Superior rectus muscle
The superior rectus muscle
(
m. rectus superior
) lifts the eyeball and turns it inward. At the same time, the gaze is directed upward and inward by 25. The eyeball in the socket simultaneously moves slightly posteriorly. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The single synergistic muscle below contracts simultaneously to move the other eye in the same direction.
Start
- Common tendon ring
Attachment
- Top of the eyeball, anterior to its equator
Innervation
- Superior branch of the oculomotor nerve (III pair of cranial nerves)
Functions
- Synergist in the other eye
Look up. Functional muscle tests
Clinical relevance
- Damage to any branch of the oculomotor nerve leads to double vision. An experienced doctor can determine the affected nerve by looking in the direction in which double vision increases. The distance between the two images increases if the patient is asked to move the affected muscle.
Issues and comments
- The left inferior oblique muscle simultaneously directs the gaze of the left eye up and to the right.
- The right inferior oblique muscle simultaneously directs the gaze of the right eye up and to the left.
Diagnosis of pathology
If you experience discomfort in your eyes, you should consult an ophthalmologist. The doctor will talk with the patient, examine the affected eye and check visual acuity. After this, the patient is sent for additional examination, which includes a number of the following procedures:
- serological studies that are carried out when the disease is infectious;
- Ultrasound;
- CT or MRI;
- measurement of intraocular pressure;
- gonioscopy - examination of the anterior chamber of the eyes;
- biomicroscopy - study of the structures of the visual apparatus using a microscope;
- ophthalmoscopy;
- electromyography.
Inferior rectus muscle
Inferior rectus muscle
(
m. rectus inferior
) lowers his gaze and turns it inward towards the nose. The eyeball in the orbit simultaneously moves slightly posteriorly. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The single synergistic muscle below contracts simultaneously to move the other eye in the same direction.
Start
- Common tendon ring
Attachment
- Bottom of the eyeball, anterior to its equator
Innervation
- Inferior branch of the oculomotor nerve (III pair of cranial nerves)
Functions
- Synergist in the other eye m. obliquus superior
Look down and medially. Functional muscle tests
Clinical relevance
- Damage to any branch of the oculomotor nerve leads to double vision. An experienced doctor can determine the affected nerve by looking in the direction in which double vision increases. The distance between the two images increases if the patient is asked to move the affected muscle.
Issues and comments
- The left superior oblique muscle simultaneously directs the gaze of the left eye down and to the right.
- The right inferior oblique muscle simultaneously directs the gaze of the right eye down and to the left.
- To more accurately determine the direction of gaze, the examiner can lift the patient's eyelids.
Superior oblique muscle
The superior oblique muscle (m. obliquus superior) turns the eyeball inward towards the nose, lowers and averts the gaze to the temple. The eyeball in the orbit simultaneously moves slightly anteriorly, so this muscle acts as an antagonist to the external rectus muscles of the eyeball. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The only synergistic muscle. below is contracted simultaneously to move the other eye in the same direction.
Start
- Wall of the orbit medial to the optic nerve canal
Attachment
- Top of the eyeball, temporal side, posterior to the equator
Innervation
- Trochlear nerve (IV pair of cranial nerves)
Peculiarities
The superior oblique muscle block acts as a lever pivot point for the muscle tendon
Functions
- Synergist in the other eye m. rectus inferior
Look down. Functional muscle tests
Clinical relevance
- Paresis of this muscle causes only a slight deviation of the eyeball. The only noticeable thing is that the head turns and tilts to the healthy side to compensate for the lesion. When the head is tilted to the affected side, the eyeball deviates upward while fixing the gaze with the healthy eye (Bilschowsky's symptom).
Issues and comments
The left inferior rectus muscle simultaneously directs the gaze of the left eye down and to the left.
- The right inferior rectus muscle simultaneously directs the gaze of the right eye down and to the right.
- To more accurately determine the direction of gaze, the examiner can lift the patient's eyelids.
Inferior oblique muscle
Inferior oblique muscle
(
m. obliquus inferior
) turns the eyeball outward and directs the gaze upward and sideways to the temple. The eyeball in the orbit simultaneously moves slightly anteriorly, so this muscle acts as an antagonist to the external rectus muscles of the eyeball. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The single synergistic muscle below contracts simultaneously to move the other eye in the same direction.
Start
- Base of the orbit, lateral to the nasolacrimal duct
Attachment
- Temporal side of the eyeball, posterior to the equator
Innervation
- Inferior branch of the oculomotor nerve (III pair of cranial nerves)
Functions
- Synergist in the other eye m. rectus superior
Look up. Functional muscle tests
Clinical relevance
- Damage to any branch of the oculomotor nerve leads to double vision. An experienced doctor can determine the affected nerve by looking in the direction in which double vision increases. The distance between the two images increases if the patient is asked to move the affected muscle.
Issues and comments
- The left superior rectus muscle simultaneously directs the gaze of the left eye up and to the left.
- The right superior rectus muscle simultaneously directs the gaze of the right eye upward and to the right.
Oculomotor muscles
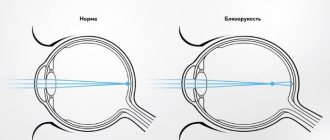
The oculomotor apparatus is a complex sensorimotor mechanism, the physiological significance of which is determined by its two main functions: motor (motor) and sensory (sensitive).
The motor function of the oculomotor system ensures the guidance of both eyes, their visual axes and the central fossae of the retinas to the object of fixation, while the sensory function ensures the merging of two monocular (right and left) images into a single visual image. The innervation of the extraocular muscles by the cranial nerves determines the close connection between neurological and ocular pathologies, as a result of which an integrated approach to diagnosis is necessary.
The constant stimulus for adduction (to ensure orthophoria) caused by the divergence of the orbits explains the fact that the medial rectus muscle is the most powerful of the rectus extraocular muscles. The disappearance of the stimulus for convergence with the onset of amaurosis leads to a noticeable deviation of the blind eye towards the temple.
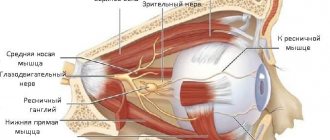
All rectus muscles and the superior oblique begin in the depths of the orbit on the common tendon ring (anulus tendineus communis), fixed to the sphenoid bone and periosteum around the optic canal and partially at the edges of the superior orbital fissure. This ring surrounds the optic nerve and ophthalmic artery. The muscle that lifts the upper eyelid (m. levator palpebrae superioris) also begins from the common tendon ring. It is located in the orbit above the superior rectus muscle of the eyeball, and ends in the thickness of the upper eyelid. The rectus muscles are directed along the corresponding walls of the orbit, on the sides of the optic nerve, forming a muscular funnel, pierce the vagina of the eyeball (vagina bulbi) and with short tendons are woven into the sclera in front of the equator, 5-8 mm away from the edge of the cornea. The rectus muscles rotate the eyeball around two mutually perpendicular axes: vertical and horizontal (transverse).
Movements of the eyeball are carried out with the help of six extraocular muscles: four straight muscles - external and internal (m. rectus externum, m. rectus internum), upper and lower (m. rectus superior, m. rectus inferior) and two obliques - upper and lower ( m.obliguus superior, m.obliguus inferior).
The superior oblique muscle of the eye originates from the tendon ring between the superior and internal rectus muscles and goes anteriorly to the cartilaginous block located in the upper inner corner of the orbit at its edge. At the pulley, the muscle turns into a tendon and, passing through the pulley, turns posteriorly and outward. Located under the superior rectus muscle, it is attached to the sclera outward from the vertical meridian of the eye. Two-thirds of the entire length of the superior oblique muscle is between the apex of the orbit and the trochlea, and one-third is between the trochlea and its attachment to the eyeball. This part of the superior oblique muscle determines the direction of movement of the eyeball during its contraction.
In contrast to the five muscles mentioned, the inferior oblique muscle of the eye begins at the inferior internal edge of the orbit (in the area of the entrance of the nasolacrimal canal), goes posteriorly outward between the orbital wall and the inferior rectus muscle towards the external rectus muscle and is fan-shaped attached under it to the sclera in the posterior external region eyeball, at the level of the horizontal meridian of the eye.
Numerous cords extend from the fascial membrane of the extraocular muscles and Tenon’s capsule to the orbital walls.
The fascial-muscular apparatus ensures a fixed position of the eyeball and gives smoothness to its movements.
Some elements of the anatomy of the extrinsic muscles of the eye
Superior rectus muscle (m. rectus superior)
Origin : Lockwood's superior orbital tendon (a fragment of the common tendon ring of Zinn) in close proximity to the perineural sheath of the optic nerve.
Attachment : to the sclera 6.7 mm from the limbus at an angle to it and slightly medial to the vertical axis of rotation of the eyeball, which explains the variety of its functions.
Functions : primary - supraduction (75% of muscle effort), secondary - incycloduction (16% of muscle effort), tertiary - adduction (9% of muscle effort).
Blood supply: superior (lateral) muscular branch of the ophthalmic artery, as well as the lacrimal, supraorbital and posterior ethmoidal arteries.
Innervation: superior branch of the ipsilateral oculomotor nerve (n. III). Motor fibers penetrate this and almost all other muscles, usually at the border of its posterior and middle thirds.
Anatomy details: Inserted behind the ora serrata. As a consequence, perforation of the sclera when applying a frenulum suture will lead to a retinal defect. Together with the levator palpebrae superioris muscle, it forms the superior muscle complex
Inferior rectus muscle (m. rectus inferior)
Origin: inferior orbital tendon of Zinn (fragment of the common tendon ring of Zinn).
Attachment: to the sclera 5.9 mm from the limbus at an angle to it and slightly medial to the vertical axis of rotation of the eyeball, which explains the variety of its functions.
Function: primary - infraduction (73%), secondary - excycloduction (17%), tertiary - adduction (10%).
Blood supply : lower (medial) muscular branch of the ophthalmic artery, infraorbital artery.
Innervation : inferior branch of the ipsilateral oculomotor nerve (n. III).
Anatomy details : forms the inferior muscle complex with the inferior oblique muscle
Lateral rectus muscle (m. rectus lateralis)
Beginning : main (medial) leg - the superior orbital tendon of Lockwood (a fragment of the common tendon ring of Zinn); non-permanent (lateral) leg - a bony protrusion (spina recti lateralis) in the middle of the lower edge of the superior orbital fissure.
Attachment : to the sclera 6.3 mm from the limbus.
Function : primary - abduction (99.9% of muscle effort).
Blood supply : superior (lateral) muscular artery from the ophthalmic artery, lacrimal artery, sometimes infraorbital artery and inferior (medial) muscular branch of the ophthalmic artery.
Innervation : ipsilateral abducens nerve (n.VI).
Anatomy details : has the most powerful fixing ligament
Medial rectus muscle (m. rectus medialis)
Origin : Lockwood's superior orbital tendon (a fragment of Zinn's tendon ring) in close proximity to the perineural sheath of the optic nerve.
Attachment : to the sclera 5 mm from the limbus.
Function: primary - adduction (99.9% muscle effort).
Blood supply : lower (medial) muscular branch of the ophthalmic artery; posterior ethmoidal artery.
Innervation: inferior branch of the ipsilateral oculomotor nerve (n. III).
Anatomy details: the most powerful extraocular muscle
Inferior oblique muscle (m. obliquus inferior)
Beginning: the periosteum of the flattened area of the orbital surface of the upper jaw under the anterior lacrimal ridge at the opening of the nasolacrimal canal.
Attachment : the posterior outer surface of the eyeball slightly behind the vertical axis of rotation of the eyeball.
Function : primary - excycloduction (59%), secondary - supraduction (40%); tertiary - abduction (1%).
Blood supply : lower (medial) muscular branch of the ophthalmic artery, infraorbital artery, rarely - lacrimal artery.
Innervation: the inferior branch of the contralateral oculomotor nerve (n. III), running along the outer edge of the inferior rectus muscle and penetrating the inferior oblique muscle at the level of the equator of the eyeball, and not at the border of the posterior and middle third of the muscle, as happens with all other extraocular muscles . This 1–1.5 mm thick trunk (containing parasympathetic fibers innervating the pupillary sphincter) is often damaged during reconstruction of a fracture of the inferior wall of the orbit, leading to postoperative Adie syndrome.
Anatomy Details: Absence of tendon explains the bleeding that occurs when the muscle is cut from the sclera
Superior oblique muscle (m. obliquus superior)
Origin : periosteum of the body of the sphenoid bone above the superior rectus muscle.
Attachment: sclera of the postero-superior quadrant of the eyeball.
Function: primary - incycloduction (65%), secondary - infraduction (32%), tertiary - abduction (3%).
Blood supply : superior (lateral) muscular artery from the ophthalmic artery, lacrimal artery, anterior and posterior ethmoidal arteries.
Innervation: contralateral trochlear nerve (n. IV).
Anatomy details: longest tendon (26 mm), pulley - functional origin of the muscle
Medial rectus muscle
Medial rectus muscle
(
m. rectus medialis
) leads the gaze to the nose; with an isolated contraction, this movement is carried out only in the horizontal plane. The eyeball in the orbit simultaneously moves slightly posteriorly. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The single synergistic muscle below contracts simultaneously to move the other eye in the same direction.
Start
- Common tendon ring
Attachment
- Medial side of the eyeball, anterior to the equator
Innervation
- Inferior branch of the oculomotor nerve (III pair of cranial nerves)
Functions
- Synergist in the other eye m. rectus lateralis
Bringing the gaze to the nose. Functional muscle tests
Clinical relevance
- Damage to any branch of the oculomotor nerve leads to double vision. An experienced doctor can determine the affected nerve by looking in the direction in which double vision increases. The distance between the two images increases if the patient is asked to move the affected muscle.
Issues and comments
- When gaze is adducted, the medial rectus muscle is tested in the test eye, and the lateral rectus muscle in the opposite eye.
How is ocular myositis treated?
An important element of therapy is massage.
After the diagnosis identifies the causes of inflammation of the eye muscles, therapeutic measures are prescribed. Etiotropic treatment is indicated only in cases of infectious origin of the disease, and in other situations symptomatic treatment is used. Conservative therapy includes various medications, and in case of traumatic injuries, surgery is performed to restore the structure of damaged muscle fibers. To treat ocular myositis, the following methods are used:
- Antibiotics with a broad spectrum of action in the form of subcutaneous injections in the lower eyelid area.
- NSAIDs to relieve pain and inflammation.
- Angioprotectors that strengthen the walls of blood vessels and prevent the development of retinal pathologies.
- Hormonal agents. They are used in cases of severe disease and the absence of a positive result from taking NSAIDs.
- Radiotherapy. It is used when classical treatment methods are insufficiently effective and to prevent recurrent disease.
- Physiotherapy, including electrophoresis with drugs, thermal procedures, massage.
- Osmotherapy is the introduction of hypertonic solutions to change the pressure of the internal environment.
For 3 months after completion of the treatment course, the patient should be regularly monitored by an ophthalmologist.
Lateral rectus muscle
Lateral rectus muscle
(
m. rectus lateralis
) looks away to the temple; with an isolated contraction, as for the medial rectus muscle, this movement is carried out only in the horizontal plane. The eyeball in the orbit simultaneously moves slightly posteriorly. Depending on the direction of gaze, other muscles of the eyeball can act as both synergists and antagonists. The single synergistic muscle below contracts simultaneously to move the other eye in the same direction.
Start
- Common tendon ring
Attachment
- Lateral side of the eyeball, anterior to the equator
Innervation
- Abducens nerve (VI pair of cranial nerves)
Functions
- Synergist in the other eye m. rectus medialis
Functional muscle tests
Clinical relevance
- Damage to any branch of the oculomotor nerve leads to double vision. An experienced doctor can determine the affected nerve by looking in the direction in which double vision increases. The distance between the two images increases if the patient is asked to move the affected muscle.
Issues and comments
- When looking away, the lateral rectus muscle is tested in the test eye, and the medial rectus muscle in the opposite eye.
Clinic of the lesion
Complete damage to the oculomotor nerve
Complete defeat of the n.oculomotorius is accompanied by a characteristic syndrome.
- Ptosis (drooping of the eyelid) is caused by paralysis of the m.levator palpebrae superior.
- Divergent strabismus (lat. strabismus divergens) - a fixed position of the eye with the pupil directed outward and slightly downward due to the action of the unresisting m.rectus lateralis (innervated by the VI pair of cranial nerves) and m.obliquus superior (innervated by the IV pair of cranial nerves - block (lat. n.trochlearis)).
- Diplopia (double vision) is a subjective phenomenon that occurs when the patient looks with both eyes. The severity of double vision increases when the gaze is fixed on a nearby object or when trying to turn the gaze towards the paralyzed internal rectus muscle of the eye. In this case, the image of the focused object in both eyes is obtained not on the corresponding, but on different zones of the retina. Double vision of the object in question occurs as a result of deviation of the visual axis of one eye due to muscle weakness due to impaired innervation. In this case, the image of the object in question falls in the correctly fixating eye on the central fovea of the retina, and with a deviation of the axis - on the non-central part of the retina. In this case, the visual image, in association with habitual spatial relationships, is projected into the place in space where the object should be located in order to cause irritation of this particular part of the retina, given the correct position of the visual axis of this eye.
- Mydriasis (pupil dilation) with lack of pupillary response to light and accommodation. Mydriasis occurs due to the fact that the n.oculomotorius innervates the m.sphincter pupillae. The absence of a reaction to light and convergence is due to the fact that this nerve is part of the reflex arc of the pupillary reflex to light.
- Paralysis of accommodation causes deterioration of vision at close distances. Accommodation of the eye is a change in the refractive power of the eye to adapt to the perception of objects located at different distances from it. Accommodation is ensured by the state of the curvature of the lens, which is regulated by m.ciliaris. Since this internal muscle of the eye is innervated by the oculomotor nerve, if it is damaged, paralysis of accommodation will be observed.
- Convergence palsy is characterized by the inability to rotate the eyeballs inwards. Eye convergence is the bringing together of the visual axes of both eyes when viewing close objects. It is carried out due to the simultaneous contraction of the m.rectus medialis of both eyes; accompanied by constriction of the pupils (miosis) and strain of accommodation. Since the m.rectus medialis is innervated by the oculomotor nerve, and the state of the pupil and accommodation also depend on its impulses, when the n.oculomotorius is damaged, convergence of the eyes becomes impossible.
- Limitation of the movement of the eyeball up, down and inward - due to paralysis of the muscles innervated by the oculomotor nerve.
- In addition to the above symptoms, due to loss of tone of the external muscles of the eye, slight exophthalmos may be observed.
Damage to the n.oculomotorius is determined by the above violations. Complete loss of function is more often observed with peripheral lesions. Due to the dismemberment and certain distance of the cell groups of the nuclei of the III nerve from each other, when the pathological focus is localized in the area of their location, a clinical picture of damage not to all muscles innervated by the III nerve, but only to some of them, may develop.
Argyll Robertson syndrome
In patients, one can encounter a dissociation between the reaction of the pupils to light and their reaction to accommodation and convergence. Loss or suppression of the pupils' reactions to light while their reaction to accommodation and convergence is preserved is called Argyle Robertson syndrome. This syndrome is considered characteristic of neurosyphilis. The reverse syndrome to Argyll Robertson's syndrome, in which the reaction to light is preserved, but their reaction to accommodation and convergence is impaired, often occurs in epidemic Economo encephalitis, especially in its chronic stage in combination with signs of parkinsonism.
Alternating syndromes with damage to the oculomotor nerve
Symptoms of damage to the n.oculomotorius can occur in the presence of a pathological focus in the midbrain. Weber's syndrome is characterized by paralysis of the muscles innervated by the oculomotor nerve on the side of the lesion, and central hemiplegia on the side opposite to the lesion. It usually occurs when the base of the cerebral peduncle is damaged.
Benedict's syndrome - consists of paralysis of the muscles innervated by the oculomotor nerve on the side of the pathological focus, combined with choreoathetosis and intention tremor in the opposite limbs (damage to the dentorubral tract and red nucleus). The syndrome occurs when the pathological focus is localized in the medial part of the midbrain tegmentum.
Claude's syndrome is paralysis of the oculomotorius on the side of the lesion, and cerebellar pathology on the opposite side. Occurs when the posterior part of the red nucleus and the third nerve root passing through it are damaged (inferior nucleus ruber syndrome).
With a large pathological focus in the midbrain, Nothnagel syndrome may develop. Then cerebellar ataxia, intention tremor, sometimes choreoid hyperkinesis, paralysis of the muscles that provide movement of the eyeballs and deafness occur on both sides. Nothnagel syndrome is caused by combined damage to the red nuclei and roots of the third nerve and medial geniculate bodies.
Lesion in the area of the cavernous sinus and superior orbital fissure
If the pathological process affects the outer wall of the cavernous venous sinus, in which the nerves that provide movements of the eyeball pass (III, IV and VI and the first branch of the V nerve), then the patient experiences paralysis of the eyeball (ophthalmoplegia), pain or hypoesthesia in the area of innervation of the first branches of the trigeminal nerve, as well as swelling of the tissues of the eyeball and eyelids, due to a violation of the outflow of venous blood from them (Foix's syndrome). When the pathological process is localized in the area of the superior orbital fissure, the same symptoms occur, but without the phenomena of swelling of the tissues of the orbital area (superior orbital fissure syndrome).
The structure of the eye muscles
It is customary to distinguish six oculomotor muscles, four of them go in a forward direction and are called rectus muscles: internal, external, superior, inferior. The remaining two have a slightly oblique direction of movement, as well as a way of attaching the eye to the apple, and therefore are called oblique: upper and lower.
All muscles, excluding the inferior oblique, originate in a dense connective tissue ring that surrounds the external opening in the optic canal. At the very beginning, 5 muscles form a kind of muscular funnel, where the optic nerve, blood vessels and nerves pass. Afterwards, the superior oblique muscle gradually deviates upward and inward, moving towards the so-called block. This is the place where the muscle transforms into a tendon, thrown through the pulley loop, which is why it changes direction to oblique, then attaching in the area of the upper outer quadrant of the eyeball below the superior rectus muscle. The inferior oblique muscle originates from the inferior internal orbital margin, passes below the inferior rectus muscle outward and posteriorly, and is attached in the region of the inferior external quadrant of the eyeball.
In the immediate vicinity of the eyeball, the muscles have a superficial layer of dense capsule of Tenon's membrane. Their attachment to the sclera occurs at different distances from the limbus. The internal rectus muscle is attached especially close to the limbus of the rectus muscles, and the superior rectus muscle is further away from the rest. The oblique muscles are attached to the apple of the eye slightly behind the equator of the eyeball - the middle of its length.
The work of muscles is largely regulated by the oculomotor nerve. It controls the internal, superior, inferior oblique and inferior rectus muscles. The functions of the external rectus muscle are controlled by the abducens nerve, while the superior oblique muscle is controlled by the trochlear nerve. The peculiarity of such nervous regulation is that one branch of the motor nerve controls the work of a very small number of muscle fibers, which allows for maximum accuracy in eye movements.
The movements of the eyeball depend entirely on the characteristics of the muscle attachment. The attachment zone of the external and internal rectus muscles corresponds to the horizontal plane of the eyeball, which provides horizontal movements: turning them towards the nose (contraction of the internal rectus muscle) or towards the temple (contraction of the external rectus muscle).
The inferior and superior rectus muscles provide mainly vertical eye movements, but due to the fact that the line of muscle attachment is localized somewhat obliquely in relation to the limbus line, along with the vertical movement of the eyes, their inward movement also occurs.
The oblique muscles, when contracting, cause more complex movements, this is due to certain features of the location of the muscles, as well as their attachment to the sclera. The function of the superior oblique muscle is to lower and rotate the eye outward, and the function of the inferior oblique muscle is to lift it and move it outward.
At the same time, the superior and inferior rectus muscles and oblique muscles are capable of providing slight rotations of the eye clockwise or counterclockwise. Good nervous regulation, as well as coordinated work of the muscles of the eyeball, make it possible to perform complex movements: unilateral or directed in different directions, which ensures the volume and quality of vision, its binocularity.
Functional Features
The function and anatomy of the extraocular muscles are interrelated. Since due attention has already been paid to the structure, now we will analyze in more detail the function of this type of muscle tissue, without which a person will not be able to correctly perceive the world around him.
The main functional feature is the ability to provide full eye movement in different directions:
- Bringing to one point, that is, there is a movement, for example, to the nose. This feature is provided by the internal rectus and additionally the superior inferior rectus muscle tissue.
- Abduction, that is, movement occurs to the temporal region. This feature is provided by the external rectus muscle and additionally by the superior and inferior oblique muscle tissues.
- The upward movement occurs due to the correct functioning of the superior rectus and inferior oblique muscles.
- The downward movement occurs due to the proper functioning of the inferior rectus and superior oblique muscle tissue.
All movements are complex and coordinated with each other.
Diagnostic methods
- Visual study of eye mobility, assessing the completeness of movements when tracking a moving object.
- Strabometry assessment of the angle of deviation of the eye in case of strabismus from the midline.
- A test with alternate covering of the eyes, which determines hidden strabismus heterophoria, and in case of obvious strabismus, determines its type.
- Ultrasound diagnostics to determine lesions of the oculomotor muscles localized close to the eyeball.
- Magnetic resonance imaging, computed tomography detects lesions of the extraocular muscles along the entire length.
Accessory muscles
In addition to the above fibers, other tissues that surround the palpebral fissure also take part in the work and mobility of the eyeball. In this case, the orbicularis muscle is considered the most important. It has a unique structure, which is represented by several parts - orbital, lacrimal and eyelid.
So, the abbreviation:
- the orbital part occurs due to the straightening of the transverse folds, which are located in the frontal region, as well as by lowering the eyebrows and reducing the eye slit;
- the secular part occurs by closing the slit of the eyes;
- lacrimal part is carried out due to the enlargement of the lacrimal sac.
All three of these areas that make up the orbicularis muscle are located around the eyeball. Their beginning is located directly near the medial angle on the bone base. Innervation occurs through a small branch of the facial nerve. It is necessary to understand that any contraction or tension of the extraocular muscles of any type occurs with the help of nerves.
Exercises for the main muscles of the eye
External eye muscle training
An effective set of exercises allows you to strengthen your external muscles. This ensures a higher quality and three-dimensional image. Regular exercise helps to achieve good vision and maintain healthy visual organs.
Training:
- Blink quickly for 20 seconds. Close your eyes and open them wide. Blink quickly again.
- Imagine that there is a rainbow in front of your eyes. Smoothly walk around the arc from one end to the other and back. Then imagine an inverted rainbow. Make arcuate movements with your eyes, lingering for a few seconds at the extreme points and lower part of your field of vision.
- Look straight ahead. Imagine that this is the center of the spiral. Make rotational movements with your eyes along a spiral trajectory. With each revolution, increase the diameter of the coil along which the gaze follows. Try to rotate your eyes a little further, beyond the limits of comfort.
- In a sitting position, slowly move your gaze from top to bottom, then from right to left. Repeat the exercise 12 times.
Training the internal muscles of the eye
The ciliary muscle of the visual analyzer is trained using the mark on glass method and an accomodo trainer.
Exercise mark on glass:
- Attach a round mark to the window glass. It should be at eye level.
- Sit 30 cm further from her.
- Move your eyes to the mark and a distant object behind the glass (tree, car, walking person).
Perform the gymnastic complex 2 times a day for 3 minutes. After 2 days, increase the training duration to 5 minutes, after another 2 days to 10 minutes.
To make an accomodo trainer, you will need to cut out a figure from thick cardboard, similar to a table tennis racket. Make a 50 cm long slot above the handle into which a ruler can fit.
Draw the letter C in the center of the figure. Put on glasses or lenses, add an additional lens at +3 to one of the glasses. Close the second eye. Place a ruler next to the open one, slowly move the rocket along it until the contours of the letters merge into a circle.
Perform 710 minutes of training with each eye.
Exercises for the six main muscles of the eye
Gymnastics is performed standing in a relaxed state. Do not move your head or body while performing the exercises.
Complex:
- Look at the ceiling, then at the floor. Do not move quickly, the eyes must do the work intended for them. Shift your gaze slowly, without looking at foreign objects.
- Move your gaze to the right and left. Move your eyes to the sides as far as the extraocular muscles allow. Do not try to complete the exercise if there is pain. In the future, this exercise will make the muscles more elastic and you will be able to completely look away to the side.
- Draw lines diagonally. Stand with your back to the wall. Move your eyes from the upper right corner of the room to the lower left. Then do the exercise in reverse. This workout strengthens the muscles, it loads them and makes them function fully.
- Take a hoop and hang it in front of your eyes or imagine a large circle. Slowly roll your eyes along the line of the hoop. The gaze should glide smoothly along the rim.
Each exercise is repeated 10 times. One workout a day is enough. This complex allows you to load all 6 muscles of the visual analyzer. If you do the work regularly, you will be able to significantly strengthen them.
Training exercises
In any situation, a violation of eye movement can occur, so at the first manifestations of a deviation, you should immediately contact a specialist who, after a thorough examination, will be able to prescribe effective treatment. In most cases, diseases and pathologies of muscle tissue are eliminated surgically. To avoid any complications and interventions, constant training of the extraocular muscles should be carried out.
Examples
- Exercise 1 – for external muscles. To relax not only muscle tissue, but also the eyes, you need to blink quickly for half a minute. Then rest and repeat the exercise again. Helps after a working day and long periods of sitting at the computer.
- Exercise 2 – for internal muscles. You need to place your finger in front of your eyes at a distance of 0.3 m and look at it carefully for several seconds. Then take turns closing your eyes, but continue to look at him. Then look carefully at the tip of your finger for 3-5 seconds.
- Exercise 3 – to strengthen the underlying tissues. The body and head should be motionless. You need to move your eyes right and left. Abduction to the side should be maximum. You need to do the exercise at least 9-11 times.
Additional exercises
Training the eye muscles is necessary not only for nearsighted and farsighted people, but also for absolutely healthy people. It allows you to strengthen the oculomotor muscles, prevent rapid aging and age-related diseases.
Additional complex:
- Blink quickly. This exercise will relax you.
- Draw a rectangle with your eyes. Draw one figure, blink quickly and draw your eyes in the other direction.
- Draw a bow and a star with your eyes.
- Horizontal and vertical spiral. Imagine a log in front of you, wind a wire around it with your finger, following the movement of your finger with your eyes.
- Place your index fingers in front of you. Move. Slowly move your fingers apart, watching them. Delay in different positions for 1 second.
- Stretch your hand forward with your index finger straightened. Look at it, slowly pulling it towards your nose. Turn your gaze to an object located further away.
Each exercise is repeated several times. It is recommended to do the entire set of exercises 2 times a week for healthy people and 1 time daily for patients with myopia or hypermetropia.
Predictions and prevention
If the disease is severe, the person may lose the ability to see.
With timely initiation of therapy, the functionality of the eye muscles can be completely restored. If the disease has become chronic, the patient must regularly undergo preventive courses of treatment to avoid relapses and complications. In severe cases and advanced pathology, the prognosis is unfavorable. Most often, patients completely lose vision or their eye muscles atrophy.
To prevent orbital myositis, you need to follow the rules of visual hygiene when working at a computer for long periods of time, avoid drafts and strong cooling. When working in production, you should always wear eye protection - goggles, masks. Women are advised to carefully and thoroughly remove decorative cosmetics every day, and also not to allow it to come into contact with the eyes when applying. All ophthalmological pathologies must be treated immediately.