse development of the vascular capsule of the lens, which normally should be completed by the 8th month of intrauterine life.
There are various variants of the anomaly:
pinpoint opacities of the posterior capsule of the lens, remnants of the vitreous artery in the form of a thin whitish cord at the posterior pole of the lens, thin rounded lines on the capsule, pigment deposits in the form of individual dots, etc.
Congenital changes associated with the presence of remnants of the vascular capsule of the lens must be differentiated from acquired ones.
Rice. 102. Residual pupillary membrane
Residual pupillary membrane is a congenital anomaly of the development of mesodermal tissue of the iris, but its remnants can be closely associated with the lens, in which changes in the form of opacification of the capsule or substance are observed. The clinical manifestations of residual pupillary membrane are very diverse. These can be small needle- or star-shaped pigment deposits that form into bizarre shapes or a delicate mesh on the front surface of the lens. More often, the pupillary membrane is a membranous formation connected by threads to the iris in the area of the small arterial circle or pupil (Fig. 102).
Changes in lens position
Complete and partial displacements of the lens can be congenital or acquired.
Congenital dislocations and subluxations of the lens
Congenital lens dislocations (ectopia) in most cases are hereditary.
The cause of ectopia of the lens is anomalies in the development of the ciliary girdle (defects, partial or complete aplasia), underdevelopment of the ciliary body, ciliary processes due to improper closure of the choroidal fissure and pressure of the vitreous arteries. Destruction and disruption of the integrity of the ciliary girdle occurs with hereditary lesions of the connective tissue (Marfan, Marchesani syndromes, etc.), disorders of the metabolism of sulfur-containing amino acids (homocystine). Ectopic lens can be an isolated lesion, but is more often combined with other congenital eye defects:
coloboma and opacification of the lens, coloboma of the iris and choroid, polycoria, aniridia, etc. Concomitant extraocular congenital anomalies and diseases are often found - clubfoot, six-toed, congenital heart disease, inguinal hernia, skeletal anomalies, etc.
Clinical manifestations of lens ectopia are diverse and are determined by the degree and direction of displacement, duration of existence, the presence or absence of concomitant eye changes and complications. The process is often bilateral.
Lens luxation into the anterior chamber
With complete dislocation, the spherical lens is located in the anterior chamber (Fig. 103). It is usually transparent, less often partially or completely clouded. The anterior surface of the lens is adjacent to the posterior surface of the cornea, the posterior surface is adjacent to the iris, pushing it posteriorly and pressing the pupillary edge to the anterior limiting membrane of the vitreous. The pupil, as a rule, is deformed, especially in cases where the fibers of the ciliary girdle are preserved in a separate area, which, spreading across the pupil, change its shape. Vision is sharply reduced.
Rice. 103. Dislocation of the lens into the anterior chamber
When the lens dislocates into the anterior chamber, the pathways for the outflow of intraocular fluid are blocked, which leads to a sharp increase in ophthalmotonus, resulting in stagnant injection, corneal edema, eye pain, and headaches. When the lens remains in the anterior chamber for a long time, degenerative changes in the cornea develop.
Complete congenital dislocation of the lens into the vitreous
- a rare anomaly.
Subluxation (subluxation) of the lens
- partial displacement of the lens. In the area of the pupil, a dislocated lens, its equatorial edge, and preserved individual thinned fibers of the ciliary girdle are visible (Fig. 104). With a slight subluxation of the lens, its presence can be judged only by indirect signs, and its equatorial edge can only be seen with a dilated pupil. The direction of displacement can be different. The directions of subluxation in both eyes are characterized by symmetry, while the degree of lens displacement is usually different.
Rice. 104. Lens subluxation
The displaced lens takes on a more regular spherical shape; it can be transparent or cloudy. The integrity of the anterior limiting membrane of the vitreous body is often preserved; if it is disturbed, the vitreous body may protrude into the anterior chamber. In cases where the lens occupies about or more than half of the pupil area, ophthalmoscopy produces a double image of the fundus.
Refraction when examined through the lens is myopic, through the area free of the lens, hypermetropic. When the lens is subluxated, an uneven anterior chamber, iridodonesis, miosis, monocular diplopia, and decreased visual acuity are observed. Complications may include secondary glaucoma, hemorrhages, and retinal detachment.
Lens ectopia in congenital syndromes
Marfan syndrome
is a family-hereditary disease that is usually transmitted in an autosomal dominant manner. The disease is based on a metabolic disorder of connective tissue.
With Marfan syndrome, there is a combination of eye changes with damage to the cardiovascular, musculoskeletal and other body systems, disorders of the endocrine glands, as well as the psyche. Damage to the cardiovascular system is manifested in the development of heart defects, aortic aneurysms, vein thrombosis and varicose veins, etc.
Signs of damage to the musculoskeletal system are arachnodactyly, dolichocephaly, fragility of bones, frequent dislocations of the limbs due to weakness of the ligamentous apparatus, joint contractures, scoliosis, kyphosis, funnel chest, winged shoulder blades. Underdevelopment of subcutaneous fatty tissue, muscles, genital organs, prolapse of organs, lengthening of the intestine, etc. are also observed. The most common triad of symptoms is gigantism, arachnodactyly, ectopia lentis.
Patients with Marfan syndrome often die in early childhood, but can live into adulthood and even old age.
Damage to the organ of vision in Marfan syndrome is observed in 50-80% of patients, often being one of the early signs of the disease. Ectopic lenses, cataracts, embryotoxon, strabismus, nystagmus, iris hypoplasia, aniridia, changes in the vitreous body, degeneration and retinal detachment, secondary glaucoma, etc. may be observed. Early signs of Marfan syndrome include embryotoxon, hypoplasia of the iris, especially its pigment border.
Subsequently, destruction of the vitreous body, destruction of the fibers of the ciliary band and, as a result, ectopia of the lenses occur. The displacement of the lenses is always bilateral, but the degree of displacement in each eye is usually different. Marfan's disease is characterized by a predominant displacement of the lenses upward, as well as upward and outward, which is caused by the destruction of the fibers of the ciliary girdle in the lower parts. Ectopia of the lens gradually progresses, the degree of its displacement increases until it dislocates into the anterior chamber.
Marchesani syndrome is inherited in a dominant and autosomal recessive manner. In many ways, this syndrome is the opposite of Marfan syndrome. Characteristic manifestations are short stature, shortened torso, neck and limbs, brachycephaly, limited mobility in joints, and diseases of the cardiovascular system. Anomalies and diseases of the organ of vision are observed: ectopia of the lenses downwards, spherophakia, microphakia, high myopia, retinal detachment, secondary glaucoma. Patients usually die at the age of 40-50 years.
Homocystinuria
- a hereditary disease associated with a violation of the metabolism of the sulfur-containing amino acid - homocystine. The main symptoms of eye damage are ectopic lenses, cataracts, myopia, and retinal degeneration. Ectopic lenses are observed in 5% of patients and appear in the early stages of the disease. Unlike Marfan syndrome, the lenses always shift downwards, which is due to changes in the fibers of the ciliary girdle in the upper segment.
Rieger syndrome
- a combination of hypoplasia of the mesodermal layer of the iris, pupil deformation in the form of a slit and Axenfeld’s symptom with anomalies of the anterior chamber angle and secondary glaucoma. Ectopic lens, congenital cataract, choroidal colobomas, and dermoid cysts at the limbus may be observed.
Ehlers-Danlos syndrome
- a hereditary disease, the symptoms of which are blue coloration of the sclera, spontaneous dislocation of the lens, keratoconus, epicanthus, increased vulnerability of the skin, fragility of superficial vessels, recurrent hematomas, poor development of subcutaneous fatty tissue. Scoliosis, hip dislocations, syndactyly, and bronchiectasis may be observed.
How does complete and partial ectopia manifest?
Complete ectopia of the eye
It is important to pay attention to the symptoms of dislocation or subluxation in time. The main symptom of complete ectopia is iridodonesis. This is a twitching of the iris of the eye. The fact is that when the lens is dislocated, it constantly vibrates. The sensitive tissue of the iris comes into contact with the biological lens and also begins to tremble. This symptom is visible to the naked eye. Iridodonesis is also diagnosed during instrumental examination. The image quality deteriorates significantly.
Important: Sprained ankle: symptoms, emergency care
Partial ectopia is more difficult to diagnose. Without a slit lamp, it is difficult to see any signs of pathology. Partial displacement of the lens is best seen in the supine position. Iridodonesis with subluxation is not always noticeable. Biomicroscopy is often necessary to diagnose this symptom. During the procedure, different depths of the vessels with ocular fluid are noted.
Vision in the initial stages of partial ectopia deteriorates slightly. When a biological lens dislocates, diplopia is diagnosed. Double vision is present even if one eye is closed. With ectopia towards the anterior ocular chamber, the ophthalmologist notices a small golden oil drop on the surface of the visual organ.