Currently, more and more people are complaining of vision problems. One of the most common ophthalmological pathologies is myopia (myopia). According to statistics, ten percent of the population suffers from this disease. The causes of myopia can be very different, let's look at them.
Introduction
Translation provided by Andrey Noskov.
This review is based on a lecture by David Yosem and adapted for Radio Lodge by assistant Robin Smithwis. David Yosem is a professor of radiology at Johns Hopkins Hospital and currently serves as chief of the Division of Neuroradiology. He is also the editor of the book Neuroradiology: Everything You Need. This article reflects a systematic approach to orbital pathology; it is based on dividing the orbit into the following sections:
- Ocular space
- Intraconal space
- Conal space
- Extraraconic space
Anatomical features
First, when you see orbital pathology, you need to determine whether the eyeball itself is involved or whether structures outside of the eyeball are involved. If the lesion is not associated with the eyeball, the next question you must answer is whether the pathology is in the intraconal space, that is, in the space limited by the conus of the extraconal muscles, or whether the lesion is located in the conal and ectraconal spaces.
We must first describe the anatomical spaces of the orbit and summarize the pathologies within these spaces, even if some of these pathologies are not visible radiographically.
And only then will we discuss the radiological signs of some orbital diseases.
Reasons for development
Atrophy of the eyeball occurs due to the following factors:
- traumatic injury;
- acute or chronic inflammation;
- detachment of the ciliary body;
- immune lesions;
- change in the permeability of the hemo-ophthalmic barrier.
Eye injuries are in first place as the cause of this disease because it is mechanical damage that is most often the source of the problem. If there is any impact on the eye, you must immediately seek help, since slowing down can lead to irreversible consequences: complete blindness and neuroretinitis.
Ocular space
The eyeball has the following clearly demarcated anatomical spaces:
The anterior chamber is bounded by the cornea in front and the lens along with the iris behind. Pathology within the anterior chamber:
- Eyeball rupture
- Hemorrhage: also known as anterior hyphema
- Cataract
- Keratitis: inflammation of the cornea
- Periorbital cellulite
Posterior chamber This is a very small area behind the iris that we cannot see during examination. Pathology within the posterior chamber:
- Glaucoma
- Uveitis
- Ciliary melanoma.
Vitreous humor A gel-like, gelatinous, clear substance that fills the space between the lens and retina in the eye. Pathology within the vitreous:
- Gap
- Hemorrhage
- CMV infection: especially associated with HIV
- Persistent hyperplasia of the primary vitreous
- Interventions for retinal detachment leading to changes in vitreous density
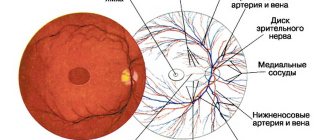
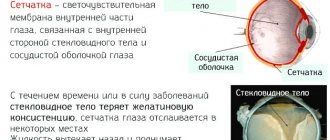
The vitreous body is surrounded by membranes: the retina, the choroid (choroid) and the sclera.
Retinal pathology:
- Retinoblastoma: a common tumor in children
- Hemangioblastoma: the most common retinal tumor in adults and is associated with Hippel-Lindau disease
- Detachment: The most common retinal lesion is mainly considered in diabetic retinopathy
Pathology of the choroid (choroid):
- Melanoma: The choroid contains melanin cells
- Metastases: the choroid is the most blood-supplied structure of the eye
- Detachment: usually post-traumatic
Pathology of the sclera:
- Infection: either due to sinusitis or viral
- Pseudotumor
- Detachment
Classification
There are three categories of disease:
- early – formed in young people due to damage to the tissues and bones that surround the eyeball (recession of the eyes occurs immediately after injury or after some time);
- late - formed as a result of various damage to the organs of vision, which lead to a decrease in the functionality of the muscles around the eyes (in this case, the cause is inflammation, bleeding, damage to nervous tissue and nodes);
- false – the cause of the disease is not in the tissues surrounding the eye, but in diseases of the eyeball, as a result of which its reduction occurs.
The doctor needs to classify the disease in order to prescribe treatment. Each subtype of enophthalmos has its own list of medications and surgical treatments.
Intraconal space
The eye muscles inside the orbit form a muscle cone. They are connected by a dense tendon ring (annulus of Zinn), with which they form the conal space.
The intraconal space (marked by an arrow) is located in the muscle cone. It contains the optic nerve, blood vessels and cranial nerves III, IV and VI.
Pathology of the intraconal space:
- Vascular malformations
- Capillary hemangioma
- Optic nerve lesions: Neuritis: Multiple sclerosis
- Devic's disease
- Neuritis due to infection (eg, herpes zoster)
- Autoimmune (eg lupus)
- Drugs (eg ethambutol)
- Carotid-cavernous anastomosis
Extraconal space
Extraconal space is the area outside the muscle cone.
Pathology of the extraconal space:
- Abscess due to sinusitis
- Schwannoma from branches V1 and V2 of the trigeminal nerve
- Bone lesions: Fibrous dysplasia of the sphenoid wing
- Metastases
- Multiple myeloma
- Diseases of the eye appendages
Appendages of the eye
The lacrimal gland is located superolaterally along the anterior surface of the orbit. Diseases of the lacrimal gland can be divided into the following types:
- Granulomatous\lymphoid Sarcoidosis, pseudotumor, lymphoma, Sjögren's syndrome, Mikulicz's disease, tuberculosis
- Pleomorphic adenoma, glandular cystic carcinoma
- Epidermoid or dermoid
The secretion from the gland accumulates in the lacrimal sac, from which the tear enters the nasolacrimal duct, which opens in the nasal cavity under the inferior concha. In children, congenital obstruction of the lacrimal duct valves can lead to the formation of cystic cavities located medial to the orbit, a condition known as dacryocystocele. In adults, the cause of duct obstruction is a stricture associated with ethmoiditis or stones blocking the nasolacrimal duct. This will cause tearing or tearing. Drainage can be improved with balloon dilatation.
Who should not do eye exercises?
Eye training is the safest and most affordable way to help relax muscles and improve visual acuity. Gymnastics has contraindications. They need to be taken into account before starting exercises. Restrictions include:
- Retinal detachment – blood flow to the eyes during exercise can worsen the condition and cause a retinal tear;
- Inflammation and infectious diseases of the eyes - pain may increase during gymnastics;
- Recovery period after surgery - during rehabilitation, you should not rub your eyes. Exertion slows down the healing process.
To avoid harm to your eyes, you should consult your doctor before doing vision exercises. The ophthalmologist will give recommendations and calculate the permissible load on the visual apparatus, which will give positive results.
Pathology of the eyeball
Calcifications
In adults, the most common intraorbital calcification occurs at the attachment sites of the eye muscles.
Other typical calcifications occur in the optic nerve head in the inner part of the eyeball, also called the optic disc. They are usually asymptomatic, but when the ophthalmologist checks the eyes, it appears that the optic disc is swollen, i.e. pseudo-edema of the optic disc. In children, calcifications in the eyeball, until proven otherwise, mean retinoblastoma, even if they are bilateral.
Retinoblastoma
- 11% of all cancers in 1 year of life 1: 17,000-24,000 live births worldwide
- Everything is inherited
Retinoblastoma is one of the most common tumors during the first year of life. Other tumors in this age group: neuroblastoma, Wilms tumor, leukemias and teratomas. All cases of bilateral lesions are hereditary and result from a defect in the tumor suppressor gene (or tumor suppression gene) on chromosome 13. The disease that is mentioned in the differential diagnosis is very rare.
The image shows a 13-month-old girl with bilateral retinoblastoma.
Small retinoblastomas are subjected to various therapies (cryodestruction, laser photocoagulation, chemotherapy, brachytherapy, radiation therapy) in order to save the eye and avoid enucleation. If a patient is treated with radiation therapy, there is a 30% chance of secondary malignancy in the radiation field, due to the radiation but also due to a tumor suppression gene defect. Outside the radiation field there is an 8% chance of malignancy.
In descending order of frequency: osteosarcoma > other type of sarcoma > melanoma > carcinoma.
These patients are also at risk of developing pineal and sella tumors. The pineal gland is considered the "third eye", and the "third testicle", in the sense that in the pineal gland you can find retinoblastoma, i.e. tripartite retinoblastoma, or even germinoma. Always examine the brain in these patients and remember that 0-4 years is the peak age for retinoblastoma, and the pineal gland is not yet calcified, so any calcification in this area is suspicious for retinoblastoma.
The image shows a photo of another patient with retinoblastoma. This tumor is presented in this case as a large calcification. When retinoblastoma occupies more than half of the eyeball, in this case, enucleation must be performed.
Leukocoria (abnormal white retinal reflex)
Typically, light passing through the iris is reflected from the retina as red. With leukocoria, it is reflected in white. Retinoblastoma is usually detected through leukocoria, a symptom that occurs in two thirds of patients with retinoblastoma. Such children are usually too young to have visual complaints.
There are many causes of leukocoria:
- Persistent vitreous (25%), Coats disease (10%), Ocular toxocariasis (10%), Cataract (13%)
- Astrocytic hamartoma, medulloepithelioma (may calcify); None of the others cause calcification
- Leukocoria occurs in 56-72% of patients with retinoblastoma and is the most common cause of leukocoria in childhood
Melanoma
The image shows a photograph of an adult patient with a mass in the right eyeball.
The most common intraocular lesion in adults is melanoma (as in this case), followed by metastases.
Other formations (hemangiomas, fibroids and osteomas) are rare.
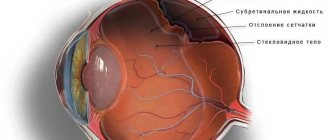
Persistent vitreous, hyaloid artery
The image shows another cause of leukocoria.
This is the persistent hyaloid artery of the vitreous body, here is the persistent hyaloid canal when the hyaloid artery does not heal. In the images we see a persistent canal that runs from the optic nerve to the lens. There is also retinal detachment (occurs in 30-55%) and note microphthalmia. Persistent primary vitreous hyperplasia is the second most common cause of leukocoria. These patients also suffer from glaucoma and cataracts.
Coats disease
Coats disease ( exudative retinitis
or
retinal telangiectasia ) is a rare disease of unknown etiology, leading to complete or partial blindness, characterized by abnormal development of blood vessels.
- Congenital, non-hereditary, unilateral vascular retinal telangiectasia
- Leakage of blood and lipids across the blood-retinal barrier
Leads to retinal detachment
- Ages 6-8, boys>girls, unilateral 90% of cases
- CT: increased density, normal size of the eyeball
- MRI: high signal d/t fat, hemoglobin breakdown products
Contusions of the eyeball
The CT image shows a patient who was urgently admitted to the hospital with post-traumatic orbital edema.
The patient has a rupture of the eyeball and, in particular, a rupture of the anterior chamber.
As radiologists, we are accustomed to looking at the vitreous if we think about a globe rupture, but that is not enough. Note that the depth of the anterior chamber is reduced. There is an increase in density as a result of hyphema (hemorrhage into the anterior chamber). Also note that the right lens is blurry, and slightly less dense than the left. This is called traumatic cataract. You might expect the lens to be denser, but this is usually not the case.
CT image shows a patient who has a traumatic injury to the left eye.
Explore the images for 5 finds, then continue reading.
Diagnostic findings:
- The anterior chamber is smaller compared to the contralateral chamber, indicating a rupture of the eyeball.
- The density in the anterior chamber is higher, indicating hyphema.
- The lens density is less, so this patient has a traumatic cataract.
- There is an area of high density in the vitreous, indicating hemorrhage.
- The eyeball is flattened along the posterior contour, which indicates a vitreous rupture.
Rupture of the eyeball can most often be diagnosed by the anterior chamber.
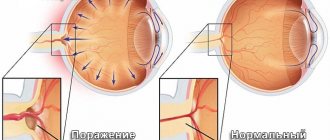
Retinal and choroidal detachment
Blood may be located in the following places:
- Anterior chamber: anterior hyphema
- Posterior chamber: posterior hyphema (too small to see on image)
- Vitreous: vitreous hemorrhage
- Choroidal detachment
- retinal disinsertion
Retinal detachment can be distinguished from choroidal detachment because the retinal epithelium ends in a serrated margin (indicated by arrows).
Obviously, retinal detachment will not go beyond this point.
Retinal detachment with hemorrhage is usually detected in adults with diabetes mellitus and hypertension. In young children this may be considered part of shaken baby syndrome. Choroidal detachment is usually associated with trauma.
The CT image (left) shows a choroidal detachment extending beyond the 10 and 2 o'clock positions (lens at 12:00) and apparently more anterior to the serratus margin. It looks like the detachment ends near the optic nerve, but if you look closely, the choroidal detachment actually crosses the optic nerve. This would be very unusual for a retinal detachment, but is sometimes seen with a choroidal detachment.
T1WI MRI image (right) shows retinal detachment. It ends near the optic nerve and with the serrated margin.
Another case of choroidal detachment.
Coloboma
Coloboma is a congenital developmental anomaly that occurs as a result of intrauterine disorders.
Microphthalmia often occurs and the eye protrudes downward. In 10% of cases it is accompanied by other central nervous system anomalies.
The image below shows a patient with bilateral colobomas.
Coloboma may be part of CHARGE :
- Coloboma _ _
- Heart anomalies _
- Choanal atresia (choanal A tresia)
- Slowdown growth and development
- Genital and Ear anomalies _
Coloboma may also be part of COACH :
- Hypoplasia of the cerebellar vermis ( Cerebellar vermis hypoplasia)
- Oligophrenia ( O ligophrenia)
- Congenital Ataxia _
- Coloboma _ _
- Liver fibrosis ( Hepatic fibrosis)
This image shows a patient with a small coloboma at the optic nerve entry site.
The image shows a patient with a coloboma, as well as an underdeveloped corpus callosum with a corresponding midline lipoma.
Intraconal pathology
Devic's syndrome
Devic's syndrome is also known as neuromyelitis optica.
Let's look at the images first and then discuss in more detail.
The image on the right shows a normal optic nerve. Note that the optic nerve has the same signal intensity as the white matter of the brain. On the opposite side there is high signal intensity in the optic nerve. Thus, this is an intraconal disease outside the eyeball, and we will differentiate a neoplastic process from a demyelinating disease.
FLAIR image with fat suppression (fat-sat). Note the abnormal signal intensity and the fact that the optic nerve is not enlarged, suggesting a nonneoplastic process.
Images of the cervical spinal cord show an extensive lesion.
Based on these images, a differential diagnosis should be made between Multiple Sclerosis (MS) and Devic's Syndrome (Neuromyelitis Optica).
Statistically, MS is much more common and would be the most likely diagnosis, but in this case it is Devic's syndrome.
Some believe that Devic's syndrome is a form of multiple sclerosis, but Devic's syndrome is different from MS:
- Devic's syndrome is more acute and transient.
- There is usually a combination of one-sided blindness and paralysis due to a long segment of transverse myelitis (MS typically has one or two segments).
- Devik is usually monophasic.
- There are usually no lesions in the brain.
Multiple sclerosis
The images show pictures of a patient who has optic neuritis.
There is an increased level of MR signal in the optic nerve, and there are several MS lesions in the brain. These lesions are distributed in time and space and are specific to MS. 50% of patients with optic neuritis are eventually diagnosed with MS. The remaining 50% have isolated optic neuritis (see differential diagnosis above).
80% of patients with multiple sclerosis develop optic neuritis at some point in time.
Meningioma
The images show a patient with extraocular intraconal disease.
Look at the images, describe them, and think about the differential diagnosis (ignoring for a moment the fact that the name for this item is meningioma).
The optic nerves are not changed, but there is a space-occupying formation, similar to a thickening of the optic nerve sheath on the left.
So it is likely a neoplasm, and meningioma is by far the most common tumor of the optic nerve sheath.
Meningiomas in the early stages of the disease manifest themselves as visual disturbances as a result of ischemic neuropathy due to venous obstruction. Clinically, this manifests itself as a “pallid optic disc.”
Abnormal enhancement of the optic nerve sheath
Symptom of tram rails in pathology of the optic nerve:
- Nerve sheath meningioma
- Leukemia
- Lymphoma
- Dissemination (metastasis) into the subarachnoid space
- Sarcoidosis
- Pseudotumor
Nerve sheath meningioma results from subdural growth leading to progressive vision loss, papilledema, and optic nerve atrophy. There is a strong association with neurofibromatosis type II. Pale optic disc due to decreased venous outflow. Calcifications are observed in 20-50%.
Dissemination (metastasis) into the subarachnoid space is another cause of increased nerve sheath signal due to the fact that the optic nerve sheath interacts with the subarachnoid space in the cranial cavity).
Optic nerve glioma
Let's take a look at the image first.
CT (left) and MRI T1WI (right)
On which side is the pathology, and what is the most likely diagnosis?
There is hypoplasia of the wing of the sphenoid bone on the right, and on the left at the level of the chiasm the optic nerve is enlarged (displayed on MRI). As a result, the diagnosis was neurofibromatosis type I with hypoplasia of the sphenoid wing and glioma of the optic tract.
The term optic nerve glioma is incorrect. In fact, the tumor can be anywhere along the optic tract from the occipital region to the chiasm and optic nerve. The term glioma is also quite nonspecific. These are juvenile pilocytic astrocytomas , according to WHO type I (I), which are the most favorable form of astrocytoma . They make up 4% of all orbital tumors. More than 50% of patients who have optic nerve gliomas also have NFI, but only 10% of patients with NFI have optic nerve glioma.
They are less often cystic in NF than in non-NF.
The average age at diagnosis is 4-5 years and only 20% of these patients have visual signs because early stage gliomas do not affect the optic nerve and because young children do not complain of vision problems.
The picture shows another case with a more typical example of optic nerve glioma, also in patient NFI
The picture shows another case with a more typical example of an optic nerve glioma in a patient with NFI.
A diagnosis of NFI is made if two or more of the following are present:
- Six or more café au lait spots
- Two or more neurofibromas of any type or 1 plexiform neurofibroma
- Many freckles in the armpit or groin area
- Skeletal dysplasia
- Optic nerve glioma
- Two or more iris hamartomas (Lisch nodules)
- Immediate relatives (first degree relatives) with NFI
LEFT: Several iris hamartomas (Lisch nodules)
- Right: Underarm freckles (small brown spots) and café au lait spots
↑ The role of deformation factors in the etiopathogenesis of surgical complications
So, an analysis of the literature and the results of our experimental and clinical studies have shown that one of the main manifestations of acute hypotony of the eye is significant disruption of the natural topographic relationships between its individual tissues and structures.
Noteworthy is the wide variety of external and internal deformation factors affecting the eye, under the influence of which one or another reaction of the contents of the eye to its opening and decompression is formed.
The complex nature of the interaction and mutual influence of individual deforming factors on each other requires their certain systematization in the process of study. When analyzing this problem, we proceeded from the fact that the basis of any deformation of the fibrous capsule and intraocular tissues is traumatic depressurization of the eyeball cavity and an imbalance in the physiological balance between intraocular (IOD) and extraocular (EOD) pressure.
Since each of these types of pressures is determined by many components and the violation of individual components of the IOD-EDI system cannot be considered in isolation from others, we have combined all the main types of pressures that determine the anatomical state of the eye in the form of a diagram (see Diagram 9).
Scheme 9. Main types of pressures, the interaction of which determines the anatomical state of the eye tissues during abdominal operations
When drawing up the scheme, we took into account the ambiguity of the impact of changes in IOD and EDI on the anatomical state of the eye, which, in our opinion, occurs during traumatic depressurization of the eyeball. The peculiarity is as follows.
Any factors that increase extraocular pressure (pressure from the eyelids, eye immobilization devices, extraocular muscles, etc.) can lead to disruption of the anatomical state of the eye (tissue deformation) only if it exceeds the intraocular pressure. Changes in intraocular pressure can cause deformation of individual intraocular tissues, regardless of whether the overall balance between IOD and EDI is disrupted or not.
Thus, when the pressure in the chambers of the eye decreases, for example, to 10 hPa, the total intraocular pressure will continue to significantly exceed the extraocular pressure, however, as our studies have shown, the choroid will thicken due to hyperemia, the additional volume of blood will shift the vitreous body anteriorly, transudation fluid from overcrowded vessels can cause CCD, thickening of the lens, “shrinkage” of the fibrous capsule, etc. will also occur.
Based on the above, we have identified two independent forms of eye deformation - extraocular and intraocular.
Conventionally, we can assume that intraocular tissue deformation occurs as a result of a violation of hydrostatics in the eye cavity (imbalance between hydrostatic, osmotic and colloidosmotic pressures in tissues and intertissue spaces and, as a consequence, changes in IOD, and extraocular - as a consequence of the predominance of external pressure (ED) .
Based on our own rheographic and echographic studies [65-68,91-95], as well as literature data, we identify five main types of intraocular and extraocular deformation. Separately, this chapter also discusses changes in the anatomical state of eye tissues according to the type of volumetric and linear deformation. The general classification of various types of eyeball deformities is presented in the diagram.
Conal pathology
Endocrine ophthalmopathy
Look at the images, describe them and think about the differential diagnosis, ignoring the title of this item.
Diagnosis of endocrine ophthalmopathy, differential diagnosis with orbital pseudotumor. We will soon discuss how to differentiate between these two diseases.
In the past, the term Graves' ophthalmopathy (Graves' disease) was used. This, however, assumes that the patient has hyperthyroidism. We now know that patients with Graves' disease can have normal thyroid function (euthyroidism) or even hypothyroidism and develop endocrine ophthalmopathy, which is why we currently use the term endocrine ophthalmopathy.
The great danger with endocrine ophthalmopathy is compression of the optic nerve, either due to direct collapse by muscles or damage due to vascular ischemia. The key point here is to inspect the orbital apex. If you do not see fat around the orbital apex, there is a high chance of compression. These patients require decompression and endoscopic surgical removal of the medial orbital wall is performed.
Pseudotumor
Take a look at the images. This is a case of pseudotumor. Pseudotumor is an idiopathic inflammation of the orbit that can affect every part of the orbit: muscle, tendon, fat, optic nerve, optic nerve sheath, lacrimal gland, etc.
The main difference between pseudotumor and endocrine ophthalmopathy is the fact that pseudotumor involves not only the muscles, but also the tendons. These patients feel pain when they move their eyes due to irritation of the tendons.
The image on the left shows an enlarged muscle, with the arrow indicating the tendon in a patient with endocrine ophthalmopathy. On the right is an image of a patient with a pseudotumor. Please note that the swelling also affects the tendon.
Main causes of visual impairment
The causes of decreased visual acuity are divided into two groups: congenital and acquired. Patients suffering from ophthalmological diseases are forced to correct their vision with glasses or contact lenses. Eye pathologies affect a person’s quality of life and limit his professional activities. Vision problems occur for the following reasons:
- Long-term eye strain;
- Atrophy of the lens muscles;
- Moisture deficiency in the mucous membranes;
- Impaired blood circulation in tissues;
- Age-related changes;
- Lack of sleep;
- Concomitant diseases of the body;
- Head or eye injuries.
Decreased visual acuity is provoked by regular and unlimited use of gadgets. Therefore, you need to take a break and give your eyes a rest. The first symptoms of decreased vision: headaches, blurred vision, discomfort in the eyes. If one of these signs occurs, you should consult an ophthalmologist.
Regular examination by an ophthalmologist is a guarantee of maintaining visual acuity. The sooner a specialist detects the disease, the greater the likelihood of its complete cure.
Extraconal pathology
Periorbital abscesses
A native (non-contrast) CT image shows a patient with an obvious periosteal or periorbital abscess. Do not hesitate and wait for peripheral enhancement during contrast before making a conclusion about an abscess! In every other place you conduct contrast and wait for a beautiful picture with peripheral enhancement like a rim in order to call the formation an abscess, to say the least, a phlegmon. Treatment: treatment of sinusitis.
In children, any extension beyond the sinuses should be called an abscess.
In children, the periorbital space is more cellular, and the pathological process spreads easily. So be confident and persistent in calling small changes an abscess.
Periorbital abscess can lead to venous thrombosis in the superior and inferior ophthalmic veins.
With fungal sinusitis (aspergillosis), you can even get cavernous sinus thrombosis and cavernous-carotid fistula.
Orbital and periorbital cellulite
The image shows a patient who is admitted as an emergency with red eye and exophthalmos.
Knowing the difference between orbital and periorbital cellulite is important and is based on an anatomical structure called the orbital septum (orbital septum, or septum orbitale).
If a patient comes in with red eye and the inflammation involves the orbital septum and extends outward from it, a diagnosis of periorbital cellulitis is made and the patient is treated with oral antibiotics on an outpatient basis.
In the case in the image above, structures behind the septum are also involved. This patient has orbital cellulitis and requires inpatient treatment with intravenous antibiotics.
Pathology of the wing of the sphenoid bone
CT image shows a patient with exophthalmos due to a lesion in the sphenoid wing.
There are four pathologies of the sphenoid wing that can cause proptosis:
- dysplasia
- fibrous dysplasia
- Paget's disease
- meningioma with hyperostosis of the sphenoid wing
Images show meningioma of the sphenoid wing
Lesions of the lacrimal gland
Diseases of the lacrimal gland can be divided into the following types:
- Granulomatous\lymphoid Sarcoidosis, pseudotumor, lymphoma, Sjögren's syndrome, Mikulicz's disease, tuberculosis
- Pleomorphic adenoma, glandular cystic carcinoma
Inflammatory conditions are by far the most common lesions of the lacrimal gland (Sjögren's syndrome, tuberculosis, fungus, pseudotumor). These conditions do not cause tumor damage.
- inflammation 64% pseudotumor, dicryoadenitis
The most common tumor-bearing condition is lymphoma, followed by pleomorphic adenoma. Epithelial tumors, including glandular cystic tumors, are rare.
Vascular malformations
Vascular anomalies can be located intraconally, extraconally, or in all spaces, and this is the reason why they are not discussed in the categories above.
Before we show you some cases, we must discuss the Mulliken and Glowacki classification system for vascular anomalies in the neck and head region, which is widely accepted today.
classification of orbital vascular anomalies according to Mulliken and Glowacki
- Capillary hemangiomas
- Arteriovenous malformations
- Venous-lymphatic malformations
- Dilation of the orbital veins
- AVF, dural AVM
Capillary hemangioma
The first anomaly in the Mulliken and Glowacki system is capillary hemangioma.
Capillary hemangiomas have the following characteristics:
- a neoplasm with a growth phase at 6-12 months of age and an involutional phase at 5-7 years of age.
- They are mainly located in the skin, but can also be seen in the extraconal space of the orbit.
- It usually resolves spontaneously, but is sometimes treated with steroids, laser, or interferons.
- May be part of PHACE syndrome: posterior fossa malformations, hemangiomas, arterial anomalies, cardiac defects and ocular disorders such as coloboma, glaucoma.
Venous malformations
The second anomaly in the Mulliken and Glowacki system is Arteriovenous Malformations.
The image shows a venous malformation. An intraconal lesion is determined in combination with phlebolitis. Most of them are single-chamber, but in this case it is multi-chamber.
Venous malformations have the following characteristics:
- Most common intracanal lesion in adults
- More common in women, average age 45 years, with slow progressive increase
- Also known as cavernous malformations, but this term is no longer used
- This lesion is characterized by phlebolith and may be part of Maffucci syndrome and Bean syndrome
- You can observe them over time, as a rule, they will grow over time and may require surgery
Lymphatic defects
Next on the list are lymphatic or venolymphatic defects.
These are small cystic areas that often bleed after minor trauma. They may have high signal intensity on T1WI due to high protein content or hemorrhage. They usually do not enhance unless there is a venous component that can be contrasted. This lesion belongs to the “family” of cystic hygroma.
Other characteristics:
- Adolescence (60% up to 16 years old)
- May bleed suddenly resulting in fluid levels
- May be extrasacral or multicompartmental
- Associated with intracranial malformations, as in Turner syndrome or fetal alcohol syndrome
- Lack of contrast enhancement in purely lymphatic lesions
Dilation of the orbital veins
The images show a patient with dilated orbital veins who noticed that the left eye moves when straining. The top image is during relaxation, and the bottom image is with the Valsalva maneuver while sneezing. During Valsalva, the vein is greatly dilated (red arrow). Note that during Valsalva and on the contralateral side, the superior ophthalmic vein is dilated (blue arrow).