The cornea is made up of layers.
The epithelium covers a dense stroma.
The inside is lined with endothelium.
The cells of the inner layer are responsible for the outflow of eye fluid. The endothelium is not renewed. When damaged, moisture enters the following layers, creating swelling. Bubbles appear in the epithelium. The cornea becomes cloudy, becomes white, matte. The pathological condition is called endothelial-epithelial dystrophy (EDD), Fuchs' dystrophy, pseudophakic bullous keratopathy.
Causes
Austrian physician Ernst Fuchs first described EED in the early 20th century. He considered the cause of destruction of the endothelium to be a malnutrition, blood supply, and hormonal imbalance.
Endothelial degeneration occurs as a result of:
- hereditary genetic disorder;
- cataract extraction operations;
- injuries;
- chronic keratitis without treatment.
Primary dystrophy is caused by heredity. Secondary damage occurs due to disease and mechanical damage. But a prerequisite for the development of edema after operations and injuries is a genetic predisposition.
Chronic corneal erosion in dogs
Natalya Vladimirovna Vologzhanina – veterinary ophthalmologist
Chronic corneal erosion in dogs is a pathological condition in which there is a constant recurrence of impaired corneal epithelization.
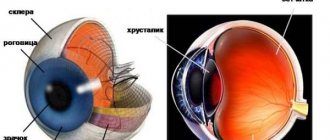
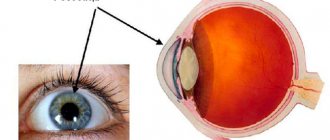
The cornea is one of the most sensitive organs in our body. It is part of the uppermost membrane of the eyeball (fibrous membrane), is transparent and serves both to refract light rays and to protect the internal structures of the eye due to its density. In its structure, it resembles a layer pie, which is covered on both sides with a dense crust, and inside there are thinner layers of cakes (Fig. 1).
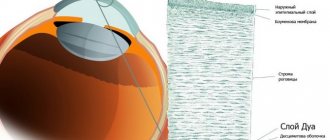
The surface of the pie on the inside is the internal epithelium, which is attached to Descemet's membrane; it is a layer of polygonal cells tightly adjacent to each other. The middle part is the corneal stroma, which consists of dense fibrous connective tissue. It contains a large number of collagen fibrils, with cells included between them - keratinocytes. The stroma is hydrophilic, therefore, if the external or internal epithelium is damaged, collagen fibers absorb moisture and the cornea may lose its transparency. The outermost layer is the superficial stratified non-keratinizing epithelium. It consists of 5-6 layers of cells and lies on the basement membrane, attached to it by hemidesmosomes. In turn, the basement membrane ensures a tight connection between the epithelium and the underlying stroma, which shows a clear and thoughtful organization of the tissues of living organisms, which nature so unusually and correctly created.
Fig. 1. Micropicture of the normal cornea: 1 – superficial epithelium; 2 – corneal stroma; 3 – Descemet’s membrane; 4 – internal epithelium (endothelium).
But even ideal biological creatures, such as the tissue of the cornea of the eye, are subject to various pathological changes in architectonics, which is typical for all living organisms in our difficult environment. A condition in which there is a violation of the integrity of the surface epithelium is called corneal erosion. It can occur in different situations, be it a superficial injury, toxic exposure or viral infection, but is always accompanied by severe pain. An animal will never tell you that it is in pain, but by certain clinical signs you can recognize that it is in discomfort.
With corneal erosion, the dog squints the sore eye, scratches it with its paw or on various objects, the owner, and lacrimation and photophobia are also observed. Sometimes, you may notice a change in the color of the cornea; it becomes cloudy, bluish-grayish, or may turn red due to a vascular response to damage. Also, redness of the conjunctiva of the eye is observed and there may be mucous or purulent discharge from the conjunctival sac.
Rice. 2. Micropicture of the cornea with the formation of pathological epithelium: 1 – pathological epithelium; 2 – corneal stroma.
In dogs of the German Boxer, American Staffordshire Terrier, Pit Bull Terrier, Staff Bull, French Bulldog, and Labrador breeds, a pathology such as chronic corneal erosion is observed. As a rule, it occurs in animals over 5 years of age and is accompanied by the above clinical signs of ocular discomfort. It is associated both with anatomical lagophthalmos (non-blinking) in these dog breeds and with impaired adhesion of the surface epithelium to the basement membrane. Presumably, this pathology is associated with the inferiority of hemidesmosomes, epithelial cells and damage to the basement membrane, characterized by the growth of pathological epithelium on the cornea (Fig. 2), which is not able to stay on its surface and, with the slightest external influence, sloughs off, forming a new erosion.
Upon examination, the erosion may not be very large in size, but this illusion is created by the fact that the pathological epithelium can occupy a fairly large area, creating the appearance of an epithelialized cornea and not allowing normal regeneration to occur (Fig. 3). This disease is under study by various ophthalmologists. In some literary sources, this pathology is even called “Boxer Ulcer”, since it is most common in these dog breeds.
Rice. 3. Clinical condition of the eye of a 7-year-old German boxer with chronic corneal erosion: 1 – visible edge of erosion; 2 – true edge of erosion.
When treating animals with similar conditions, problems often arise due to the peculiarity of the disease - it constantly recurs. The dog experiences a positive effect during treatment and everything seems to be fine, but after a while, repeated erosion may occur in the same place or in another, including on the bilateral eye, where there was not even a suspicion of pathology.
To treat dogs with chronic corneal erosion, combined therapeutic and surgical techniques are used, which consist of removing the pathological epithelium, correcting the surface of the cornea using special equipment and prescribing drugs that prevent the development of infection and stimulate corneal regeneration. In addition, superficial keratectomy with tarsorrhaphy for a period of time is an effective treatment method. The operation consists of microsurgical removal of the superficial layers of the cornea in the area of the pathological area, followed by closing the eye to the third eyelid for better tissue healing, as under a bio-bandage. In most cases, after surgery, if the animal is properly cared for and the veterinarian’s recommendations are followed, no relapse is observed (Fig. 4a, 4b). The procedure is carried out under general anesthesia and, therefore, preliminary examinations of the animal are required for systemic pathologies and an assessment of the risks of anesthesia.
| Rice. 4a. Clinical picture of chronic corneal erosion in a Labrador dog, 10 years old. Cloudiness of the cornea and loose edges of erosion are visible | Rice. 4b. Condition of the eye on the 14th day after superficial keratectomy. Complete epithelization of the cornea, at the site of the former erosion there is slight turbidity that does not interfere with vision. |
Chronic corneal erosion can occur in other dog breeds and may be associated with different problems. Other causes of chronic recurrent corneal erosion are limbal insufficiency syndrome, failure of the meibomian glands, keratoconjunctivitis sicca, diabetes and other systemic diseases that lead to degenerative processes in organs and tissues.
The diagnosis of chronic recurrent corneal erosion is not a death sentence; in modern times, most pathologies can be maintained, if not cured. But it should be taken very seriously, because such conditions can lead to irreversible changes in the cornea of the eye, impairment of the animal’s vision and its quality of life.
If you notice that your dog’s eyes are watery and red, he is squinting, scratching and experiencing discomfort, you should immediately contact a veterinary ophthalmologist, where they can provide qualified assistance and cope with any insidious disease.
Return to list
Symptoms
The disease occurs without symptoms. Development from initial cellular changes to overt clinical manifestations can take 20 years.
Signs that appear during the course of the disease:
- vision in the morning is worse than in the evening;
- foreign body sensation;
- pain;
- sensitivity to light;
- hyperemia;
- lacrimation;
- swelling, clouding of the cornea;
- bull formation
Bubbles on the surface of the epithelium burst, causing severe pain.
Diagnostics
Upon external examination, clouding of the cornea is noticeable, which is sometimes accompanied by dilation of the conjunctival vessels. The diagnosis is confirmed using diagnostic procedures:
- Biomicroscopy. Signs of EED: lack of endothelial cells, swelling, bullous lesions of the epithelial layer.
- Pachymetry. By measuring the thickness of the cornea, the degree of swelling is assessed.
- Confocal microscopy. The method allows us to examine the structure of the endothelium, determine the density and size of its cells, and trace the dynamics of the destructive process. The guttas are also visible using the method. Specific drop-shaped formations are distinguished among endothelial cells by small dark cells with a light center. As the endothelial cells decrease, the gutta merge into large areas.
- Visometry in the morning and evening helps to indirectly determine the swelling inherent in EED and the degree of vision loss.
Signs of epithelial corneal dystrophy
In the early stages of the pathological process, patients note increased intolerance to light and glare. Over time, vision deteriorates in the morning, and is somewhat restored in the evening. This happens because during sleep, moisture does not evaporate from the surface of the cornea, but accumulates in it. When the eyelids are open during the day, this mechanism of fluid removal is also activated, which leads to a shift in the balance to the normal state.
As endothelial cells die, vision deteriorates. If a patient's visual acuity decreases to such an extent that he loses the ability to care for himself, indications arise for a corneal transplant.
Treatment
Conservative therapy program:
- local administration of hypertonic saline solutions;
- the use of drops to improve trophism;
- applying eye ointments to promote healing;
- pain relief with analgesics in the form of drops or tablets;
- cross-linking procedure.
The saline solution traps and removes excess fluid from the tissues. Vision is corrected using optics - glasses, therapeutic contact lenses.
Bullous formations are eliminated using corneal cross-linking:
- The epithelium is removed from the cornea;
- apply riboflavin;
- irradiated with a special ultraviolet spectrum.
As a result, a new frame is formed on the cornea, preventing its deformation.
Surgical treatment - keratoplasty. Indications:
- severe degree of vision loss;
- thinning of the cornea;
- low endothelial density.
Types of keratoplasty:
- end-to-end - complete corneal transplantation;
- layer-by-layer DSEK - transplantation of Descemet's membrane with endothelium.
The damaged cornea is replaced with donor tissue and bioimplants. Layer keratoplasty is performed minimally invasively. The graft is inserted through a small incision, unfolded and fixed to the stroma with a stream of air.
Types of corneal dystrophy
The disease is classified based on which layers of the cornea are affected.
| Affected layer | Types of dystrophies: | Peculiarities |
| Outer epithelium |
| The primary form, which an experienced ophthalmologist can notice even in a child. Develops when there is a small number of epithelial cells or their dysfunction. It manifests itself in a large number of cysts, which over time transform into opacities. |
| Bowman's shell |
| They belong to the primary form and can be diagnosed in pediatric patients. Despite remissions, they continue to progress. |
| Horny stroma |
| They are rare, congenital forms in which there is a corresponding family history. They develop due to failures in the synthesis of collagen fibers. During ultramicroscopic diagnostics, the doctor determines the abnormal thinness of collagen fibers and their alternation in a bundle with loose layers that do not have a specific organization. |
| Endothelium |
| It is characterized by cell death, which can cause excess fluid in the stroma. It most often affects women and appears at the age of thirty. |