The lacrimal glands are located in pairs on each eye, on the upper and lower eyelids. The upper gland is called the greater orbital, the lower is called the lesser palpebral. The orbital lacrimal gland is located in a recess formed by the frontal bone and is hidden under the supraorbital margin. The palpebral gland is located in the upper outer fornix and is accessible for inspection.
Composition of tears
The composition of tear fluid includes: water (up to 98%), electrolytes or inorganic salts (up to 2%), a small amount of proteins, lipids, mucopolysaccharides and other organic components.
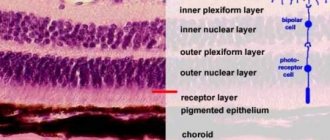
Normally, a tear has the appearance of a layered film covering the anterior surface of the cornea, which ensures the transparency and ideal smoothness of the latter. This precorneal tear film consists of: a superficial lipid layer in contact with the atmosphere, an aqueous layer with mucin, and a mucoid layer in contact with the corneal epithelium. The composition of the surface lipid layer includes the secretion of the meibomian glands, which protects the underlying aqueous layer from evaporation. The aqueous layer is synthesized from the secretion of the lacrimal glands. The mucoid layer takes on the function of a connector between the corneal epithelium and the aqueous layer of tear fluid.
Functions of tears
Tears have an important protective function. It continuously moisturizes the surfaces of the conjunctiva and cornea, improving the optical properties of the latter.
In addition, tears improve the trophism of the cornea, since the salts, proteins and lipids dissolved in it nourish the cornea. The composition of tears also contains a specific antibacterial substance (lysozyme), which provides its bactericidal properties. Tear also performs a protective function mechanically, removing small foreign substances from the surface of the eye. Normally, the accessory lacrimal glands secrete up to a milliliter of tear fluid every day, which is quite enough for the film to be evenly distributed over the entire surface, well moisturizing the eyeball. Foreign substances entering the eye, excessive irritation from light, wind or temperature, as well as certain emotional states cause the main large lacrimal gland to work.
Literature
- Diseases of the lacrimal organs: Monograph / Cherkunov B.F. - Samara: State Enterprise "Perspective", 2001. - 296 p. — ISBN 5-900031-43-8.
- Lacrimal glands // Small encyclopedic dictionary of Brockhaus and Efron: in 4 volumes - St. Petersburg, 1907-1909.
- Lacrimal glands // Great Soviet Encyclopedia: [in 30 volumes] / ch. ed. A. M. Prokhorov. — 3rd ed. - M.: Soviet Encyclopedia, 1969-1978.
- Beloglazov V. G.
Lacrimal organs // Great Medical Encyclopedia, 3rd ed. - M.: Soviet Encyclopedia. - T. 23. - Volokonenko A.I.
Conjunctiva // Great Medical Encyclopedia, 3rd ed. - M.: Soviet Encyclopedia. - T. 11.
Lacrimal glands
The lacrimal secretory organs include: the lacrimal gland, as well as small accessory lacrimal glands located in the fornix of the conjunctiva. The location of the lacrimal gland is under the upper eyelid, in its upper outer section. The gland is usually divided into the orbital upper and palpebral lower parts. The tendon of the muscle that lifts the upper eyelid separates these two parts from each other. The orbital part of the lacrimal gland is located in the bony fossa of the superior outer wall of the orbit. A total of about a dozen excretory ducts of the main lacrimal glands open into the upper fornix of the conjunctiva.
The lacrimal gland is supplied with blood by the lacrimal artery, a branch of the ophthalmic artery. Blood flows out through the lacrimal vein.
The production of tear fluid is regulated by parasympathetic nerve fibers of the facial nerve. At the same time, the lacrimal gland is innervated by sympathetic fibers of the superior cervical sympathetic ganglion and branches of the trigeminal nerve.
The accessory glands involved in the formation of tears are usually classified into 3 groups of glands:
- With a fatty secretion, which includes the meibomian glands, localized in the cartilaginous plate and the Zeiss glands, located in the follicles of the eyelashes.
- With water secretion. These are the Krause glands and Wolfring glands located in the conjunctival cartilage, some of which are located along the edge of the cartilaginous plate; as well as Moll's glands in the hair follicles of the eyelashes.
- With mucous secretion, including goblet cells, as well as granule-containing glands in the conjunctiva and cartilage; The crypts of Henle, in the folds of the conjunctiva and the glands of Manz located in the limbal conjunctiva.
Notes
- ↑ 1 2 3 4 5 6 Brzhesky V.V., Somov E.E.
Corneal-conjunctival xerosis (diagnosis, clinic, treatment) / 2nd ed., revised. and additional // St. Petersburg: Lefty. Saint Petersburg. - 2003. - 120 p. ISBN 5-93356-027-8. (P. 5-12). - Clinically Oriented Anatomy, Dalley & Agur.
- ↑ 1 2 Dogel A. S.
Lacrimal glands // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907. - ↑ 1 2 3 4 5 Avetisov S. E., Egorov E. A., Moshetova L. K., Neroev V. V., Takhchidi H. P.
Ophthalmology: national guide // M.: GEOTAR-Media. - 2008. - 944 p., ill. ISBN 978-5-9704-0707-3. (pp. 72-83, 362-399). - Tarkhanov I.R.
Tears // Encyclopedic Dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). - St. Petersburg, 1890-1907. - “eye, human.”Encyclopædia Britannica. 2010. Encyclopædia Britannica 2010 Ultimate Reference Suite DVD 2010
- Sapin M. R., Bocharov V. Ya., Nikityuk D. B., Satyukova G. S., Selin Yu. M., Spirin B. A.
Human anatomy / In 2 vols. T. 2, 5th ed. . reworked and additional // M.: Medicine. - 2001. - 640 p., ill. ISBN 5-225-04586-3. (pp. 583-589). - Illustrated Anatomy of the Head and Neck, Fehrenbach and Herring, Elsevier, 2012, page 153.
Lacrimal organs
The outflow of tear fluid involves a complex system of anatomical formations.
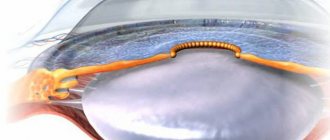
The narrow strip connecting the back surface of the edge of the eyelid and the eyeball is called the lacrimal duct. Then the tear fluid accumulates as a tear lake near the inner corner of the eye, near the lacrimal openings, which are easily distinguishable - upper and lower, on the corresponding eyelids. These points open the entrance to the lacrimal canaliculi, which carry tears, often uniting, to the lacrimal sac, which passes into the nasolacrimal canal. The canal itself opens with a hole already inside the sinuses.
Therefore, when some medications are introduced into the eye, you can sometimes feel their taste, since with the flow of tears the medicine enters the nose and then into the mouth.
Initially, the lacrimal canaliculi have a vertical course of approximately 2 mm, then continuing horizontally (8 mm). The main amount of tears - 70% - flows through the lower lacrimal canaliculus.
The lacrimal canaliculi open in one common way into the lacrimal sac, where at the entrance site there is a mucous fold, the so-called. Rosenmüller valve, which creates an obstacle to the reverse flow (reflux) of tear fluid from the bag. The sac itself, 5-10 mm in size, is located inside the bony lacrimal fossa outside the orbital cavity between the anterior and posterior lacrimal ridges. The outflow of tear fluid from the lake occurs according to the pump principle: when blinking, due to the pressure gradient created by the orbicular muscle and the fascia of the lacrimal sac, the tear flows through the lacrimal canaliculi into the lacrimal sac, and then into the nasolacrimal duct. The nasolacrimal duct opens into the lower nasal passage, partially covered by a mucous fold - the valve of Hasner. Blockage of the nasolacrimal duct can lead to stretching of the lacrimal sac, followed by inflammation.
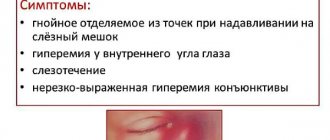
Symptoms of the lesion
A feeling of dryness, burning in the eye, sensation of a foreign body or “sand” may indicate hypofunction of the lacrimal gland, in which an insufficient amount of tear fluid is produced. Lacrimation, on the contrary, indicates a violation of the outflow of tears. Moreover, an obstacle to the outflow of tears can be located at any level: from the patency of the lacrimal openings to the condition of the nasolacrimal canal.
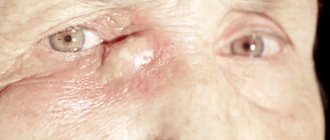
Especially often, due to a chronic delay in the outflow of tear fluid, the lacrimal sac suffers, with the appearance of redness and swelling of the inner edge of the eye. The lacrimal gland often becomes inflamed due to specific lesions of the glandular organs.
Pathology
Due to disruption of the tear glands, dry, itchy and burning eyes may occur, which are signs of dry eye syndrome or Sicca keratoconjunctivitis. In this syndrome, the tear glands produce less tear fluid. This is mainly due to the aging process or taking certain medications. To determine total tear production
You can use the Schirmer test (Schirmer-I test),
the main tear production
is the Jones test (Schirmer-II test, the following can also be used:
test thread test
,
lactoferrin test
,
test with sodium fluorescein dilution
,
assessment of the height of the tear meniscus
). Many medications or diseases that cause dry eye syndrome can also cause insufficient salivation and dry mouth. Treatment varies depending on the etiology and includes avoiding irritants, stimulating lacrimation, increasing tear production, clearing the eyelids, and treating ocular inflammation[8].
In addition, there are other pathologies of the lacrimal gland [4]:
- developmental anomalies - absence or underdevelopment of the main lacrimal gland
- lacrimal gland injuries
- lacrimal gland tumors
- dacryoadenitis - inflammation of the lacrimal gland due to bacterial and viral infections, with autoimmune diseases also affecting the salivary glands, such as Sjögren's, Schauman's, Mikulicz's diseases
- dacryops - a cyst of the lacrimal glands, both main and accessory (in the latter it is associated with trachoma)
- displacement of the lacrimal gland (congenital or acquired)
Diagnostics
The position and condition of the eyelids are examined during an external examination. The area of the lacrimal sac is palpated, which may be painful due to its inflammation. Eversion of the upper eyelid allows for external examination of the palpebral portion of the lacrimal gland with a slit lamp. With further biomicroscopy of the eye, the condition of the lacrimal openings and the degree of hydration of the conjunctiva with the cornea are assessed. A test with a specific dye (rose Bengal) makes it possible to identify epithelial cells that are not viable due to insufficient function of the lacrimal glands.
Assessment of the patency of the lacrimal canals is carried out by washing the lacrimal ducts; normally, sterile water injected into the lacrimal opening enters the nose and then into the mouth. A fluorescein test also helps to assess the patency of the lacrimal drainage system. Normally, a special fluorescein dye introduced into the conjunctival sac should appear in the nasal cavity after a few seconds.
Suspicion of obstruction of the lacrimal ducts requires an x-ray examination with a contrast agent (contrast dacryocystography), which will reliably show the level and degree of obstruction of organs in the lacrimal outflow system.
To assess the rate of tear fluid production, a test with litmus strips (Schirmer test) is prescribed, which is placed behind the lower eyelid. The rate of wetting of the strips with tears determines the functions of the lacrimal gland. If the rate of wetting of the strips is below 1 mm/minute, a violation of the secretion of the lacrimal glands is impaired.
Deterioration in the production of tear fluid is often caused by certain medications.
Physiology and functions
The tear secreted by the main lacrimal gland enters the conjunctival sacs through the ducts and, mixing with the secretions of other glands of the conjunctiva and eyelids, participates in the formation of excess tear fluid. Secretion by the main lacrimal gland occurs for the most part only reflexively upon irritation of the cornea, conjunctiva and nasal mucosa, or during psycho-emotional reactions (crying) and reaches 30 ml/min. Normally, with the constant formation of tear fluid, it does not participate [1]. The functioning of the lacrimal gland begins 2 months after birth[4], which is why practically no lacrimation is observed before this age; in old age, the function of the lacrimal gland gradually declines[5].
In addition to the main lacrimal gland, in the conjunctiva of the sclera and eyelids there are several dozen additional small lacrimal glands that produce tears to constantly moisturize the eyes with tear fluid under normal conditions. The tear secreted by the accessory lacrimal glands accounts for about 10% of its total secretion.
, amounting to 0.5-2 ml/day and provides basal hydration of the eyes under normal conditions. This explains, in particular, that if the main lacrimal gland is damaged, the eye does not dry out. Accessory lacrimal glands can be damaged by chemical burns of the conjunctiva[1][4].
The human lacrimal glands perform a number of essential functions that are responsible for maintaining the normal and constant functioning of the cornea and conjunctiva. The lacrimal glands produce tears, the main water-containing component of the tear fluid, which performs the optical, trophic and protective function of the outer anterior surface of the eyeball. The lacrimal glands also secrete mucins, which make up 50% of tears [1].
Treatment
Treatment always depends on the causes of the disease.
To compensate for impaired tear production, replacement therapy is most often recommended in the form of regular administration of drugs with a composition identical to the tear fluid. For a longer presence of tears in the eye, the paths of its outflow - lacrimal puncta - are sometimes specially blocked with some kind of “plugs”.
Inflammatory diseases of the lacrimal ducts with disruption of their patency require the prescription of anti-inflammatory therapy or surgical restoration of the outflow tract - bougienage or surgical intervention.
Persistent obstruction of the patency of the nasolacrimal duct is an indication for dacryocystorhinostomy surgery, with the performance of an anastomosis - a direct connection between the lacrimal sac and the nasal cavity through the bone septum separating them.
Dagaev Adam Huseinovich
How to feel the tear duct
Finding the tear duct is not difficult and can be done with your index finger. The tear duct is presented in the form of a corner, which is located in the inner corner of the eye at the junction with the bridge of the nose. If you feel this tubercle then remember that this is the lacrimal sac.
Now you know where the lacrimal canal is located in newborns and what problems can arise with this organ. We hope that we have clearly explained what the lacrimal canal is and its functional features.
We recommend reading: how to massage your eyelids without leaving home.