+RU
Consultation with a Phlebologist in Moscow, Articles, Reviews of Clinics
Join us and follow the news on social networks
In order for human organs to function fully, blood circulation must be normal. Blood delivers oxygen and essential nutrients. The process must also function in the eye area, otherwise the development of diseases cannot be avoided.
Vascular eye problems worry many people. Due to inattention to oneself, many pathologies go unnoticed. To avoid complications, you should visit the hospital promptly and undergo medical examinations.
Burst capillaries in the eyes
- How our eyes work
- Common pathologies
- Common pathologies
- Characteristic symptoms
- Diagnostics
- Treatment Laser therapy
- Vitamins for eyes Complivit Oftalmo
- Vitrum Vision
- Blueberry Forte with lutein
- Star eyebright
- Biorhythm Vision
- Omega-3
Medical indications
The clinical picture is characterized by changes in the boundaries of the field of visual perception.
Inflammatory processes in the retina are open (due to the anatomical structure of the vessels). With inflammation in the focal area, infiltration of the retina and choroid begins. Scar tissue then forms, followed by the death of nerve and ganglion cells. The inflammatory process may be accompanied by vasculitis, hemorrhage, obliteration, as well as blockage or changes in the condition of blood vessels.
Classification of retinitis according to provoking factors:
- Infectious or metastatic - occurs as a result of the development or long-term course of infectious diseases.
- Systemic - manifests itself against the background of blood diseases.
- Shingles and exudative - characterized by inflammatory processes of unknown or external origin.
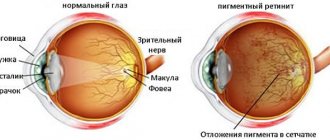
- Genetic or pigmentary - develops in the presence of renopathy (degeneration of photoreceptors) and other hereditary pathologies of the visual organs.
Classification of retinitis by location of the lesion:
- Common - determined by inflammation of the retina and choroid (choroid).
- Disseminated - affects areas surrounding the periocular nerve.
- Localized - the inflammatory process spreads through the center of the retina.
Etiology of the disease
There are a number of factors that can cause the development of retinitis:
- Infectious diseases - toxoplasmosis, leprosy, syphilis, sepsis, pneumonia, tuberculosis, erysipelas and some forms of endocarditis or meningitis. Septic forms of retinitis are provoked by staphylococci, streptococci, pneumococci and treponema pallidum.
- Viral diseases - toxoplasmosis, typhus, sarcidosis, actinomycosis and leper. Retinitis can be caused by herpes, influenza, measles and adenoviruses. Meningitis and endocarditis can be of viral or infectious origin.
- Changes in blood composition - diabetes mellitus, autoimmune diseases, leukemia and albuminuria.
- External influences - perforation of a corneal ulcer, mechanical damage, trauma, burns, exposure to ultraviolet radiation (sun rays) or ions.
The disease is not accompanied by pain. Its characteristic feature is a decrease in visual acuity. Retinitis symptoms manifest depending on the location of the inflammatory process:
- Macular region - central vision and color perception are reduced.
- The edges of the retina - light sensitivity decreases, binocular and peripheral vision decreases. With this type of retinitis, the following symptoms appear: loss of pictures or loss of visual perception in relation to certain objects. Patients often experience fog in their eyes. They have difficulty getting used to the dark.
- The spread of the inflammatory process to nearby tissues leads to the development of uvititis, optic neuritis, endophthalmitis and panophthalmitis. These pathologies are dangerous and lead to the death of the entire eye.
Against the backdrop of the appearance of chorioretinal scar tissue, vision declines rapidly. Serious symptoms include hemorrhages in the vitreous and retina. If treatment is untimely, exudative or tractional retinal detachment and death of the optic nerves occur.
Etiology
Uveitis of the eye can occur due to infection,
the onset of an allergy, due to poor metabolism, injury, severe hypothermia, or against the background of any general disease.
The most common are considered to be infectious uveitis, leading to the development of inflammation. The infection is caused by fungi, streptococci, mycobacterium tuberculosis, treponema, toxoplasma, herpes virus, etc.
Acute allergic uveitis can begin as a result of consuming any foods or medications. Background diseases are rheumatism, rheumatoid arthritis, glomerulonephritis, ulcerative colitis, psoriasis or multiple sclerosis.
Injuries include eye burns of varying severity, foreign bodies and other penetrating injuries to the eyeball.
Hormonal dysfunction can also cause uveitis, the reasons for this are menopause, menstrual irregularities, etc.
Symptoms of retinal detachment
The first symptom of retinal detachment is photopsia.
. They are sparkles, lightning, bright dots, etc. flashing in the eyes. Photopsia occur due to the fact that impulses are formed in the visual receptors, both when light rays penetrate them and during mechanical influences on the retina. Vitreoretinal fusion stretches the tissue, affecting light-sensitive cells. This provokes photopsia.
Retinal detachment is often accompanied by threads, dots and floaters slowly floating before the eyes. But such photopsies are not direct signs of pathology; they appear very often and do not require therapy. As a rule, they are provoked by destruction of the vitreous structure.
Often a Weiss ring
(round cloudiness). It indicates retinal detachment, as well as posterior detachment of the vitreous body (its hyaloid membrane) from the point of fixation to the optic nerve head.
Dark moving spots or cobwebs may appear in the patient's field of vision. These phenomena provoke bleeding in the vitreous body when the retina ruptures.
Sometimes the patient loses parts of the visual field. In this case, the eye is covered with a veil or veil. This process provokes tearing of the sensory tissue of the retina. Because of this, the patient's visual perception is upset.
The photo shows a human eye with retinal detachment.
It is worth noting that peeling occurs at a location in the shell that is opposite to the resulting effect. When the defective area of vision appears at the top, it means that the lower part of the retina has departed and vice versa. This symptom may weaken or disappear in the morning and appear with renewed vigor in the evening. This occurs due to the absorption of subretinal substance. When the process develops in areas near the middle of the eye, the described symptom will not appear.
The upper sections of the retina recede faster than the lower ones. This occurs due to the fact that the fluid accumulated in the intercellular space slowly flows down. It tears off the lower parts of the retina. This process can proceed for a long period without any manifestations. It makes itself felt only when the macular zone is affected.
The patient may also experience the following symptoms: decreased visual acuity, distorted perception of the configuration and dimensions of objects. Metamorphopsia may also be observed (straight lines are perceived as curved). The strength of this effect depends on the level of pathological changes in different parts of the retina.
These signs may occur when:
- injury to the organs of vision or head;
- getting rid of a cataract or foreign object;
- intravial injections;
- vitrectomy;
- scleral filling;
- PDT;
- laser coagulation.
Therefore, when a patient develops metamorphic photopsia, the doctor must carefully examine him to collect information and make a diagnosis.
All of the above signs of retinal detachment most often appear in the early stages of the disease. Symptoms of the secondary type of pathology are few, due to the fact that exudative separation is not tied to tissue tension.
Tractional avulsion most often occurs slowly and without any special symptoms. Photopsia and other visual impairments increase gradually or do not develop at all. Sometimes for several years. Only if the pathology begins to affect the macula will the patient begin to notice a significant drop in visual acuity.
Arterial system of the eye
The main role in the blood supply to the eye belongs to one of the most important branches of the internal carotid artery - the ophthalmic artery, which enters the orbit along the optic nerve canal, along with it.
Inside the orbit, it separates the main branches: the central retinal artery, lacrimal artery, posterior short and long ciliary arteries, supraorbital artery, muscular arteries, ethmoidal arteries (anterior and posterior), internal eyelid arteries, supratrochlear artery, nasal dorsum artery.
The role of the central retinal artery is to supply part of the optic nerve, for which a branch is separated from it - the central artery of the optic nerve. It passes inside the optic nerve and exits through the optic disc directly to the fundus. Here, it is divided into branches, forming a rather dense network of capillaries that nourish the inner layers of the retina and the intraocular segment of the optic nerve.
Occasionally, an additional blood vessel may be found in the fundus that takes part in feeding the macular area - this is the cilioretinal artery, originating in the posterior short ciliary artery. When the blood flow of the central retinal artery is disrupted, the cilioretinal artery has the task of providing nutrition to the macular zone, which will prevent a decrease in central vision.
The ophthalmic artery branches into 6-12 posterior short ciliary arteries, which branch off into the sclera, bending around the optic nerve, forming an arterial circle that provides blood supply to the segment of the optic nerve after it leaves the eye. At the same time, they provide blood flow directly to the choroid of the eye. These arteries do not approach the ciliary body and the iris, which makes the inflammatory processes of the anterior and posterior segments of the eye relatively isolated.
The ophthalmic artery also gives rise to two posterior long ciliary arteries, which pass the sclera on both sides of the optic nerve and then pass through the perivascular space to reach the ciliary body. In the ciliary body, the posterior long ciliary arteries and the anterior ciliary arteries - branches of the muscular arteries - unite, as well as, partially, the posterior short ciliary arteries, to form the large arterial circle of the iris. It is located in the root zone of the iris, the branches extending from it are directed to the pupil. In the border zone of the pupillary girdle and the ciliary girdle of the iris, these branches create the small arterial circle. The iris and ciliary body receive blood supply through their branches and the small arterial circle.
Muscular arteries provide blood supply to all the muscles of the eye, and the arteries of the rectus muscles branch into branches of the anterior ciliary arteries, which also divide, forming vascular networks in the limbus, connected to the highways of the posterior long ciliary arteries.
The internal arteries of the eyelids are located in the thickness of the skin, then come out to the surface of the eyelids and connect with the external arteries - branches of the lacrimal artery. As a result of this fusion, the lower and upper arterial arches of the eyelids are formed, through which their blood supply occurs.
Several branches of the arteries of the eyelids extend to the posterior surface, providing blood supply to the conjunctiva - these are the posterior conjunctival arteries. Near the fornix of the conjunctiva, there is a connection between them and the anterior conjunctival arteries - branches of the anterior ciliary arteries that supply the conjunctiva of the organ of vision.
The lacrimal gland receives nutrition from the lacrimal artery, which also provides blood flow to the external and superior rectus muscles, as it passes nearby. Next, it participates in the blood supply to the eyelids. Leaving the orbit through the supraorbital notch in the frontal bone, the supraorbital artery supplies the area of the upper eyelid simultaneously with the supratrochlear artery.
The ethmoidal arteries (anterior and posterior) take part in the blood supply to the nasal mucosa, as well as the ethmoidal labyrinth.
Other highways also provide blood circulation to the eye: the infraorbital artery is a branch of the maxillary artery, which is involved in supplying nutrition to the lower eyelid, the rectus and oblique muscles, the lacrimal gland with the lacrimal sac, and the facial artery, which separates the angular artery to supply the inner area of the eyelids.
Retinal diseases
The inner layer of the eye containing photoreceptors is called the retina. Function: converting incoming rays into nerve impulses. The following eye diseases of the retina in adults are distinguished:
Retinitis
Retinitis is an inflammatory process of the retina. The causes can be infectious (bacterial, viral retinitis) and non-infectious. Non-infectious ones are provoked by traumatic injuries, radioactive damage, sunlight, and allergic causes. The vision narrows, there is double vision, vision in the dark is disrupted, and flashes appear before the eyes. Retinal hemorrhage is possible.
Therapy: a combination of local and parenteral antibacterial or antiviral drugs, corticosteroids. For hemorrhage in the retina (the so-called “bloody eye”) - vitrectomy.
Retinopathy
Retinopathy is a disease when a macular fold appears in the vitreous body. Causes: diabetes mellitus (see diabetic retinopathy), hypermetropia, trauma, retinal detachment. In this case, a person experiences double vision and vision loses clarity.
For retinopathy, drops are prescribed that improve metabolic processes. If the cause is diabetes mellitus, then adjustment of the treatment regimen is necessary to normalize blood glucose levels. Laser coagulation is effective.
Glaucoma
Glaucoma is congenital or acquired increased intraocular pressure. Causes: chronic diseases of internal organs, severe myopia, hypertension. Symptoms are double vision, flashes and flickering sparks, limited vision in the periphery, headache, eye pain, blindness. Highlight:
- Open-angle glaucoma - an obstruction to the outflow of aqueous humor forms in the deep layers of the eye. The disease develops slowly.
- Angle-closure glaucoma - the outflow is blocked suddenly, leading to an acute attack. Emergency assistance required.
The basis of therapy is to reduce IOP. It is achieved by prescribing blood pressure drops and treating the underlying disease.
Retinal dystrophy
Hereditary or acquired progressive fundus disease. When the central zone (macula) is damaged, macular degeneration of the retina develops. This is an age-related degenerative disease. Caused by vascular damage due to hypertension, diabetes, injuries to the visual organ, as well as myopia.
Symptoms of the disease are a blind spot in the center, distortion of vision, flickering of flies. In the fundus, the doctor will see the characteristic bull's eye symptom - a dark spot surrounded by a light rim.
Therapy in the early stages - drops with vitamins and antioxidants, corticosteroid drops. To strengthen muscles - physiotherapy (electrophoresis, phonophoresis, ultrasound). In later stages - reconstructive surgery on the retina.
Retinal disinsertion
Injuries and severe somatic illnesses can provoke detachment of the retina from the choroid. Symptoms are a veil, flickering spots before the eyes, limited visual fields on the sides, incorrect perception of the shapes of objects. The condition threatens complete blindness.
Treated using laser soldering or surgery.
Common pathologies
Among the numerous problems, diseases of the vascular tract of the eye account for approximately 5%.
The most common pathologies are the following:
| Pathology | Characteristic |
| The pathology is characterized by the absence of the iris. The pupil is dilated to its maximum, only blackness is present. |
| An eye defect can be acquired or congenital. The pupil takes the shape of a pear, and fundus defects may appear. |
| There may be two or more pupils, one is large, the others are smaller. Visual acuity decreases. |
| The location of the pupil is eccentric, vision decreases, and strabismus may develop. |
| The form of the anomaly is harmless and is often found in children. Dense membranes in the center of the lens affect visual acuity. |
Diseases of the eye vessels are dangerous and require immediate intervention from medical personnel.
Traumatic lesions
Retinal detachment can be classified in this group quite conditionally, because the separation of this layer from the choroid of the eye can occur both as a result of trauma (rupture) and other diseases - diabetic retinopathy, tumors, edema of any origin.
Prevention of retinal detachment when it ruptures
Detachment can be partial or complete. Symptoms, as a rule, are pronounced - a veil before the eyes, a significant deterioration in vision, the appearance of light sparks, distortion of the shapes of objects. They occur on the side corresponding to the localization of the detachment.
The main method of treatment is surgery.
Structure and functions of the retina
The retina is a highly differentiated nervous tissue that is located on the inner part of the back of the eyeball. The retina helps to correctly perceive the image that is projected onto it due to the corneal layer and the lens. Next, the image is converted into nerve impulses, which subsequently enter the cerebral cortex.
The retina is in closest contact with the eyeball along the edge of the optic nerve. The thickness of the retina varies in different areas. The retina has a rather complex structure, thanks to which it is the first to perceive light and converts light energy into a signal that contains information about everything that a person sees.
The important part is the macula, or macula. It is responsible for the quality of central vision
The macula contains many photoreceptors that allow a person to see well during the day.
Surgery
Surgery is required if the disease occurs with serious complications. As a rule, the operation involves certain stages:
- the surgeon cuts the adhesions that connect the membrane and the lens;
- removes vitreous humor, glaucoma or cataracts;
- removes the eyeball;
- using laser equipment, attaches the retina.
Every patient should know that surgery does not always result in a positive result. The specialist warns him about this. After surgery, there is a risk of exacerbation of the inflammatory process. Therefore, it is important to promptly identify the disease, diagnose it, and prescribe effective therapy.
PreviousTularemiaNextNodular goiter
Glaucoma
Treatment - specific tips and recommendations
The choice of treatment strategy for atherosclerotic lesions will depend on the results of the study, the presence of accompanying diseases and complications.
Therapeutic relief of the pathological condition is carried out by ophthalmologists, who, after a detailed study of each individual clinical case, decide on the choice of medications and treatment procedures or the urgency of surgical intervention.
Drugs used in the initial stages
- Angioprotectors that protect the weakened and lost elasticity of the vessel wall from ruptures.
- Vasodilators that prevent spasms and improve blood circulation in damaged areas.
- Anti-sclerotic complexes for the direct elimination of fatty plaques.
- Antiplatelet agents that help improve the rheological properties of blood and prevent the formation of blood clots.
To obtain the maximum effect from the drugs, patients are recommended dosage forms in the form of eye drops, as they go directly to the site of damage, providing an accelerated therapeutic effect. If there are diseases occurring simultaneously with this one, they are also treated to eliminate the chance of complications.
Important! Do not try to start treatment on your own. Incompatibility of drugs can lead not only to complete loss of vision, but also to the death of the patient
Surgical treatment is used for patients in whom atherosclerosis has caused the development of a critical complication of retinal detachment. Among the most popular surgical interventions today are:
- laser coagulation of the retina;
- scleral ballooning;
- vitrectomy or removal of the vitreous.
Find out here whether treatment with folk remedies (herbs) is effective; what drugs are used for vascular atherosclerosis, read here.
Used in practice
- Mildronate, a stimulator of central and local circulation. Price – 250 rub.
- Vazonit, Peripheral vasodilator. Cost 340 rub.
- Solcoseryl, ointment for disinfection. Price 350 rub.
- Arbiflex, anti-inflammatory drug. Cost 480 rub.
Laser therapy
A modern painless procedure that involves destroying deposits using a laser beam of variable wavelength.
The entire procedure takes no more than 20 minutes and has no contraindications. Because the procedure is expensive, it is optional and serves as an alternative to traditional surgery. After the procedure, the patient must also undergo consultations and be observed by an ophthalmologist for 2 months to monitor health and eliminate possible complications.
Consequences and complications
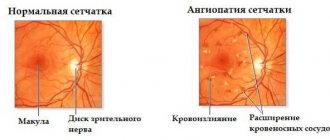
Increased blood pressure primarily damages the walls of blood vessels throughout the body. Examination of the fundus is one of the mandatory procedures when diagnosing hypertension and its consequences. With hypertensive angiopathy, arterial vasospasms, dilatation and inversion of the retinal veins are observed.
The thickness of the arteries, in relation to the size of the veins, decreases. The veins in the area of intersection with the arteries bend and move into the retina. Sometimes there is a loss of veins at the intersection with the arteries, swelling of the retina occurs, and hemorrhages may develop.
Hypertensive angiosclerosis
Since the causes are systemic in nature, angiosclerosis of both eyes is observed. In the early stages, there are no obvious external symptoms. As retinal damage progresses, double vision, blurred vision, or loss of vision may occur. Diagnosis of hypertensive angiosclerosis of the retina is carried out using fundus ophthalmoscopy and fluorescein angiography.
Reference! Treatment is based on therapeutic methods that involve preventing pathology.
Functions
The main function of the retina is photoreception - a chain of biochemical reactions during which light stimuli are converted into nerve impulses. This occurs due to the breakdown of rhodopsin and iodopsin - visual pigments formed when there is a sufficient amount of vitamin A in the body.
The retina of the eye provides:
- Central vision. Allows a person to read, do close-up work, and clearly see objects located at different distances. The cones of the retina, which are located in the area of the macula, are responsible for it.
- Peripheral vision. Necessary for orientation in space. It is provided by rods, which are localized paracentrally and on the periphery of the retina.
- Color vision. Makes it possible to distinguish colors and their shades. It is responsible for three different types of cones, each of which perceives light waves of a certain length. This enables a person to distinguish between green, red and blue colors. Impaired color vision is called color blindness. Some people experience a phenomenon called a fourth, additional cone. It is typical for 2% of women who can distinguish up to 100 million colors.
- Night vision. Provides the ability to see in low light conditions. It is carried out thanks to rods, since cones do not function in the dark.
Common pathologies
Damaged blood vessels in the eyes can lead to the development of many unpleasant and dangerous consequences.
There are the following vascular diseases of the organ of vision:
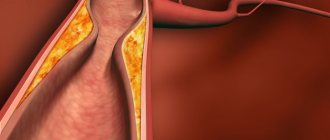
- Thrombosis - forms in the central optic artery or in the branches extending from it. As a result of cholesterol deposits on the walls of the arteries, they become clogged. High blood coagulation can contribute to its development.
- Ischemic neuropathy occurs due to impaired blood circulation, as well as when the innervation of the arteries of the fundus is impaired.
- Chorioretinitis is an inflammatory process that affects the vascular branches of the eye.
- An aneurysm is another pathology of the arteries of the fundus, during which their lumen is limited and the walls protrude. If blood coagulation is low, severe bleeding occurs.
The photo below is an example of some diseases
Development of chorioretinitis
Who is at risk
A dangerous disease can appear as a result of bad habits (excessive alcohol consumption). Also, people employed in hazardous work automatically fall into the risk group. If the environmental situation is bad, this negatively affects the condition of the retina. Most often, angiopathy is diagnosed in elderly patients.
People most susceptible to developing the anomaly:
Women in position
In this case, it is important to identify the disease at an early stage. If the disease progresses, it can cause retinal detachment
Angiopathy rarely manifests itself in the early stages; it usually makes itself felt in the second and third trimester. Most often, pregnant women are not prescribed treatment, since the pathology goes away after the birth of the child. But if the expectant mother suffers greatly from gestosis, the doctor will select the necessary medications; Newborn babies. If the birth was difficult or the baby was injured during the birth process, then proliferative changes occur in the vascular system. As a result, the gaps in the capillaries narrow, and blood circulation proceeds slowly; Children in adolescence. It is still unknown what is the reason for the appearance of pathology in this category of patients. Boys are usually diagnosed with juvenile angiopathy, accompanied by minor hemorrhages. Cataracts and glaucoma often appear. In severe cases, vision loss occurs.
Diagnostics
In order to identify how the pathology has affected the blood vessels of the eyes and correctly prescribe treatment, the patient must undergo a full examination.
Diagnostic measures used for this may be the following:
- Ophthalmoscopy - examines the fundus of the eye, the membrane of blood vessels, and the retina. An ophthalmoscope is used to carry out the procedure. The beam of light is directed to the right place, and the doctor can see everything he needs. There are several methods for performing ophthalmoscopy, each of them involves the use of different mirrors.
- Fluorescein angiography. A contrast liquid is injected into the vascular system, and the specialist analyzes the condition of large and small vessels, the retina and the fundus of the eye. The method is often used to identify the choroid.
- Doppler - ultrasound diagnostics, allows you to evaluate the nature of blood flow in the vessels, speed, coagulation, etc. During the study, ischemic changes can be detected.
- Rheography - unlike the method listed above, you can calculate the amount of blood that enters the eyeball over a certain period of time.
As a result of the research methods carried out, a diagnosis can be made and treatment can be prescribed. This is important, since many pathologies can lead to irreversible consequences.
Treatment of retinal detachment
Retinal detachment is considered a dangerous disease of the retina.
It is important to remember that with such a diagnosis, the patient can only be cured with the help of surgery, and no medicines or folk remedies can eliminate such a disease
Any self-medication will only lead to the loss of precious time, because detachment is considered fresh only in the first few months after its appearance. If pathology is detected at such a time, the chances that vision will be fully restored after treatment increase.
In a situation where it is possible to diagnose an old retinal detachment, surgical intervention is much more difficult for both the doctor and the patient.
Long-term retinal detachment results in the death of a large number of light-sensitive cells and this creates certain difficulties in restoring vision.
Drug treatment is used as an adjunct to surgical treatment. For eye injuries, fibrinolysis inhibitors are used to stop intraocular bleeding. Drugs to improve cellular nutrition and vitamin complexes are also prescribed.
Delaying or ignoring the symptoms of the disease can lead to complications: atrophy of the eyeball, persistent decrease in pressure, secondary cataracts and blindness. During the operation, the attending physician reduces the distance between the light-sensitive cells and the pigment epithelium.
Adhesions are created in the area of the rupture. This allows you to normalize vision. The cost of treatment depends on the type of surgery. The most commonly performed eye surgeries are:
- laser therapy;
- scleroplasty;
- extrascleral filling;
- ballooning;
- vitrectomy;
- vitreoretinal intervention;
- cryocoagulation.
Laser coagulation of the retina also refers to surgical methods, but has its own characteristics. This is an outpatient operation that does not require a long rehabilitation period.
It is carried out in the ophthalmology office of the clinic. It is used independently for small detachments, and in addition to operations for better fusion of the retina with the underlying layers.
Treatment of this retinal disease is carried out using the following groups of operations:
- extrascleral interventions are performed on the surface of the sclera;
- endovitreal interventions are performed inside the eyeball.
Even after a successful operation, a person needs to visit an ophthalmologist twice a year and undergo a thorough examination of all blocked retinal tears.
In addition, such patients are advised to undergo courses of conservative therapy, which combines the use of retinoprotective, metabolic and vitamin tissue preparations.
After eye surgery, the patient will have to avoid any physical activity on the body and heavy lifting. The prognosis of developed retinal detachment will depend on the duration of the disease and the timeliness of treatment.
When retinal disease is diagnosed at the very beginning of its development during surgery, the outcome is usually favorable. It is possible to prevent the disease in people by following preventive measures and timely contacting a specialist when the first signs of retinal detachment appear.
The size of the detachment increases over time, leading to further deterioration of vision. Therefore, if symptoms appear, it is better to immediately consult a specialist. If the detachment has already occurred, only surgical treatment is possible.
And the faster it is carried out, the greater the chance of preserving the viability of the retinal cells, and therefore its functionality.
Treatment
In order to treat diseases affecting the eye vessels, the following medications and methods may be prescribed:
- Eye drops, for example, Albucid, Floxal. The effect is local, drops are used to treat the retina and membrane. It is possible to relieve inflammatory processes and stop the further spread of infection.
- Eye ointment – Acyclovir, Tetracycline. The drug is applied behind the lower eyelid or on its surface. Just like drops, it has a local effect; symptoms can be relieved in a few days.
- Tablets – medications in the form of tablets can be used to treat vascular diseases. The composition of the blood improves, coagulation decreases, and the formation of blood clots is prevented.
- Treatment by surgery. An operation is performed only if neither drops nor medications give the desired effect. The procedure is performed by a specialist in ophthalmic-oncology clinics.
Since many vascular diseases occur deep at the bottom of the eyeball, treatment becomes difficult. Drugs with local action are ineffective, so it is recommended to combine them with other methods.
Laser therapy
A new and effective treatment method. Suitable for vascular deformation and disruption. Patients are given local anesthesia using drops; the procedure lasts no more than half an hour. The patient does not experience pain and does not require further follow-up with a specialist.
The laser beam acts directly on defective areas of blood vessels. Can be used for prevention.
Surgery is performed to treat the following diseases:
- age-related changes in the retina;
- angiomatosis;
- retinal dystrophy;
- hypertensive retinopathy;
- retinal tear.
Laser coagulation can be carried out after surgery, so the results can be consolidated.
If the patient has serious pathologies, such as diabetes, there may be a relapse after laser coagulation. Overall, this is an effective and simple method of therapy. The percentage of complications is low, the rehabilitation period is fast.
Laser beam directed at the pupil
Vitamins for eyes
Modern lifestyle makes the eyes vulnerable to the development of many pathologies. There are many provoking factors: working at a computer, poor lighting, stress, etc. In order to maintain the health of the visual organs, it is recommended to drink vitamin complexes several times a year (see Vitamins for strengthening the blood vessels of the eyes - who needs them?).
Complivit Oftalmo
The main advantage of vitamins is that they have a positive effect on all eye functions. Contains many vitamins and minerals. The deficiency of nutrients is replenished, the walls of blood vessels are strengthened, and regeneration processes are accelerated.
Vitrum Vision
Contains everything you need for your visual organs. The eyes are supplied with everything they need, visual acuity increases, and blood circulation improves. The development of many diseases can be prevented. It is not recommended to take it together with other multivitamins; if necessary, you should consult your doctor.
Blueberry Forte with lutein
Everyone knows about the beneficial properties of blueberries. It contains all the substances that activate recovery processes. The permeability of cell membranes is restored, and the walls of blood vessels are strengthened.
Among the shortcomings, one can highlight only intolerance to the components included in the composition.
Star eyebright
The vitamin complex is designed for connoisseurs of the power of nature. The plant has a positive effect on tissue regeneration and is suitable for people who spend a lot of time at the computer. Blood circulation improves and blood vessels are strengthened.
Biorhythm Vision
The organs of vision are constantly under tension during the day, so they must fully rest at night. When under load, an additional complex of beneficial substances for the eyes is required. Vitamins maintain visual acuity, strengthen the walls of blood vessels, and prevent the development of many diseases.
Omega-3
Many people mistakenly believe that the drug is only suitable for the heart, but this opinion is erroneous. The eyes need support not only under heavy loads, but also with age. With the help of Omega-3, atherosclerotic processes can be prevented, and all conditions for cleansing will be created. Instructions for use are included in the package.
Proper nutrition
To maintain health, it is necessary to maintain proper nutrition.
The following products should be present in the diet:
- Carrot juice - the eyes will be saturated with vitamin A, twilight vision will improve. In order for it to be better absorbed by the body, it is necessary to mix it with milk in a 1:1 ratio. The cocktail must be drunk every day for one month.
- Parsley – removes toxins, relieves inflammation from the optic nerve. In winter, dried herbs can be used to maintain eye health.
- Blueberry. It is useful in any form, both frozen and fresh. Preparations with blueberries are not as effective as the natural product.
- Apricot – contains potassium, which is good for the eyes.
The price of such products is low, and many people grow them in their gardens.
Types of angiopathy
Retinal angiopathy occurs as a result of pathological conditions of the body, accompanied by deterioration of blood supply to the fundus of the eye. Such changes in the capillaries of the visual apparatus can appear at any age, but are most often diagnosed in older people. Depending on the nature of the origin, the following types of retinal angiopathy are distinguished:
- Hypertensive. Elevated blood pressure is one of the most common causes of hypertensive angioneuropathy. Arterial hypertension leads to damage to the central artery, narrowing of blood vessels, dilation of veins and damage to retinal tissue. As a result of this, the venous bed branches, pinpoint hemorrhages occur, and the risk of rupture and the development of atherosclerosis increases. With timely treatment of hypertension, the structure of the eye returns to normal.
- Hypotonic. Low blood pressure provokes a slowdown in blood flow and a decrease in the tone of small capillaries, as a result of which the blood thickens and the risk of thrombosis increases. During the diagnostic process, expansion of the arterial network and pulsation of the veins are observed.
- Diabetic. In diabetes mellitus, blood vessels are damaged throughout the body, as a result of which blood circulation is impaired, blood vessels become clogged, the capillary wall swells and vision deteriorates. Due to high levels of glucose in the blood, blood clots form, tissue atrophy begins, and multiple hemorrhages are observed.
Diabetic retinal angiopathy develops in several stages:
- Non-proliferative. Gradual damage to the vessels of the fundus is observed, microscopic aneurysms are formed, and minor hemorrhages develop. This stage is accompanied by swelling of the retina and redness of the iris.
- Preproliferative. Damage occurs to the retinal veins, which become tortuous and dilated. When blood vessels rupture, hemorrhages are observed and venous infiltrates are formed, causing a significant deterioration in vision.
- Proliferative. The most severe degree of diabetic angiopathy, in which new capillaries are formed, characterized by increased fragility. This leads to the appearance of a large number of hemorrhages, causing retinal detachment.
- Traumatic. Due to injuries to the head, neck or eyes, blood vessels are compressed and intracranial pressure increases significantly, which can lead to the formation of leukocyte emboli.
- Youthful. A rare and dangerous form of retinal angiopathy, the nature of which is not precisely known. The pathology develops up to 30 years of age. Juvenile vascular angiodystonia manifests itself through inflammatory processes, hemorrhages and proliferation of connective tissue, which ultimately leads to various complications.
- Congenital. Develops in premature babies due to underdevelopment of the vascular system.
Determining the type of retinal angiopathy is an important point in making a diagnosis, on which the specifics of treatment depend.
Treatment of retinal angiopathy is best started at the initial stage, when changes are minimal. Lack of treatment threatens the development of blindness.
Prevention
It is easier to prevent the development of diseases than to fight them later. Moreover, treating vascular eye pathologies is difficult and time consuming.
In order to prevent their development, you must follow simple rules:
- Control your blood cholesterol levels. It settles on the walls of blood vessels, plaques form, which in turn lead to thrombosis. To prevent this from happening, its level should be controlled. For this purpose tests are taken.
- Take vitamin complexes several times a year. With their help, the arteries are maintained in good shape and do not become thinner. Blood composition improves.
- Follow a regime when you have eye strain. Spending time at the computer, TV, or book should alternate with rest. You need to take a break every hour. Spend this time doing eye exercises.
Healthy Eye Products
It is not difficult to maintain the eye vessels and prevent the development of diseases associated with them (see How to strengthen the eye vessels quickly and effectively). If the pathologies described above have been identified, it is necessary to consult a doctor and undergo an examination. Without treatment, they can lead to complete blindness; they need to be treated promptly.
Retinal dystrophy - symptoms and signs
symptoms
- Decreased visual acuity in one or both eyes (the need for bright light for reading or writing is also a sign of decreased visual acuity);
- Narrowing of the field of view;
- The appearance of scotoma (spot or sensation of a curtain, fog or obstruction in front of the eyes);
- A distorted, wave-like image before the eyes, as if a person is looking through a layer of water;
- Poor vision in darkness or twilight (nyctalopia);
- Impaired color discrimination (colors are perceived as different, not corresponding to reality, for example, blue is seen as green, etc.);
- Periodic appearance of “floaters” or flashes before the eyes;
- Metamorphopsia (incorrect perception of everything related to the shape, color and location in space of a real object);
- Inability to correctly distinguish a moving object from a stationary one.
ophthalmologist In addition to the listed clinical symptoms, retinal dystrophy is characterized by the following signs identified during objective examinations and various tests: 1. Amsler test 2. 3.
electroretinography
Symptoms
The clinical picture of different uveitis is somewhat different. Symptoms of inflammation of the anterior region:
- redness of the eyes;
- lacrimation;
- increased sensitivity to light;
- loss of vision;
- painful sensations;
- narrowing of the pupil;
- rise in intraocular pressure.
The acute course of the disease causes severe symptoms, forcing the patient to consult a doctor as soon as possible.
With chronic inflammation, the severity of the manifestations is weak or unnoticeable: some redness of the eye, a feeling of red dots in front of the eyes.
Peripheral uveitis manifests itself:
- feeling of flies flashing before the eyes;
- bilateral eye damage;
- decreased visual acuity.
Inflammation in the posterior region is disturbing due to distorted perception of objects. The patient complains that he sees “through the fog,” spots appear before his eyes, and visual acuity decreases.
Methods for diagnosing eye diseases
After an examination and medical history, the patient will need to have a blood test to confirm or refute the presence of inflammation. A number of specific procedures are also prescribed:
- Ophthalmoscopy. Allows the doctor to examine the fundus in detail. This is done using special tools. It is considered the most informative type of diagnosis.
- Visometry. Using special tables, the doctor will determine visual acuity and, if necessary, select corrective eyepieces.
- Refractometry. The technique is used to determine the optical power of the organ of vision. Helps detect astigmatism and hypermetropia.
- Perimetry. Peripheral view analysis.
- Using Rabkin's tables, the patient's color perception is checked.
- Biomicroscopy. A microscope equipped with a powerful lens allows you to examine the smallest deviations in the structure of the cornea, iris, and lens.
- Strabismus. The technique is used to determine the angle of strabismus.
- Ultrasound examination of the eyeball.
- Probing the lacrimal canal.
- Ophthalmometry. Measuring the radius of refraction of the cornea.
- Examination of eyelashes to identify mites.
| After the age of forty, it is recommended to undergo tonometry every year to detect glaucoma at an early stage. Using special equipment, the doctor measures intraocular pressure. |