Treatment of proliferative processes in the retina involves suppression of vascular endothelial growth factor (VEGF: vascular endothelium growth factor) in the case of diagnosing neovascularization of the retina. A similar condition is often detected in diabetic retinopathy, wet form of macular degeneration, and also after venous thrombosis. This stops the growth of new pathological vessels with high wall permeability. VEGF inhibitor drugs are considered by modern medicine as an addition to laser treatment and the use of triamcinolone in patients with macular degeneration.
The introduction of intravitreal injections of VEGF inhibitors into clinical practice has made it possible to use new methods of treating macular degeneration. The use of anti-VEGF therapy as the only treatment method, or its combination with LCS, makes macular edema less pronounced and helps improve visual acuity. Today, ranibizumab (Lucentis) is officially registered for the treatment of AMD. It is prescribed for macular edema, which has caused decreased vision, when the thickness of the macular zone of the retina is more than 300 microns. Positive results of randomized studies of the use of bevacizumab, pegaptanib, and aflibercept prove their high effectiveness. Clinical trials are currently planned to compare the effectiveness of these drugs in the treatment of macular degeneration.
For the administration of anti-VEGF drugs, the intravitreal method is considered the most appropriate, since it is most effective in delivering the substance directly to the retina. With this method of administration, a larger percentage of the active substance (up to 51%) remains in the vitreous body, up to 13.2% of the total dose reaches the retina and choroid. If another method of administration is used - subconjunctival, sub-Tenon, then up to 5.3% of the administered dose is delivered to the internal structures of the eye (vitreous body, retina, choroid).
Pathogenesis of diabetic retinopathy
The leading component that affects blood vessels in diabetes mellitus is constant hyperglycemia, that is, high levels of glucose in the blood. This condition leads to the launch of a whole system of pathological processes at the pathophysiological, biochemical and molecular genetic level. As a result, damage to the retina occurs.
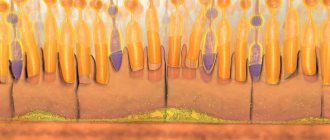
In the process of damage to the endothelial lining of retinal vessels, mechanisms are activated that enhance the synthesis of substances (cytokines, growth factors, extracellular matrix proteins) involved in cell death (through dysfunction and apoptosis). As a result of all these transformations, desolation of the vascular bed and increased filtration of blood components occurs. In addition, hemorrhages occur and pericytes die. As a result of damage to the vascular network, retinal hypoxia develops.
In response to a lack of oxygen, protein synthesis increases in retinal cells, which ultimately leads to an increase in the amount of VEGF. This substance is released into the extracellular space and affects epithelial cells. The latter begin to rapidly divide and potentiate the formation of new vessels.
Vascular endothelial growth factor in normal and pathological conditions
The VEGF protein was first isolated back in 1983. Its main goal was to increase the permeability of the vascular wall of the arteries located in the tumor node. This protein belongs to the glycoproteins and has structural similarities to platelet growth factor. It contains five types of receptors (with tyrosine kinase activity), that is, VEGF can be influenced by the processes of embryogenesis, pregnancy, wound healing, tumor growth, reproductive function in women, the development of coronary disease and diabetic retinopathy.
The VEGF-A protein has been studied to the greatest extent. This substance has several isoforms, but its main effect on cells is through the tyrosine receptor, which is located in the membrane structure. With intravitreal administration of the VEGF 165 blocker, a significant slowdown in the processes of pathological neovascularization occurs, while the effect on physiological vascularization was practically absent or insignificant.
In addition, VEGF is involved in embryogenesis and early angiogenesis. In adults, endothelial growth factor acts in two ways in the vascular wall: on the one hand, it promotes the survival of endothelial cells, on the other, it stimulates vascular permeability and causes dilation of the lumen of the arteries. For example, in the kidneys, VEGF controls the functioning of the filtration system and is responsible for glomerulogenesis. In addition, this protein affects the regeneration of muscle cells, the restructuring of the myocardium and causes the formation of bone tissue inside the cartilage.
In addition to physiological processes, VEGF leads to the launch of several other beneficial mechanisms. These include the growth of collateral vessels in response to hypoxia, as well as improved tissue nutrition during wound healing.
In patients with diabetes, VEGF is secreted by retinal pigment epithelial cells, resulting in the growth of new blood vessels and retinal edema. Type 1 diabetes is characterized by neovascularization processes, while type 2 diabetes is more likely to cause retinal edema, which leads to loss of central vision.
Cochrane
What is the purpose of this review?
The aim of this review was to find out whether treatment with vascular endothelial growth factor inhibitors (called anti-VEGF) prevents vision loss when new blood vessels form in people with severe myopia (nearsightedness). To answer this question, Cochrane researchers collected and analyzed all relevant studies and found six studies.
Key information
People with severe myopia and new blood vessels forming (growing) in the back of the eye (retina) may benefit from treatment with vascular endothelial growth factor (anti-VEGF) inhibitors. This treatment can prevent vision loss. Side effects (harm from treatment) are rare.
What was learned in this review?
With myopia, the eyeball becomes too long. With severe myopia, sometimes the retina (the light-sensitive tissue at the back of the eye) becomes very thin and new blood vessels begin to form (grow) in it. These newly formed blood vessels can leak fluid and blood, which can cause vision loss.
Vascular endothelial growth factor (anti-VEGF) inhibitors are medications that can slow the growth of these new blood vessels. Doctors may inject anti-VEGF into the eyes of people with severe myopia and signs of new blood vessels growing in the back of the eye. This may prevent vision loss.
What are the main findings of this review?
Cochrane researchers found six relevant studies. These studies were conducted at clinical sites on three continents (Europe, Asia and North America). Three studies compared anti-VEGF treatment with photodynamic therapy (PDT, a treatment using a light-sensitive drug and light source that destroys abnormal cells); one study compared anti-VEGF with laser treatment; another study compared anti-VEGF treatment with no treatment, and two other studies compared different anti-VEGFs with each other. In some studies, people in the comparison group received anti-VEGF after a short period, meaning the results may underestimate the benefit of anti-VEGF.
The results of this review showed that:
• People with severe myopia who have received anti-VEGF treatment are likely to achieve better vision than people treated with PDT, laser treatment, or no treatment (low to moderate certainty of evidence). • Two different types of anti-VEGF, ranibizumab and bevacizumab, are likely to have similar effects on vision (moderate certainty of evidence). • Side effects (harm from treatment) are rare.
How relevant is this review?
Cochrane researchers searched for studies published up to 16 June 2021.
VEGF inhibitors
Anti-VEGF drugs are used for tumor metastasis as an additional therapy. Vascular growth factor inhibitors are monoclonal antibodies that precisely bind to VEGF receptors, causing vascular endothelial growth factor to stop working. By suppressing the growth of blood vessels, they prevent further spread of tumor tissue.
Recently, scientists have identified the role of VEGF in the development of diabetic retinopathy. In this regard, drugs from their anti-VEGF group began to be used for the conservative treatment of patients.
In practical medicine, several drugs that belong to this group are used: penaptanib (selectively blocks VEGF 165), ranibizumab, bevacizumab (non-selective blocker of all isoforms).
Pegaptinib (Macugen) has the greatest affinity for the VEGF 165 protein isoform. Experimental studies have found that its intravitreal administration reduces the degree of neovascularization, leukostasis and mediated cellular hyperfiltration. An American organization approved the use of this drug in patients with age-related macular degeneration back in 2004.
Ranibizumab (Lucentis) is specifically designed to treat age-related macular degeneration. Unlike the previous drug, it affects all isoforms of human VEGF. In an experimental study on monkeys, it was found that intravitreal administration of Ranibizumab reduced neovascularization and the permeability of existing vessels. In 2006, the American committee approved the use of Ranibizumab for the edematous form of age-related macular degeneration.
Bevacizumab (Avastin) was synthesized from mouse antibodies. It acts non-selectively and blocks all VEGF isoforms. This drug has already begun to be used to treat wet age-related macular degeneration, but it is still officially approved for use in ophthalmology.
Results of clinical studies on the use of anti-VEGF drugs
Systemic intravenous administration
This route of administration of anti-VEGF drugs has been studied in only one study. In this case, Bevacizumab at a dose of 5 mg/kg was used to treat 18 patients suffering from a neovascular form of age-related macular degeneration. The number of drug administrations was 1, 2, 3 with an interval of two weeks. The study was uncontrolled.
Already two weeks after the start of the study, an increase in visual acuity was noted. The parameters remained at a high level throughout the entire observation period (24 weeks). There was also a decrease in retinal thickness at the end of observation. Despite such a high effectiveness of the drug, the work did not study possible side effects.
Intravitreal administration
Large clinical trials have examined the activity of pegaptanib and ranibizumab when administered intravitreally. As a result, it was found that the activity of ranibizumab exceeds that of pegaptanib. However, the number of side effects in the latter case is also less. Among the adverse effects of ranibizumab, the most important are pathologies of the heart and blood vessels (including stroke), and a tendency to bleeding.
These drugs have also been studied in patients with diabetes. One large study (multicenter, double-blind) included 172 patients with biabetic macular edema. Patients treated with pegaptanib had significantly better visual function at the end of the study (36 weeks) than the comparison group. In addition, the thickness of the central zone of the retina was lower, and laser treatment had to be resorted to less frequently. In modern clinical ophthalmology, Bevacizumab is used for preoperative preparation before vitrectomy for proliferative diabetic retinopathy.
Anti-VEGF therapy regimens
For diabetic macular edema, for example, monthly injections for 3 or 6 months are most effective.
If the disease progresses, the course of treatment can be continued for a longer period. During therapy, the patient is examined monthly by an ophthalmologist with mandatory optical coherence tomography (OCT), after which the course of treatment is adjusted. Treatment requires a strictly individual approach, so the exact regimen is selected for each patient. When treating wet AMD, it is recommended to adhere to the following regimen: for 3 months, injections are given monthly, once a month. Next, the doctor observing the patient determines the subsequent treatment plan. Dedov I.I. Complications of diabetes. – M.: Medicine, 1995. Katsnelson L.A. et al. Vascular diseases of the eyes. – M.: Medicine, 1990. Balashevich L.I. et al. Modified clinical classification of age-related macular degeneration. Ophthalmological bulletins, 2011. Neroev V.V. et al. "Local and systemic production of VEGF-A in complicated proliferative diabetic retinopathy." Medical Immunology, 2021.
Possible side effects of anti-VEGF administration
Systemic side effects
Anti-VEGF drugs are administered directly into the vitreous through the sclera. Despite this, part of the drug may penetrate into the systemic circulation. As a result, various undesirable consequences may occur. Among the systemic effects of VEGF inhibitors, attention should be paid to hypertension and proteinuria. Most often, these changes occur during treatment of cancer. Hypertension occurs due to an increase in peripheral vascular resistance due to inhibition of nitric oxide synthesis by endothelial cells (normally stimulated by VEGF). Kidney function is also impaired, which can cause increased blood pressure. Other symptoms of the systemic influence of anti-VEGF include infertility, myocardial remodeling, inhibition of regenerative processes in muscle tissue, disruption of regeneration processes, development of bleeding and the wall of the stomach or intestine, disruption of the formation of collaterals.
All of the listed systemic side effects are especially dangerous for patients with diabetes.
Ophthalmic complications
With intravitreal administration of VEGF inhibitors, the following local complications most often occur: retinal detachment, lens damage, endophthalmitis. Such deviations are not common, and the risk of complications is higher in patients with diabetes because they require continuous treatment over several years.
In addition to the reaction to intravitreal administration, complications directly related to the action of VEGF antagonists may occur. This protein, normally synthesized by retinal pigment epithelial cells, promotes neuroprotection of photoreceptors and is also responsible for the development of choriocapillaris. If the selective VEGF blocker pegaptanib is used, the number of retinal ganglion cells does not decrease.
Intravitreal administration of the non-selective VEGF blocker bevacizumab also failed to detect a toxic effect on retinal ganglion cells. Despite the lack of confirmation of a damaging effect on the retina, light microscopy revealed destruction of mitochondria in the inner segment of the photoreceptor layer. Also, experimental work on rodents revealed an increase in apoptosis as a result of intravitreal administration of bevacizumab. Currently, scientists continue to search for selective anti-VEGF drugs that would not affect the neuroprotective effect of this protein.
Ophthalmic complications of anti-VEGF therapy
The use of anti-VEGF drugs in the treatment of ophthalmological diseases can lead to a number of pathological conditions: retinal detachment, increased intraocular pressure, endophthalmitis, and damage to the lens. According to available research data, the frequency of such complications is no more than 1–1.5% of all cases of therapy. Systemic side effects are also rare. Sometimes there are: increased blood pressure, myocardial infarction, stroke, proteinuria.
Experts associate such reactions with some amount of the drug entering the bloodstream. There is evidence that after intravitreal administration of bevacizumab, its level in the bloodstream gradually decreases over the course of a month, and after the administration of ranibizumab and pegaptanib, it remains unchanged.
Another study, currently initiated, aims to assess the degree of penetration of VEGF inhibitors into the bloodstream during intravitreal injections. In addition, the objective of the study will be to assess the safety of such drugs in patients with serious diseases: diabetes mellitus, macrovascular pathologies, high rates of arterial hypertension, and nephropathy. Subsequent studies will determine the optimal duration of therapy with anti-VEGF drugs and the advisability of combination with other treatment options for AMD.
In our clinic, highly effective drugs approved by the Ministry of Health are used for anti-VEGF therapy. The experience and professionalism of doctors, as well as adherence to advanced treatment methods, allow us to achieve high therapeutic results without possible complications and side effects.