Age-related macular degeneration (AMD) is a chronic eye disease with a progressive course, characteristic of older people. It is indicative of damage to the central zone of the fundus - the macula or macula, with dysfunction of the retina, pigment epithelium and choriocapillaris. AMD is the most common cause of low vision and partial blindness in people over 60 years of age. The disease is equally common in all countries of the world, regardless of the level of economic development. With age, the disease tends to progress, and by the age of 65-75, certain signs of AMD are detected in almost 75% of the population, and in 10% there is partial or complete loss of central vision. After 80 years, the number of people who have lost central vision already reaches 18% of the population.
The disease has quite a lot of names, which over the years have sounded like central senile degeneration, central involutional retinal dystrophy, senile macular degeneration, age-related macular degeneration, age-related maculopathy, atherosclerotic macular degeneration, Kunt-Junius type dystrophy, familial drusen, central chorioretinal dystrophy. Currently, clinical practice has proven that all these pathologies are signs of one disease.
Causes and risk factors
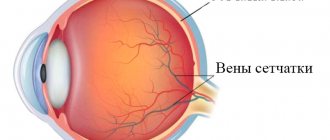
In AMD, the pathological process is localized in the central zone of the retina; as a rule, the disease affects both eyes at once and has a slow, long-term course with steady progression.
Delay in seeking the necessary help due to a long asymptomatic course of the pathological process, and sometimes incorrect diagnosis of the disease, lead to loss of professional skills and performance. At the same time, in patients of working age, primary disability due to AMD is about 21%.
Factors contributing to the occurrence of the disease, experts include:
- Age-related changes in the body in people over 50 years of age;
- Heredity;
- Arterial hypertension;
- Light skin and light (usually blue) iris color;
- Smoking;
- Oxidative stress reactions;
- Lack of vitamins and antioxidants in the body, deficiency of carotenoids in the macula;
- High level of solar radiation.
In addition, a clear relationship with the occurrence of age-related macular degeneration was revealed in cases of damage to the carotid arteries by atherosclerotic plaques, diabetes mellitus, excess body weight, and metabolic disorders.
Clinical experience shows that older women (60 years and older) suffer from AMD twice as often as their male peers.
Macular degeneration
What is AMD?
Age-related macular degeneration (AMD), or macular degeneration, is a disease that affects the central, most important area of the retina - the macula, which plays a key role in vision.
Age-related macular degeneration is the leading cause of irreversible vision loss and blindness among people aged 50 years and older in the developed world. Because people in this group represent a growing proportion of the population, vision loss from macular degeneration is a growing problem.
According to WHO, the share of the population of the older age group in economically developed countries is about 20%, and by 2050. will probably increase to 33%. Accordingly, due to the expected increase in life expectancy, the steady increase in atherosclerosis and concomitant pathologies, the problem of AMD remains the most pressing. In addition, in recent years there has been a clear trend toward “rejuvenation” of this disease.
The cause of decreased vision is degeneration of the macula, the most important area of the retina, responsible for the sharpness and acuity of central vision necessary for reading or driving a car, while peripheral vision is practically unaffected. The socio-medical significance of this disease is due precisely to the rapid loss of central vision and loss of general performance. The severity of the process and loss of central vision depends on the form of AMD.
Dry and wet forms of AMD
Intense metabolism in the retina leads to the formation of free radicals and other reactive oxygen species, which can cause the development of degenerative processes when the antioxidant system (AOS) is insufficient. Then, in the retina, especially in the macula and paramacular region, under the influence of oxygen and light, non-cleavable polymer structures are formed - drusen, the main component of which is lipofuscin.
With the deposition of drusen, atrophy of the adjacent layers of the retina occurs and the growth of pathological newly formed vessels in the retinal pigment epithelium is noted. Subsequently, scarring processes occur, accompanied by the loss of a large number of retinal photoreceptors.
Ophthalmologists distinguish two variants of the course of this disease - dry (non-exudative, atrophic) and wet (exudative, neovascular) forms of AMD.
The dry form of AMD is more common than the wet form and is detected in 85% of all cases of AMD. Yellowish spots known as drusen are diagnosed in the macular area. The gradual loss of central vision limits patients' ability to see fine details, but it is not as severe as in the wet form. However, dry AMD can slowly progress over several years to the late stage of geographic atrophy (GA), a gradual degradation of retinal cells that can also lead to severe vision loss.
There is currently no definitive treatment for dry AMD, although some are currently in clinical trials. A huge number of clinical studies have proven that certain nutrients such as beta-carotene (vitamin A), vitamins C and E can help prevent or slow the progression of dry macular degeneration. Research shows that taking high doses of certain eye supplements and vitamins can reduce the risk of developing early-stage AMD by 25%. Eye doctors also recommend that patients with dry AMD wear sunglasses with UV protection.
The wet form of AMD is present in approximately 10-15% of cases. The disease progresses quickly and often results in significant loss of central vision, with dry AMD progressing to more advanced and damaging forms of the eye disease. In wet AMD, the process of new blood vessels growing (neovascularization) begins. The wall of such vessels is defective and allows blood cells and fluid to pass through, which accumulate in the space under the retina. This leakage causes permanent damage to the light-sensitive cells in the retina, which die and create blind spots in central vision.
Choroidal neovascularization (CNV) underlies the development of wet AMD. Abnormal vascular growth is the body's faulty way of creating a new network of blood vessels to ensure the required amount of nutrients and oxygen reaches the retina. Instead of this process, scarring occurs, resulting in severe loss of central vision.
Causes and risk factors for developing AMD
Despite numerous studies on AMD, the causes of this disease remain unclear to date. AMD is a multifactorial disease.
Age is the main reason. The incidence increases sharply with age. Among middle-aged people, this disease occurs in 2%, at the age of 65 to 75 years it is diagnosed in 20%, and in the group from 75 to 84 years, signs of AMD are found in every third person. A significant portion of the population has a congenital predisposition to AMD, but there are a number of factors that either contribute to the onset of the disease or prevent it.
A number of risk factors have been proven that negatively affect natural protective mechanisms and therefore contribute to the development of AMD, the most significant are:
- Race – the highest prevalence of AMD is observed in Caucasians
- Heredity - Family history is an important risk factor in 20% of patients with AMD. A threefold increase in the risk of developing AMD has been established if the disease occurs in relatives in the first generation
- Cardiovascular disease plays a significant role in the development of AMD. It has been established that with atherosclerosis, the risk of damage to the macular area increases by 3 times, and in the presence of hypertension – by 7 times.
- Cigarette smoking is the only risk factor whose significance was confirmed in all studies. Quitting smoking reduces the risk of developing AMD.
- Direct exposure to sunlight
- Diet—The risk of AMD is higher in people who eat more saturated fat and cholesterol, and who are overweight.
- Light iris
- Cataracts, especially nuclear ones, are a risk factor for the development of AMD. Cataract surgery may contribute to the progression of the disease in patients with existing changes in the macular area.
Symptoms of AMD
Age-related macular degeneration usually causes slow, painless, and irreversible vision loss. In rare cases, vision loss can be severe.
Early signs of vision loss from AMD include:
- appearance of dark spots in central vision
- blurred image
- distortion of objects
- deterioration in color perception
- sharp deterioration of vision in poor lighting and darkness
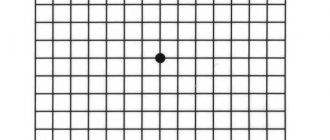
The most basic test for determining the manifestations of AMD is the Amsler test. The Amsler grid consists of intersecting straight lines with a central black dot in the middle. Patients with symptoms of AMD may see that some lines appear blurred or wavy, and dark spots appear in the field of vision.
An ophthalmologist can distinguish the manifestations of this disease even before changes in the patient’s vision develop and refer him for additional examinations.
Diagnosis of AMD
Diagnosis of AMD is based on medical history, patient complaints, assessment of visual functions and data from examination of the retina using various methods. Currently, fundus fluorescein angiography (FAGD) is recognized as one of the most informative methods for detecting retinal pathology. To conduct FAHD, various models of cameras and special contrast agents - fluorescein or indocyanine green - are used, which are injected into the patient’s vein, and then a series of fundus photographs are taken.
Stereoscopic images can also be used as a baseline for dynamic monitoring of a number of patients with severe dry AMD and patients during treatment.
OCT (optical coherence tomography) is used to finely assess changes in the retina and macula, which makes it possible to detect structural changes at the earliest stages of retinal degeneration.
Treatment of dry and wet forms of AMD
Despite enormous strides in improving diagnostic methods for AMD, its treatment remains a rather difficult problem. In the treatment of dry forms of AMD and with a high risk of developing the disease, courses of antioxidant therapy are recommended in order to normalize metabolic processes in the retina.
According to the AREDS study, the beneficial effect of taking antioxidants was achieved in those participants who had intermediate or late stage AMD in at least one eye. Combination therapy with antioxidants, zinc and copper over 5 years reduced the incidence of late-stage AMD by 25%, and the risk of loss of visual acuity of 3 or more lines by 19%.
It should be remembered that replacement therapy for the prevention and treatment of dry AMD cannot be a course; its use is possible only on an ongoing basis. It should be used in people over 50 years of age, and in the presence of risk factors (smoking, overweight, severe medical history, cataract extraction), then even earlier.
Treatment of wet AMD is aimed at suppressing the growth of abnormal blood vessels. Today, there are a number of drugs and techniques registered in Russia that can stop or reduce the manifestations of abnormal neovascularization, which has improved vision in a significant number of people with wet AMD.
For more information, read our article “Treating Age-Related Maular Degeneration.”
Types and types of AMD
According to the type of course, age-related macular degeneration is divided into early and late phases, and according to the type of clinical manifestations available - into “dry” and “wet” forms.
In almost 90% of cases of the disease, it is the “dry”, non-exudative form of AMD, which has a slowly progressive course, that is diagnosed. The “wet”, exudative form of the disease occurs only in 10% of cases. This form of AMD is especially dangerous; it is accompanied by the phenomena of pathological choroidal neovascularization, which leads to a tragic drop in visual acuity.
The main provoking factor in the occurrence of AMD is retinal ischemia - a violation of blood circulation and nutrition. In this regard, the disease has two variants of its course:
- With the formation of friends. Drusen - deposits of yellowish-gray lipids are usually detected symmetrically in both eyes, as thickenings under the retinal pigment epithelium (RPE). Their number, shape and size can vary, as well as the degree of prominence with the severity of changes in the RPE. An increase in the number of drusen and an increase in their size often leads to fusion and the appearance of choroidal neovascularization. This is explained by the active synthesis of vascular endothelial growth factor, which acts as a powerful stimulator of angiogenesis. Initially, newly formed vessels can grow under the RPE, causing its detachment. Over time, perforation of the RPE occurs, leading to detachment of the neuroepithelium. The progression of the process causes the formation of a choroidal neovascular membrane, the amount of connective tissue increases and a fibrous scar appears as an outcome of AMD.
- With the occurrence of atrophy. This flow option leads to extensive so-called. geographic involution of the pigment epithelium localized in the macular zone of the retina. In rare cases, choroidal neovascularization may occur in the later stages of the pathological process.
Treatment of the “wet” form of macular degeneration
Age-related macular degeneration is treatable as long as the disease has not reached the terminal stage. The goal of the treatment is to stop the progression of changes in the retina and maintain visual acuity. Previously, when identifying AMD, the main efforts were aimed at combating the consequences of the disease - the growth of defective blood vessels and the leakage of the liquid part of the blood. To do this, pathological vessels were “cauterized” using a medical laser (laser coagulation of the retina). The effect of this treatment was temporary. Currently, to treat age-related macular degeneration, along with laser coagulation, intraocular (intravitreal) injections of drugs that prevent the growth of pathological blood vessels (anti-VEGF) are used.
Intravitreal administration of anti-VEGF drugs targets a protein that causes the growth of abnormal retinal vessels. This treatment makes it possible to delay the progression of the disease for many years and significantly improve the quality of life of patients, and in some cases, slightly increase the visual acuity of a patient with macular degeneration.
Despite the high effectiveness of intravitreal injections of anti-VEGF drugs, they only work until the formation of rough scars on the retina and significant loss of vision. If you have been diagnosed with AMD, visit your doctor regularly and do not delay treatment to avoid losing your vision!
During an intravitreal injection, the doctor uses a special needle to inject the drug into the eye cavity, into the vitreous body. Injections are performed using sterile instruments in an operating room; they can only be done by a doctor who has undergone special training and is proficient in the technique of intraocular injections. The administration procedure is carried out after instillation of anesthetic drops and is not accompanied by pain.
The anti-VEGF drug, entering the eye cavity, blocks the release of endothelial vascular growth factor, as a result of which new abnormal vessels do not appear, already formed pathological vessels become empty and collapse, and fluid (exudate) is absorbed. Thus, it is possible not only to combat existing symptoms of the disease, but also to prevent their occurrence, and in some cases, to improve visual acuity.
For intravitreal administration for AMD, the drugs most often used are Lucentis and Eylea, and some clinics may also use Macugen or Avastin. The latter is not registered in the Russian Federation for use in ophthalmology.
Lucentis was the first drug developed to treat wet macular degeneration. A few years later, the drug Eylea was also used for the treatment of AMD, which has a longer therapeutic effect.
Fig.4 Intravitreal injection - the injection is made directly into the vitreous body of the eye
In our “Retina Center” we use only Lucentis and Eylea drugs, certified for the treatment of exudative forms of macular degeneration. The injections are carried out by experienced doctors who are fluent in the technique of intravitreal drug administration.
Lucentis injections are performed according to the following scheme: 0.05 ml of the drug intravitreally once a month. Typically, three injections are given with an interval of 30 days (to accumulate the drug in the eye cavity), after which the doctor needs to evaluate the effect of the drug and select an individual treatment regimen in the future. Treatment with Eylea is carried out according to a similar scheme: three intraocular injections of 2 mg each with an interval of 30 days, then injections are performed once every two months (or less often).
To speed up the removal of edema and improve the blood supply to the retina, courses of vascular medications and physiotherapeutic treatment can be prescribed (including at home - the AMBO-01 device).
Clinical picture
In the “dry” form of AMD with the formation of drusen (hard or soft), the course of the disease is not accompanied by significant visible and functional impairments. Most patients retain fairly high (0.5 or higher) visual acuity. At the same time, drusen are considered to be a risk factor for neovascularization in AMD.
The “wet” form of AMD, unlike the “dry” one, progresses much faster and almost always occurs in people already suffering from the “dry” form of the disease.
“Wet” AMD is characterized by the following symptoms:
- Weakening of vision (with “dry” AMD, vision deterioration occurs gradually, in the case of “wet” AMD - sharply).
- Difficulty reading, lack of improvement with glasses correction.
- Poor image contrast, blurred vision.
- Curvature of lines and falling of letters when reading.
- Metamorphopsia is a distortion of the shape of objects.
- Scotomas are the appearance of dark spots in the field of vision.
It is “wet” or exudative AMD that in 90% of cases leads to partial blindness. This form of the disease is accompanied by the growth of newly formed abnormal vessels. Such vessels from the choriocapillaris layer in the choroid through the perforation of Bruch’s membrane grow under the RPE and/or neuroepithelium. According to experts, this situation is a factor in the formation of the subretinal neovascular membrane located under the retina.
The newly formed vessels have abnormally permeable, weak walls, through which the liquid component of the blood begins to ooze, leaving accumulations of lipid deposits and cholesterol under the retina. Quite often they rupture with the occurrence of local (rarely large in volume) hemorrhages. These processes lead to disruption of blood circulation and nutrition of the retina, and provoke the occurrence of fibrosis. As a result of “wet” AMD, a subretinal scar occurs, which exposes the retinal tissue to such severe changes that it ceases to perform its functions.
Age-related macular degeneration cannot lead to absolute blindness. During the course of the disease, only central vision is gradually lost, as an absolute scotoma (dark, opaque spot) occurs. Peripheral vision remains intact, since the pathological process affects only the macular region of the center of the retina. Patients with AMD see with “lateral vision” and its acuity to the outcome of the process, as a rule, does not exceed 0.1 (first line of the table).
The course of the pathological process of AMD is absolutely individual for each patient, however, when a subretinal neovascular membrane occurs, it becomes very important to receive timely medical care. Early diagnosis and timely adequate treatment of this condition in most cases allows one to preserve visual functions and achieve long-term remission or reverse development of the process.
Symptoms of “wet” macular degeneration
The “wet” form of AMD is characterized by progressive deterioration of central vision and irreversible damage to the macular area. Painful sensations do not appear even in an advanced stage. Eye involvement is usually bilateral, but changes in one eye may progress more quickly. The patient does not notice a clear decrease in vision for some time, because the healthier eye takes on all the visual load and compensates for the deterioration of vision in the second eye.
As more and more cells in the macula are destroyed, vision quickly deteriorates and cannot be corrected with glasses. A blurry spot appears in the center of the visual field, which quickly increases in size and darkens. It becomes difficult for a person to read, write, distinguish faces, and he cannot perform work that requires examining small details. Surrounding objects may be perceived in a distorted form, with curved contours.
Diagnosis of AMD
A number of signs of age-related macular degeneration may appear before the immediate deterioration of vision. And yet, only an ophthalmological examination makes it possible to detect them in a timely manner and take appropriate measures for treatment.
Today, a whole arsenal of traditional and innovative diagnostic methods is used to diagnose AMD. These include:
- Visometry with tables to establish visual acuity.
- Ophthalmoscopy with instrumental examination of the fundus.
- Visocontrastometry with an accurate assessment of the visual analyzer.
- Computer perimetry with the study of residual visual fields.
- Fluorescein angiography to evaluate retinal vessels.
- Optical coherence retinotomography, to obtain optical sections of any part of the fundus.
- Color stereo photography.
For patients diagnosed with AMD, one of the most informative tests for self-monitoring is the Amsler Grid. This test is designed to detect the initial stages of macular edema that occurs with choroidal neovascularization.
Diagnosis of age-related macular degeneration
The examination begins with standard diagnostic procedures (determining visual acuity, examining the fundus, measuring the visual field). If characteristic changes are detected in the retina, an extensive vision examination is prescribed, including the diagnostic methods listed below.
Optical coherence tomography (OCT, OCT) allows non-invasively, that is, without penetrating into the eye cavity with the help of any instruments, to obtain intravital sections through the entire thickness of the retina and thus evaluate its structure. The method allows you to identify drusen, abnormal vessels, macular edema and other changes.
Fluorescein angiography (FA) helps to visualize altered retinal vessels and determine which treatment method will be most effective (laser coagulation, intravitreal injections, photodynamic therapy).
Perimetry is a technique that allows you to assess the state of the visual field. Since macular degeneration is characterized by damage to central vision, perimetry can identify areas of loss of visual fields (scotomas).
The Amsler test (grid) is a simple and informative method that allows you to identify a characteristic symptom of the “wet” form of macular degeneration - curvature of lines. The Amsler grid looks like thin intersecting horizontal and vertical lines. A patient with exudative AMD sees the lines in the drawing as uneven, broken, or pale. The larger the area of the macula involved in the pathological process, the more distorted the lines will appear when tested.
Indocyanine green angiography (ICGA) , like FA, requires intravenous administration of a contrast agent. After some time, a series of sequential photographs of the retina are taken in infrared light. This diagnostic procedure allows you to determine changes in the retina that are not detected by FA.
Treatment
It is advisable to approach the treatment of age-related macular degeneration using a set of basic principles of modern medicine: timeliness, differentiation (depending on the stage and form of the disease), duration (sometimes for the rest of life), complexity (therapeutic and surgical treatment methods).
Therefore, treatment should include:
- Drug therapy: vitamins and antioxidants, peptide bioregulators and angeogenesis inhibitor drugs.
- Laser treatment: retinal laser coagulation, photodynamic therapy.
- Surgical treatment: vitrectomy with removal of SNM, transplantation of retinal pigment epithelium (in clinical trials).
People who have reached 55-60 years of age should take into account that if distance visual acuity deteriorates, the outlines of visible objects are distorted, letters fall out when reading and lines are distorted, as well as if difficulties arise with vision at night, it is necessary to immediately consult an ophthalmologist . When a disease is detected, it is worth conducting independent monitoring of visual functions using the Amsler test. Adhere to medication therapy prescribed by a specialist.
The availability, simplicity and low cost of the method of intravitreal administration of Kenalog has made it widespread in vitreomacular surgery. It is applicable for macular edema of various natures and those caused by “wet” AMD, including. This method is quite effective and leads to a rapid reduction in swelling, but even its single use is fraught with serious complications.
The last decade has marked the beginning of a new era in the treatment of age-related macular degeneration. Now, drugs that inhibit (suppress) the production of vascular endothelial growth factor (VEGF2) are successfully used to treat this disease. Of course, the reasons for the formation of the subretinal neovascular membrane in AMD today have not yet been fully elucidated, however, studies conducted in recent years indicate a direct connection between its development and VEGF. Angiogenesis inhibitor drugs are now the method of choice in the treatment of age-related macular degeneration, because they show the best results in terms of preserving the visual acuity of patients.
Why does macular degeneration develop?
The trigger point for the development of macular degeneration is changes in the retinal vessels, which are responsible for the normal supply of nutrients to the retinal cells. If the delivery of nutrients to the retinal tissues is disrupted, its cells begin to experience oxygen starvation, which triggers a cascade of pathological reactions here.
Among the main causes of AMD is age. Despite the fact that degenerative changes in the macula are also found in middle-aged patients, the main group of patients with AMD consists of people over the age of 60 years. Other factors contributing to the development of AMD are hereditary predisposition, overweight and obesity, and bad habits (smoking). The disease is statistically more often detected in women with white skin color.
Prevention of AMD
When diagnosing the early stages of age-related macular degeneration and/or with an existing genetic predisposition to it (cases of AMD in the family), it is necessary:
Undergo a comprehensive ophthalmological examination every 2-4 years, from 40 to 64 years, if there is a genetic predisposition to the disease. And starting from the age of 65, visit an ophthalmologist at least once a year to examine visual functions for AMD.
It is always worth remembering that only early detection and competent treatment of AMD will help slow down and stop vision deterioration, which will maintain a high quality of life in the future.
Causes of AMD development
The causes of the disease still remain unclear. But scientists suggest that the following factors may lead to its development:
- Age is the main reason. The incidence increases rapidly with age. Signs of AMD occur in 2% of middle-aged people, in 20% of elderly people aged 65-75 years, and in every third person after 75-80 years.
- Genetic predisposition to the development of the disease, but there are factors that contribute to either the occurrence of the disease or its prevention.
- Race - the prevalence of macular degeneration is more common among Caucasians.
- Heredity (family predisposition) is one of the risk factors in almost 20% of patients with age-related macular degeneration. The risk of AMD increases threefold when the disease occurs in close relatives.
- Cardiovascular disease is one of the main risks for the development of AMD. With atherosclerosis, the risk of the disease increases three times, and with hypertension – seven times.
- Cigarette smoking is the only risk factor confirmed in all studies. Quitting this habit reduces the risk of developing the disease.
- Impact of UV rays on the retina of the eye.
- Poor diet - The risk of AMD is significantly higher in people who eat a lot of saturated fat and have increased body weight.
- Light iris. People with light irises (blue, gray, green eyes) suffer from AMD more often.
- Cataract, especially nuclear. Cataract surgery often contributes to the progression of the disease in people with existing changes in the macula.