The mechanism of pathology development
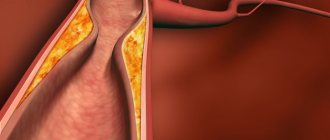
Most often, thrombosis of the central retinal vein and its individual branches is determined in humans. The condition is characterized by a sharp disruption of normal blood flow through the orbital veins and vessels.
If there is a blockage of the central vein, then there is a violation of the outflow of blood. It begins to accumulate in the vessels, which contributes to their deformation. The vascular walls become denser, which leads to slower blood flow. Gradually, a blood clot forms, disrupting normal blood circulation.
Prolonged stagnation of blood leads to the release of its liquid part into the tissues around the vessel. There is an increase in pressure inside the eye, and hemorrhage and swelling may develop. One possible consequence is macular edema, a swelling of the central region of the retina.
In such a case, the condition is dangerous; complete restoration of vision remains in question.
If the blood supply to the eye is disrupted, optic nerve ischemia is often diagnosed, characterized by a sharp decrease in visual function and monocular blindness. The disease occurs more often in men and can lead to complete loss of vision.
Occlusion of the central retinal artery (CRA) and its branches poses a serious danger due to the rapid development of unpleasant symptoms and irreversible consequences.
Prevention
Central retinal vein thrombosis can be prevented. To do this, you need to monitor your health and undergo an annual examination. Reduces the risk of developing the disease by eliminating the pathogenetic factor:
- in case of hypertension, you should take medications to normalize blood pressure;
- for diabetes mellitus, control glucose levels: follow a diet, normalize weight and take recommended endocrine medications;
- if retinopathy is present, patients should visit an ophthalmologist every 6 months;
- endocrinological diseases, especially pathology of the thyroid gland, also require correction; women should remember that oral contraceptives increase the risk of blood clots - you should not get carried away with them;
- people suffering from cardiovascular pathology should take anticoagulants: for example, Aspirin daily.
Currently, a large number of special exercises have been developed that not only prevent deterioration of eye condition, but also increase visual acuity.
Eye training:
- Sharply open and close your eyes 5 times, alternately look left and right, then up and down;
- blink quickly for 2 minutes;
- lightly press on the closed eyelid for a couple of seconds, repeat 10 times.
In addition to exercising, it is important to maintain a healthy lifestyle. Moderate physical activity and the elimination of stress are necessary for the health of the body, including the eyes. Compliance with diet is an important component of the prevention of thrombosis of any location. Eating blueberries has a good effect: these can be fresh berries, frozen or pharmaceutical preparations.
Patients with predisposing factors should understand that eye thrombosis can lead to irreversible consequences that cannot be eliminated by any drugs or surgeries. That is why it is necessary to constantly prevent blood clots, lead a healthy lifestyle, and consult a doctor at the first symptoms of the disease.
Types of thrombosis
Depending on the degree of damage to the retinal veins, two types of thrombosis are distinguished:
- Ischemic. With this type, most of the vessels in the eyeball are damaged. A serious hemorrhage in the retina is diagnosed, and visual function is seriously reduced. Irreversible consequences may develop if treatment is not started on time.
- Not ischemic. A small area of blood vessels is affected, there is no hemorrhage, visual impairment is minimal and unnoticed by the patient.
In medicine, there is also the concept of complete and incomplete thrombosis of the central vein. The first group includes the ischemic form, the second – non-ischemic. The degree of ischemia directly affects the quality of a person’s vision.
Symptoms
When this pathological condition occurs, the following signs are observed:
- decreased visual acuity;
- reduction of the field of perception;
- formation of “blind spots”.
The development of pathology occurs in several stages:
- Poor circulation, changes in the walls of blood vessels. Stagnation occurs. In some cases, vision deteriorates slightly.
- Tissue swelling occurs. Hemorrhage occurs.
- Extensive thrombosis develops. Damage to new vessels and areas.
The development of pathology occurs painlessly and suddenly. If any changes in visual function occur, you should immediately consult an ophthalmologist.
Find out how to treat pterygium of the eye here.
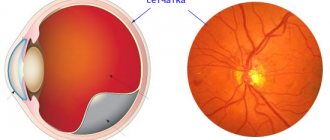
Photo of the fundus affected by the disease
How not to miss an insidious enemy - the first symptoms of eye cancer.
Reasons for development
This pathological condition develops as a consequence of various health problems of the patient.
There is a division of the most common causes according to the patient’s age:
| Age | Causes |
| Elderly |
|
| Young people |
|
| All age categories |
|
Factors that provoke the development of the disease are also identified:
- Increased body weight.
- Passive lifestyle.
- Alcohol abuse.
- Lack of vitamins in the body.
These factors are not capable of independently triggering the development of thrombosis, but their combination increases the likelihood of its occurrence several times. This disease affects women and men equally.
Clinical picture
Thrombosis develops gradually. With partial occlusion, a person does not notice any bright signs, the change in vision is minimal. The disease is often diagnosed accidentally during an examination by a doctor.
A sick person may experience:
- Slight decrease in visual function.
- Peripheral hemorrhages.
- Pallor of the arteries.
- Areas of excess blood are difficult to discern.
The ischemic form of thrombosis is characterized by the presence of more pronounced symptoms:
- Massive hemorrhages.
- Severe swelling.
- Excess blood accumulation is very noticeable.
- Noticeable loss of vision.
- Poor reaction of the pupils to light.
- Marked narrowing of the ophthalmic artery.
There are several stages of thrombosis. Each of them is characterized by the development of different symptoms.
Stages:
- The first stage is called prethrombosis. At this stage, venous blood stagnates. The veins become wider, darken, and tortuosity of the vessels appears. The center of the retina becomes swollen. At the first stage, a person may experience blurred vision; this phenomenon is not perceived as a symptom of the disease.
- The second stage is thrombosis. It is characterized by serious circulatory disorders, the occurrence of hemorrhages in the retina and other parts of the eyeball. The boundaries of the optic nerve are poorly visible or not visible at all. Macular edema is present and visual function is severely impaired. The patient notes the presence of a veil before the eyes, loss of visual boundaries. In the absence of adequate treatment, complete or incomplete thrombosis develops, and pathological changes in the retina are noted.
- Postthrombotic retinopathy is the third stage of the disease. The return of a person's vision occurs at a slow pace. Unnatural capillary formations are diagnosed. There are residual hemorrhages in the fundus. During the recovery period, new blood vessels may form in places where they should not be.
Unfortunately, relapse of the disease is possible in the absence of proper treatment.
Stages and symptoms
Normal retinal thrombosis occurs in only three stages:
- Prethrombosis. This stage can be characterized by tortuosity and slight dilatation of the veins, as well as isolated hemorrhages. Here, clinical manifestations have not yet been observed, but “fogging” in the organs of vision may periodically appear.
- Thrombosis. The second stage is determined by noticeable linear hemorrhages in the fundus, swelling of the macula on the retina and not entirely clear boundaries of the optic nerve head. In addition, there is a persistent “veil”, as well as a sharp drop in visual acuity.
- Postthrombotic changes. At the final stage, the fundus of the eye is covered with traces of hemorrhages and newly formed vessels with excessively thin walls. At this stage, visual acuity returns extremely slowly.
Diagnostics
An experienced ophthalmologist can easily determine the degree of thrombosis. Diagnosis of the disease consists of interviewing the patient and conducting specific examinations. The doctor finds out when changes in visual functions began, what medications the patient is taking, and whether the person has certain diseases.
After conducting a survey and collecting information, studies are prescribed using special techniques:
- Visometry. The method involves studying visual acuity. In the ischemic form of thrombosis, the severity exceeds 0.1, in the non-ischemic form - below this indicator.
- Tonometry. During the study, the pressure in the eyeball is measured. Indicators are taken throughout the day. In a diseased organ, the numbers will be 2-3 mmHg. Art. lower than in a healthy person.
- Perimetry. A method that helps determine the narrowing of the field of vision (scotoma). With thrombosis, a similar phenomenon is observed in the area of the affected retina. The density of the scotoma varies with different amounts of hemorrhage and the presence of ischemic foci.
- Microperimetry. The method is used to determine the reaction of certain parts of the retina to light, which allows you to accurately identify the affected area.
- Biomicroscopy. Allows you to see signs of thrombosis: crushing of the anterior chamber of the eye, a suspension of blood in the vitreous body, lack of a friendly reaction of the pupils when illuminating the diseased eye.
- Optical coherence tomography. Examination using a scanning beam helps determine the structure, size of swelling and features of the course of the disease. The method is used to evaluate the effectiveness of treatment.
- Fluorescein angiography (FA). An effective technique that helps determine the type of thromboembolism, the degree of the pathological process, the affected area, and the period of onset of the disease. The method is often used during the first examination; it helps determine the presence of thrombosis if other methods have not helped.
After confirming the diagnosis, appropriate treatment is prescribed aimed at eliminating the causes and symptoms of thrombosis and restoring visual function.
Self-determination of the disease at an early stage is impossible.
Symptoms are minimal; people often do not pay attention to minor visual impairment. Intense signs are observed during a serious course of the disease, when the person no longer sees well.
A preventive ophthalmological examination is required at least once every 6 months. Regularly visiting a medical specialist will help you not to miss the onset of the disease and select therapy on time.
Treatment Options
In general, treatment of ocular thrombosis is carried out taking into account the diagnostic results. Therapy can be carried out on an outpatient basis or in a hospital setting. The decision on hospitalization is made by the ophthalmologist based on the severity of the disease.
All patients are recommended:
- Avoid strenuous physical activity
- Follow a diet (table No. 15)
- Prevent direct sunlight from entering the affected eye
- Maintain hygiene
- Temporarily stop working at the computer, watching TV, reading
It is strictly forbidden to self-medicate, take medications or perform any procedures without the approval of the attending physician.
Drug therapy
It is the main method of treatment, which is conservative in nature. Therapy using drugs is aimed at stabilizing blood flow in the affected vessels and preventing the progression of the pathological process.
Principles of treatment
Treatment of thrombosis depends on the severity of the disease. For uncomplicated types, the use of medications is sufficient.
Complicated forms of thrombosis will require surgical intervention. The choice of treatment method remains with the doctor.
Conservative treatment
The use of medications helps restore normal blood circulation in the eyeball and visual functions.
The doctor will select medications based on the degree of thrombosis and the patient’s condition. Before treatment, the patient must inform the doctor about the medications he is taking.
Medicines used in therapy:
- Medicines that lower blood pressure. These can be tablets - Nefedipine, Phenigidine. A solution of the drug Dibazol is administered through a vein; Lasix is used for intramuscular administration. Timolol will help reduce pressure in the eyes.
- It is possible to normalize blood flow with the use of fibrinolytic drugs. The drug Plasminogen is injected into the under-eye space for two weeks.
- To avoid relapse of the disease, the patient may be prescribed Acetylsalicylic acid. The intake is carried out under the supervision of a doctor to monitor blood clotting.
- Special hormonal drugs are used to reduce swelling and inflammatory processes. Dexamethasone is often used for a similar purpose - administered under the eyeball, or in the form of droppers.
- If there is pain, analgesics are used.
- Vitamin complexes are required, with the main focus on ascorbic acid and B vitamins.
All medications are prescribed by a doctor. Independent choice of medications can lead to an exacerbation of the process and serious negative consequences.
Surgical methods
Even after successful drug treatment, the patient is recommended to undergo laser coagulation of the retina. The operation is performed under local anesthesia on an outpatient basis. Its duration is no more than half an hour.
It is performed by a qualified ophthalmologist. During surgery, a laser is applied to the blood clot, causing it to dissolve. The result is the restoration of normal blood flow in the vessels of the eyeball.
The operation has some contraindications:
- Retinal disinsertion.
- Presence of cataracts.
- Hemorrhages are diagnosed in the fundus.
- Reduced transparency of the eye media.
Drug treatment of postthrombotic retinopathy
The most common method of treating pathology is medication. Doctors prescribe medications that affect metabolic processes in the structures of the eye and blood vessels. Usually, drugs are prescribed that have a hemostatic effect, normalizing vascular permeability. Ophthalmologists often prescribe Etamzilat, an antihemorrhagic agent that improves blood microcirculation. The effect of the drug is associated with an activating effect on the formation of thromboplastin. The drug does not affect prothrombin time and does not contribute to the formation of blood clots. "Etamzilat" is prescribed to take 1-2 tablets 2 times a day. In more rare cases, doctors recommend intramuscular or subjunctival administration of the drug.
Parmidin allows you to restore impaired microcirculation, reduce inflammation of the retina and the permeability of the vascular wall. This drug blocks the union of platelets, stimulates the dissolution of blood clots, and prevents the deposition of atherogenic lipids in the vascular wall, which lead to the development of atherosclerosis. The use of the drug can reduce the swelling of endothelial cells. Parmidine is taken 1.5 g per day. The duration of treatment is usually from two to six months. It is advisable to combine the drug with vitamins and lipoic acid. The use of this drug is contraindicated in patients with liver disease.
For complex therapy of postthrombotic retinopathy, doctors often prescribe:
- "Taufon";
- "Vixipin";
- "Oftan Katahrom";
- "Quinax";
- "Taurine".
In order to prevent post-thrombotic retinopathy, ophthalmologists prescribe vasodilators. Cavinton is most often used. Take it 1-2 tablets 3 times a day. The duration of treatment usually does not exceed 3 months. An analogue of this drug is Pentoxifylline. It allows you to improve blood microcirculation and dilate blood vessels. The drug is used 2 tablets 3 times a day. Taking any medications must be agreed with your doctor.
Possible consequences
In 10% of all cases of vascular thrombosis, complete loss of vision is possible. This complication often occurs as a result of ischemia of the entire central vein and optic nerve atrophy.
Insufficient blood supply leads to other complications after thrombosis:
- Atrophic changes in the nerve.
- Repeated macular edema.
- Secondary glaucoma.
The appearance of a scotoma is possible - an area of the retina of the eyeball with altered or lost visual acuity.