Even a person who has encountered one or the other ailment cannot always understand the difference between myopia and astigmatism. Each disease has its own symptoms that are unique to it.
There are more and more people experiencing visual impairments every day. In everyday life, we do not always notice in time that we have begun to see worse. And only when the font on the computer monitor has to be enlarged more and more, and the sheet of text is brought closer to the eyes, do we think about the need to have our eyesight checked. It is these signs that become the first symptoms of myopia and other visual impairments.
Astigmatism exhibits similar symptoms, so both of these diseases are easy to confuse. In addition to similar symptoms, both diseases have a similar nature of occurrence. In both cases, the problem arises due to deformation of the lens. Very often both
In this article
- Astigmatism
- Myopic astigmatism
- Causes of astigmatism
- Myopia
- Causes of myopia
- Astigmatism and myopia: differences
- Treatment of astigmatism and myopia
- Prevention of astigmatism and myopia
diseases are combined. Let us consider in detail each disorder separately and how myopia differs from astigmatism.
Astigmatism
To roughly imagine how a person with astigmatism sees, you need to look at yourself with a teaspoon. This is a disease that is characterized by a defect in the refractive power of the eye, that is, refractive error. The reason is a distortion of the shape of the lens or cornea of the eye.
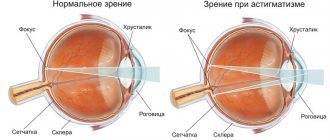
In healthy organs of vision, the lens and cornea have an even hemispherical shape. With astigmatism, their surface is distorted. As a result, light rays passing through the eyes are scattered incorrectly. Since the rays are not focused at one specific point, part of the image goes to the retina, and part is formed in front of it. A person with astigmatism ends up seeing a distorted picture. Objects at any distance appear slightly blurry. Outlines can stretch both horizontally and vertically. A distorted image is the main symptom of the disease.
Very often, astigmatism is combined with other visual impairments, such as myopia and farsightedness. Depending on this, astigmatism is distinguished:
- Simple. Myopia or farsightedness appears only on one meridian (conventional horizontal and vertical lines perpendicular to each other) of the eyes.
- Difficult. Deviations are characteristic of two meridians.
- Mixed. Myopia appears on one meridian, and farsightedness on the second.
If astigmatism is combined with myopia, it is called myopic. When farsightedness occurs along with astigmatism, it is hypermetropic astigmatism.
Myopia, farsightedness and astigmatism - how to cure and how to prevent?
The eyes are the window to the world. How far can you see through it? How clear is your vision?
Today we are talking about the most common problems with an ophthalmologist from Clinic Expert Tula LLC, a certified doctor in the Russian Federation, Tatyana Sergeevna Zhuravleva.
Tatyana Sergeevna, tell me, why and how often do you need to check your vision?
The frequency of vision tests is regulated by the Ministry of Health. There are several age periods, since in each of them we can identify certain types of pathology. These are 1, 12 months, 3 years, 6, 7, 10, 11, 15, 16 and 17 years. However, the strain on the eyes of modern children has increased. Therefore, we ask parents to bring their children to see an ophthalmologist annually to have their visual acuity checked.
If we talk about diseases that can be detected at one age or another, then, for example, at one month of age we can already identify congenital eye pathologies: cataracts, glaucoma, dacryocystitis, nystagmus, strabismus. At 12 months, one can judge the eye’s ability to refract light (refraction), i.e.
about the presence of congenital myopia (myopia) or farsightedness (hypermetropia), astigmatism. At the age of 3, it is already possible to check visual acuity. It is also advisable to do this at 5 years of age. Why? First of all, due to the proliferation of various kinds of gadgets: phones, tablets, etc.
Another reason: at this age, preparatory classes for school, clubs, etc. often begin, which also puts additional strain on vision.
It is important to warn parents that the child is born with slight farsightedness and this is the norm. Such farsightedness gradually disappears as the baby grows. However, in some children at the age of 7, when they go to school, its remains remain and, importantly, remain undetected.
This happens because only visual acuity is checked, and additional studies - in particular refractometry - are not carried out. At school, such a child may not see clearly at close range, as a result of which his writing is not entirely straight. In addition, he is not always able to say that he sees poorly. It is clear that this may ultimately affect his academic performance.
Therefore, such children are temporarily prescribed spectacle correction for near work until farsightedness goes away.
In adults under 60 years of age, the frequency of vision assessment is once every two years if there are no problems, and once a year or more often if there are any problems.
What are myopia and farsightedness?
Normally, the maximum clarity (focus) of what we see is formed precisely on the retina of the eye. Nearsightedness (myopia) is one of the most common disorders when this focus is shifted and is in front of the retina. As a result, vision becomes blurry. To put it another way: with myopia, a person sees well near and poorly at distance.
Unlike myopia, farsightedness (in other words, hyperopia) is a disorder when the focus of the image is not in front of the retina, but behind it. In other words, a person sees well at a distance, but poorly at close range.
Are there any risk factors for developing myopia?
Yes, definitely. Among them:
- genetic predisposition. If one of the parents has myopia, then the child has a 50% chance of developing it. When both people have myopia, the risk of developing it increases to 70%. Moreover, the child may have a higher degree of myopia than the parent, and moreover, it may manifest itself at an earlier age;
- - injuries to the cervical spine, including during obstetrics;
- — early start of children’s education;
- - excessive visual strain - in particular due to the use of phones, tablets, computers;
- - increased training loads.
- Tatyana Sergeevna, how is myopia and farsightedness treated?
If we talk about non-surgical restoration of vision, then functional treatment is prescribed using special optical devices, irradiation of the ciliary muscle with a low-intensity laser, photo and magnetic therapy, training to relieve accommodation spasms, massage of the ciliary muscle by changing positive and negative muscles. Massage of the cervical-collar area, magnetophoresis with medicinal substances are carried out, vascular drugs and vitamins are used.
Gymnastics for the eyes is mandatory. It includes rotational movements clockwise and counterclockwise (5-6 times), looking up and down, left and right, and some others.
There are somewhat fewer methods for treating farsightedness. This is mainly the wearing of glasses, increased visual load on the low-vision eye in the form of working or playing with small objects with occlusion of the better-seeing eye, as well as hardware treatment methods.
In cases where conservative (non-surgical) treatment does not help, surgical correction methods are used.
But will surgery cure farsightedness and nearsightedness?
With farsightedness, most people simply do not go for it, since they may already have normal distance vision, but for near they use glasses. It is also possible to restore vision surgically for farsightedness, and if a person is thinking about this, then he needs to get an individual consultation with an ophthalmic surgeon for laser vision correction.
Regarding myopia. In children with progressive myopia, scleral strengthening operations are performed. Modern surgical interventions in the form of laser vision correction in adults are successful and, depending on the degree of myopia, they can help achieve 100% vision.
How to live with age-related farsightedness?
This type of disorder is called “presbyopia.” This pathology is based on age-related changes in the lens. In people with normal vision, it usually develops at 40-45 years of age. If a person previously had myopia, then presbyopia will develop later, and if farsightedness - earlier than this age.
Correction is carried out using glasses. As farsightedness increases, they are changed.
Are surgeries performed for age-related farsightedness?
Operations have been developed, but not all have worked well. The most successful intervention is considered to be performed when the lens of the eye already has signs of cataract sufficient for surgery. In this case, it is removed and replaced with a modern artificial lens. It refracts light rays much better and leads to a significant improvement in vision.
Tell us about the prevention of myopia and farsightedness.
For myopia, preventive measures include general strengthening of the body, including hardening and a balanced diet. Any sport that does not involve prolonged tilting of the head down, with the risk of bruising, is useful. Swimming, tennis, volleyball, basketball, running are good.
It is necessary to provide good lighting at the table, including a table lamp of 60-100 W (the light should fall from the left if the person is right-handed). It is necessary to maintain the correct posture at the table.
The distance of the eyes from the book and notebook should be at least 40 cm. You should not read while lying down, or in transport.
Breaks in classes are required: with normal vision - every 40 minutes, with mild myopia - every 30 minutes, with moderate and high degree - every 10-15 minutes.
A separate issue is watching TV. Children under 3 years old should not watch it. From 3 to 7 years, the total viewing time should not exceed 30-40 minutes per day.
Gymnastics for the eyes is also useful. We talked about it earlier.
Myopic astigmatism
More often than others, a combination of myopia and astigmatism occurs. As a rule, the disease is congenital.
The causes of acquired myopic astigmatism are:
- mechanical eye injuries;
- consequences of unsuccessful surgery;
- high load on the visual organs;
- consequences of severe eye inflammation.
Symptoms of myopic astigmatism:
- unclear outline of objects;
- poor vision at a distance;
- rapid eye fatigue;
- redness, photophobia, lacrimation;
- headache.
The disease is corrected with glasses and contact lenses. Spherical lenses are used to correct myopia, and cylindrical lenses are used to correct astigmatism. For a patient with myopic astigmatism, a special accessory is made that combines both of these parameters.
In cases of complex myopic astigmatism, surgery may be required. There are two types of operations performed: keratotomy and laser vision correction.
Classification and causes of myopia development
Ophthalmologists distinguish the following types of myopia:
- Congenital
- Hereditary
- Acquired (in preschool or school age)
- Mixed
The prognosis for children with congenital myopia depends on the complex of rehabilitation measures.
Acquired myopia can develop over many years, usually debuting at school age
This is due to the standardization of training, low attention to physiological characteristics and requirements, and sharply increased eye strain
You should pay attention to maintaining a sleep and rest schedule. Long-term strain on the eyes is divided into several parts, alternated with relaxing physical exercises for the head and neck. The rarest myopia is hereditary
Parents with this pathology have a very high chance of having a myopic child. During the initial examination of a newborn, a competent pediatrician will also pay attention to the parents’ medical history. This will allow you to timely assess the risks and limit the factors that contribute to visual impairment in a child at an older age.
The rarest myopia is hereditary. Parents with this pathology have a very high chance of having a myopic child.
During the initial examination of a newborn, a competent pediatrician will also pay attention to the parents’ medical history. This will allow you to timely assess the risks and limit the factors that contribute to visual impairment in a child at an older age.
Classification of myopia by degree:
- weak – up to 3.0 diopters
- average – from 3.25 to 6.0 diopters
- high – above 6.0 diopters
All of them are diagnosed at an outpatient appointment with an ophthalmologist. Only he can correctly assess the stage of myopia development and give correct recommendations. In adults and children, the primary stage is visometry - checking visual acuity using special tables with letters or pictures. Next, to clarify the diagnosis, an ophthalmoscopy is performed - an examination of the fundus of the eye. It allows you to determine the degree of degeneration of eye structures and the transparency of the optical media.
Low myopia
Appears more often before the age of 18 years. It is manifested by rare squinting, rapid fatigue during exercise, photophobia and a desire to blink more often. This stage may not progress for a long time, bringing only occasional discomfort. The structures of the eye are not yet subject to significant changes, the vessels are still full of blood, the nutrition of the nerve fibers is not impaired. Low myopia is diagnosed using the Sivtsev-Golovin table, which consists of lines with letters of different sizes. It is also advisable to perform an ophthalmoscopy in order to identify possible astigmatism (curvature of the lens or cornea) in time. If myopia is uncomplicated, then the doctor recommends a set of physical exercises for the eyes and vitamin complexes to improve eye nutrition.
Glasses are prescribed for distance use only; there is no need to wear them all the time. If astigmatism is present, glasses lenses are selected taking into account the complication.
Moderate myopia
It starts with a defect of 3.25 diopters. Here the patient complains that he does not see images clearly at a distance of more than 2-3 meters. As the stage of the disease progresses, this distance is reduced to half a meter. The contours of objects become unclear, the picture becomes blurry. Ophthalmoscopy reveals stretched, thinned vessels and impaired nutrition of the retina. Correction must be carried out using glasses or contacts. For moderate myopia, surgical or laser treatment may be recommended, especially if there are concomitant eye pathologies.
Causes of astigmatism
According to the nature of its occurrence, astigmatism can be congenital or acquired. In the first case, the disorder can be inherited or occur during the formation of the fetus. If one of the parents had similar vision problems, then the disease at the genetic level can be passed on to the baby. The probability of transmitting a hereditary disease in this case is 50% to 50%. If both parents had ophthalmological disorders, the risk increases to 75%.
During pregnancy, the following factors can trigger the development of eye disease:
- alcohol consumption;
- smoking;
- use of antibiotics.
In addition, the disease can be caused by incorrect position of the muscles, eyelids and bones of the orbit. Due to such pathologies, uneven pressure is placed on the eyes, which leads to impairment.
The most common causes of acquired astigmatism are:
- injuries of the cornea and lens;
- inflammatory diseases (for example, keratitis, blepharitis, etc.);
- consequences of eye surgery, when the patient did not follow postoperative recommendations or the sutures were applied incorrectly;
- degeneration of the cornea, which can result from a disease such as keratoconus: the membrane becomes thinner and takes on a cone-shaped shape.
The main symptom of astigmatism is the distortion of objects. A person sees objects blurred, unclear, or they may appear double.
In addition, visual impairment may be accompanied by:
- headaches;
- painful reaction of the eyes to light;
- poor vision in low light;
- rapid and severe eye fatigue.
A person with astigmatism sees objects blurry at any distance.
What is astigmatism and what are its symptoms
Astigmatism is a condition that occurs when a defect in the cornea or lens prevents images from focusing correctly. When light rays enter an eye with astigmatism, they are focused on multiple points on the retina at the same time, causing blurred vision. Often this condition is caused by abnormal curvature in different parts of the cornea.
Astigmatism can develop at any age and among its main symptoms we find:
- Blurred vision at long and short distances.
- Visual fatigue.
- Double vision.
- Red eyes.
- Difficulty driving at night.
- Squint for focusing
- Tension headache
Myopia
When objects at a distance begin to “float” and you have to squint your eyes to see them, this is a reason to think about visual impairment. In most cases, blurry objects at a distance and clear contours close up indicate that a person is nearsighted. Myopia, as ophthalmologists call the disease, occurs in many people. It has become especially widespread with the advent of various gadgets in a person’s daily life. Fatigue and increased eye strain are the main causes of visual impairment in adults.
As with astigmatism, with myopia, pathology is caused by incorrect refraction of optical power, that is, refractive error. In healthy organs of vision, light rays enter the eyeball, are refracted in the cornea and lens, and are then formed into a clear image on the retina.
Our organs of vision are designed in such a way that when viewing objects near and at a distance, the optical power of the eyes changes. This happens due to the ciliary muscle or, as it is also called, the ciliary muscle. When looking at nearby objects, muscle fibers contract and are tense. When viewed from a distance, the ciliary muscle, on the contrary, relaxes. Under its influence, the curvature of the lens changes. The ability of the organs of vision to change the focal length to ensure good vision at different distances is called accommodation.
Myopia is caused by a change in the shape of the eyeball under the influence of various factors. It becomes more elongated, ellipsoidal. Accordingly, the length of the eye axis increases. As a result, the image is formed not on the retina, but in front of it.
In life, this leads to poor vision at a distance, objects in the distance become blurry.
Symptoms of myopia
The main symptom of myopia can be considered good visibility of objects located close, and poor in the case of distant objects.
But this pathology also has other signs:
- People with this disease usually squint to better see things at a significant distance;
- The eyes get tired quickly even with short periods of exercise;
- People with this diagnosis often experience headaches.
This pathology can be detected in a child by the following signs:
- Frequent complaints of headache;
- The child brings objects close to his face to examine them;
- Frequent blinking;
Causes of myopia
Like astigmatism, myopia can be congenital or acquired. If a disorder is diagnosed in a baby soon after birth or in childhood, then its cause is a hereditary factor. During life, the disease often occurs due to poor visual hygiene. The development of myopia is caused by:
- fatigue of the visual organs;
- reading or working with small details in poor lighting;
- eye injuries;
- diabetes;
- poor nutrition, lack of vitamins and nutrients in the diet.
Myopia can be false. The cause of this disorder is increased visual stress, which leads to spasm of the ciliary muscle. If you do not give your eyes rest, for example, work without a break for a long time at the computer, the muscle stops relaxing. Depending on what object the vision is focused on, close or far, the muscle contracts or relaxes, changing the shape of the lens. With false myopia, the muscle stops relaxing. As a result, visual acuity decreases.
Only a specialist can determine true or false myopia during an examination. False myopia does not require drastic treatment measures. It can be eliminated with eye drops and exercises.
Features of myopia
Unlike astigmatism and farsightedness, nearsightedness focuses light in front of the retina.
This results in distant objects appearing blurry. As a rule, with myopia, there is an increase in the size of the eyeball. However, in some cases, this visual impairment can cause the refractive power to be too high.
Depending on the difference with normal vision, there are 3 degrees of myopia - weak, medium and high.
The last degree can reach impressive values - up to 30 diopters.
Astigmatism and myopia: differences
The common features make astigmatism and myopia similar. In both cases, the disorder occurs in the same areas of the visual organs. These diseases have similar treatments. Without delving into the problem, the diseases are easy to confuse, but the development of ophthalmology has made it possible to identify the differences between these two visual pathologies.
When diseases occur separately, they have different symptoms. If with myopia the patient sees well near and poorly at a distance, then with astigmatism objects are blurred at any distance. This is the main difference between myopia and astigmatism. Another characteristic sign of the disease is double vision or changes in the shape of things. A person with astigmatism has difficulty determining the distance to objects.
Different types of lenses are used to correct diseases. For myopia, wearing glasses or lenses with negative optical power is prescribed. Astigmatism requires the use of cylindrical lenses. You need to understand that optical aids do not eliminate the problem, they only help you see better.
In both cases, once the diagnosis is made, surgery, including laser correction, may be recommended. Astigmatism is eliminated by laser removal of the top layer of the cornea. Thus, its curvature changes. The differences between the diseases may not be obvious. An accurate diagnosis can only be made during an examination.
What are the differences between pathologies?
The same elements of the optical system of the eye are involved in these refractive errors, but the principles of development of the disorders and their manifestations are different. This is the main difference between the two diseases. Each of them has its own clinical picture if the diseases are diagnosed in isolation from each other.
Astigmatism has a congenital or acquired nature and is characterized by a change in the normal shape of the cornea or lens. As a result, light rays are refracted incorrectly, the focus points are shifted and the retina captures a distorted image. The consequence is that the eye sees objects blurry.
With myopia, objects are focused in front of the retina, and a person sees blurry objects only in the distance. Myopia combined with astigmatism complicates treatment.
So, the main difference between the two disorders is that with myopia a person sees objects blurry only in the distance, and with astigmatism - at any distance.
There are also different approaches to correcting the disease. For myopia, diverging (negative) lenses are recommended, for simple astigmatism - cylindrical ones.
Complex and mixed astigmatism is corrected using lenses that combine cylindrical and spherical components.
It should be borne in mind that wearing glasses in both cases does not eliminate the cause, therefore, if long-term wearing of glasses does not give a positive effect, they resort to surgical methods of treatment. For myopia, the operation can be performed at any age, and for astigmatism - only for adults.
Treatment of astigmatism and myopia
Modern treatment methods make it possible to get rid of visual impairments such as astigmatism and myopia in almost one hundred percent of cases. The following types of operations can be performed:
- laser correction;
- keratoplasty;
- eye lens replacement;
One of the most common ways to get rid of the disease is laser vision correction. The method has few contraindications, the operation is quick and painless and has a short recovery period. Keratoplasty or keratotomy is used in cases where laser correction is ineffective or has contraindications. In this case, in order to change the refractive power of the eyes, incisions are made on the cornea.
Sometimes it may be necessary to replace the cornea or lens. Such operations are performed with a high degree of astigmatism and myopia. The disadvantage of surgical intervention is that the cornea takes a long time to heal after surgery. In addition, keratoplasty does not guarantee 100% relief from the disease.
We would like to add that eye microsurgery is performed only on patients over 18 years of age.
Types and classifications
Myopic astigmatism is divided into simple and complex. In the first case, part of the rays is focused in front of the retina, the rest - on the retina. As a result, it turns out that myopia develops in one meridian of the eye, while in the other, vision remains normal.
With a complex version of astigmatism, all rays are collected only in front of the retina. Myopia is observed in both meridians of the eye, but with different values.
A complex version of myopic astigmatism, in turn, can be direct or reverse. Direct complex astigmatism involves changes on the vertical meridian; in the case of a simple variant, modifications occur on the horizontal meridian.
Read more about what complex myopic astigmatism is.
Myopic astigmatism can be congenital or acquired (the result of surgery or injury).
Depending on the location of the changes, corneal and lens types of myopic astigmatism are distinguished. The corneal variant is most often acquired, in cases where a toric deformation of the cornea occurs. The lens type of astigmatism is associated with the asymmetric structure or location of the lens.
Myopic astigmatism can have 3 degrees:
- Weak degree (less than 3 D) suggests slight distortion; a person may not even notice the disorder, and the symptoms of the disease are practically absent.
- Medium degree (3-6 diopters): in this case, symptoms and distortion are noticed by the patient.
- High degree (more than 6 diopters): vision is greatly distorted, as a result of which the patient sees all images elongated.
Symptoms
Myopic astigmatism can be recognized by a set of signs characteristic of both astigmatism and myopia. The main symptoms of the pathology are:
- gradual or sudden decrease in visual acuity;
- curvature of objects, blurred outlines;
- a feeling of objects slowly moving horizontally or vertically, objects shaking;
- splitting of objects, most often horizontally.
These symptoms can be mistaken for myopia, but they are distinguished from it by the presence of additional symptoms. For example, a patient complains of an inability to focus on an object. This sign is characteristic of astigmatism and is not entirely typical of myopia.
Constant uneven load on the eyes, the need to strain vision leads to the appearance of nonspecific symptoms: lacrimation, headaches, nausea. They appear mainly in the afternoon and intensify in the evening.
Pathology manifests itself somewhat differently in children. Unlike adults, who are able to compare normal vision with poor vision, they have no idea what it means to see clearly. Therefore, they do not have any complaints about blurry pictures. However, with close observation of the baby, you can understand that not everything is in order with his vision. Thus, in case of unilateral damage to the organs of vision, they try to exclude the “weak” eye from the process of perception. There can be several options for such manipulations: covering the eye with your hand, looking at objects and images with peripheral vision. Over time, the disease can be complicated by strabismus or amblyopia.
- 1. Myopia
- 2. Astigmatism
LECTURE No. 24. Myopia and astigmatism
1. Myopia
Myopia (myopia) is one of the variants of the refractive ability (clinical refraction) of the eye, which is formed simultaneously with a decrease in distance vision due to a mismatch in the position of the posterior main focus in relation to the central zone of the retina.
Myopia can be congenital (hereditary, intrauterine genesis); it progresses with age and can be malignant. Acquired myopia is a type of clinical refraction. Often, with age, it increases slightly and is not accompanied by noticeable morphological changes in the eyes. This process of refractogenesis is considered to be a biological variant. But under certain conditions, the frequency of both congenital and acquired myopic refraction is pathological in nature: the development of so-called progressive myopia occurs. This kind of myopia progresses in most children in the early school years, so it is often called “school-age”, although this is not entirely correct, since myopia can progress at a more mature age.
Causes of myopia
Myopia usually appears in childhood, progressing with age. The following factors are of great importance in the development of myopia:
1) genetic, in which myopic parents are more likely to have nearsighted children. Factors such as weakness of the accommodative muscle, weakness of connective tissue (the sclera becomes tensile, resulting in an increase in the length of the eyeball) can be inherited;
2) unfavorable environmental conditions, especially during prolonged work at a close distance from the eye. This is professional, school myopia, which easily develops with incomplete development of the body;
3) weakness of accommodation, leading to an increase in the length of the eyeball, or, on the contrary, tension of accommodation (inability of the lens to relax), which leads to spasm of accommodation.
In contrast to true myopia, with false myopia, vision is restored to normal with drug treatment (i.e., seven-day instillation of a 1% atropine solution). This requires careful observation and skiascopy with the participation of an ophthalmologist. Spasm of accommodation can be eliminated with the help of special therapeutic exercises for the eyes.
A person may suspect the initial signs of false myopia, or spasm of accommodation:
1) during visual work at close range, rapid eye fatigue, pain in the eyes, in the forehead, and in the temples may occur;
2) near visual work can often be facilitated by using weak plus lenses (in this case, this does not mean that the person is farsighted);
3) “setting” the eyes to different distances may be difficult or slow, especially when moving the gaze from a close object to a distant one;
4) distance vision deteriorates.
Spasm of accommodation, if left untreated, becomes persistent over time, is difficult to treat and can lead to true myopia.
Progressive myopia
Progressive myopia is any type of myopia that manifests itself as deterioration of distance vision. There is information about the antecedent of false myopia to true, i.e., this is a condition in which there is a more or less rapid and pronounced drop in distance visual acuity due to spasm, or tension, accommodation. However, after eliminating the spasm with the help of cycloplegic drugs (atropine, scopolamine, homatropine), vision is restored to normal, and refractometry reveals emmetropia or even farsightedness.
In recent decades, myopia (myopia) more often began to develop in preschoolers who, during their upbringing, had a high visual load in combination with a sedentary lifestyle, poor nutrition and weakening of the body due to frequent illnesses (tonsillitis, dental caries, rheumatism, etc.). Among students in the first and second grades, myopia occurs in 3–6%, in the third and fourth grades – in 6%, in the seventh and eighth grades – in 16%, in the ninth and tenth grades – in more than 20%. Severe (high, advanced) myopia causes over 30% of low vision and blindness from all eye diseases; it is an obstacle to the choice of many professions.
The mechanism of development of myopia that occurs during childhood consists of three main links, such as:
1) visual work at close range (weakened accommodation);
2) complicated heredity;
3) weakening of the sclera - disturbance of trophism (intraocular pressure).
Consequently, according to the predominance of certain causes of development, myopia can be conditionally divided into accommodative, hereditary and scleral.
The development of each of these forms of myopia over time leads to irreversible morphological changes in the eyes and a pronounced decrease in vision acuity, which is often small or does not improve at all under the influence of optical correction.
The main reason for this is a significant lengthening of the eye axis: instead of 22–23 mm, it reaches 30–32 mm or more, which is determined using an echo-ophthalmograph. If myopia progresses over the course of a year by less than 1.0 diopters, then it is conditionally considered benign, and if the increase is 1.0 diopters. and more – malignant. However, it is not only a matter of progression, but also of the size and changes in the intraocular structures (vitreous body, choroid, retina, optic nerve).
Large stretching of the eyes during myopia leads to widening of the palpebral fissure, resulting in the appearance of some kind of bulging eyes. The sclera becomes thinner, especially in the area of attachment of the lateralis muscles and near the edge of the cornea. This can be determined with the naked eye by the bluish tint of the cornea due to the transillumination of the choroid, and sometimes by the presence of anterior staphylomas of the sclera. The cornea also stretches and thins. The anterior chamber of the eye deepens. Mild iridodonesis (trembling of the iris), destruction or liquefaction of the vitreous body may occur. Depending on the genesis and magnitude of myopia, changes in the fundus occur. Changes to be distinguished include:
1) peridiscal light reflexes;
2) myopic cones;
3) true staphylomas;
4) changes in the area of the retinal spot;
5) cystic retinal degenerations;
6) retinal detachment.
Stretching of the sclera and atrophy of the pigment epithelium layer near the disc often lead to the appearance of myopic cones. Signs of high myopia are usually staphylomas, or true protrusions of the posterior sclera. In the area of the retinal spot, the most serious changes of a degenerative and atrophic nature occur with high myopia. The formation of cracks in the choroid in the form of yellowish or whitish stripes, and then the appearance of white polymorphic, often merging lesions with scattered lumps and accumulations of pigment are consequences of stretching of the posterior segment of the eyeball.
With the development of pathological changes in the area of the retinal spot, patients experience metamorphopsia (distortion of the shape and size of visible objects), weakened vision, ultimately leading to a strong decrease, and sometimes to an almost complete loss of central vision.
Progressive myopia occurs simultaneously with pathological changes at the extreme periphery of the fundus in the form of racemose retinal degeneration, and then multiple small defects of the slit-like, oval or round shape. Additional possibilities for the occurrence of retinal detachment explain changes in the vitreous body.
High myopia can sometimes appear in children in the first months of life, which suggests that such myopia is either hereditary or congenital. The latter develops as a result of diseases or underdevelopment in the antenatal period and is more common in children who have suffered a mild form of retrolental fibroplasia. Typically, this myopia is difficult to correct optically.
Prevention and treatment of myopia. To prevent progressive myopia, the following is necessary:
1) prevention of the development of myopia among the younger generation (primary prevention);
2) delaying the progression of already existing myopia (secondary prevention).
The beginning of the prevention of myopia or its development should occur with clarification of heredity and determination of clinical refraction in children under one year of age, but not later than 12 years of age. At the same time, there should be a differentiated attitude towards raising a child, taking into account the state of his heredity and refraction. To do this, children should be divided into two groups:
1) children with a family history of myopia, regardless of the detected value and type of refraction, with congenital myopia, with emmetropia;
2) children with farsighted refraction without a history of myopia.
These are the so-called prevention groups (risk groups). Ophthalmologists must transmit lists of these groups to kindergartens and schools annually in July-August.
Treatment of myopia can be conservative or surgical. Conservative treatment begins with vision correction using glasses or contact lenses.
It is necessary to have glasses that are comfortable and that they correspond to the configuration and size of the face, to ensure visual acuity in both eyes within the range of 0.9–1.0 and to have stable binocular vision. You should wear glasses constantly. In cases of moderate or high myopia, you can use bifocal glasses so that the lower hemisphere of the lens is weaker than the upper hemisphere by an average of 2.0–3.0 diopters. For high myopia and anisometropia (more than 3.0 diopters), correction with hard or soft contact lenses is recommended.
Treatment of rapidly progressive and severe myopia is a serious and often difficult task. The development of changes in the area of the retinal spot, the appearance of recurrent hemorrhages in the retina and vitreous body require cessation of visual work, creation of rest for the eyes, protection of them from harsh light and vigorous treatment. Both local and general treatment with calcium chloride, cysteine, Chinese Schisandra, ginseng, mezatone, ethylmorphine hydrochloride (dionine), as well as subconjunctival oxygen injections and reflexology are recommended. It is necessary to prescribe rutin with ascorbic acid, riboflavin, thiamine, vitamin E, intermedin, adenosine triphosphoric acid, taufon, etc.
If correction with glasses or contact lenses, conservative treatment methods, as well as reflexology do not stop or significantly reduce the rate of progression of the process, then surgical treatment is indicated. The decision on the timing and method of surgery is made depending on a number of factors. The younger the child, the faster the annual (over two to three years) progression of myopia (by more than 1.0 diopters per year), the more significant the increase in the sagittal size of the eye, the greater the indications for strengthening the eye capsule - scleroplasty. The choice of scleroplasty technique is made in accordance with the stage of myopia, i.e., the location and magnitude of morphological changes. It is necessary to take into account that the less myopia, the more effective scleroplasty. Prevention of rapid progression of myopia through scleroplasty is effective in almost 90% of cases. Within two to three years after surgery, myopia often increases by 1.0 diopters. versus 3.0–4.0 diopters. with a conservative method of treatment. If myopia is stable for two to three years, but the child who has reached adulthood does not want to wear glasses and contact lenses or if it is impossible to ensure high visual acuity with their help, a keratotomy can be performed, i.e., non-through incisions on the cornea, due to which reduces its refractive power by a given amount. Keratotomy is most effective for low and moderate myopia, and for high myopia, keratomileusis is possible.
Treatment of accommodative false myopia primarily requires limiting visual work at close range, correct correction of existing ametropia and anisometropia. The main methods of treatment are various training exercises for the ciliary muscle, instillation of medications prescribed by an ophthalmologist, as well as reflexology.
2. Astigmatism
Astigmatism is a refractive error in which different types of ametropia or different degrees of one type of ametropia are combined in one eye.
Etiopathogenesis of astigmatism and its forms. The development of astigmatism is based on unequal refraction of light rays in different meridians of the eye, which is associated with differences in the radius of curvature of the cornea (less often the lens). The strongest and weakest refractive power is observed on the two main mutually perpendicular meridians. As a result of this feature, the image on the retina is always unclear and distorted. As a rule, the cause is an abnormality in the structure of the eye. However, such changes can occur after operations, eye injuries, and corneal diseases.
There is simple astigmatism, in which emmetropia is noted in one of the main meridians, and ametropia (myopia or hypermetropia) in the other; complex astigmatism, when ametropia of the same type, but of varying degrees, is noted in both main meridians of the eye; mixed astigmatism, in which myopia is noted in one of the main meridians and hypermetropia in the other.
In astigmatic eyes there are main meridians with the strongest and weakest refractive power. If the refractive power is the same throughout the meridian, then astigmatism is called correct; if it is different, it is called incorrect.
With direct astigmatism, the vertical main meridian has the strongest refraction, and with reverse astigmatism, the horizontal one has the strongest refraction. When the main meridians pass in an oblique direction, they speak of astigmatism with oblique axes. Correct direct astigmatism with a difference in refractive power in the main meridians of 0.5 diopters. considered physiological, not causing subjective complaints.
Clinical picture and diagnosis of astigmatism. Patients complain of decreased visual acuity, rapid eye fatigue during work, headaches, and sometimes seeing objects as curved. Spherical convex and concave glasses do not improve vision. A refractive study reveals differences in the refractive power of the eye in different meridians. The basis of the diagnosis is to determine refraction in the main refractive meridians.
Treatment of astigmatism. Glasses with cylindrical or spherocylindrical lenses (astigmatic lenses) are prescribed. Constantly wearing such glasses maintains high visual acuity and good performance.
Table of contents
Causes
Ophthalmologists call the main cause of myopic astigmatism a genetic predisposition to the disease. According to statistics, 63% of patients with this diagnosis had relatives who were nearsighted or suffering from astigmatism. The risk is highest in children whose both parents suffer from myopia, astigmatism or other visual impairments.
In addition to congenital forms of the disease, there is an acquired disease, the cause of which may be:
- mechanical injury to the eye shell;
- penetrating or blunt trauma to the eyeball with displacement or damage to the lens;
- complications after surgical or minimally invasive eye interventions;
- a long-term inflammatory process of the outer membranes or internal structures of the eye;
- vascular abnormalities of the head and organs of vision;
- systemic diseases leading to a regular increase in intraocular pressure.
The environmental situation plays a significant role in the risk of myotonic syndrome with subsequent curvature of the lens and changes in the shape of the cornea. There are a number of substances that, when they come into contact with the membrane of the eye, seriously change the structure of the tissues of the cornea, then the vitreous body, etc.
It is important! In 40% of adult patients, pathology occurs if astigmatism has not been treated or myopia corrected through surgery or glasses. More than 50% of such diagnoses are made to office workers who spend most of the day at the computer.