Quote from EFACHKA
Read in full In your quotation book or community!
Anterior chamber of the eye: structure and functions, norm and deviations, photo
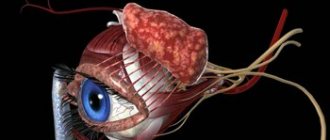
Our organs of vision perform an important function, allowing us to explore the world around us, make new discoveries, etc. But how are they arranged? This is a rather complex “unit”, which consists of two areas: the posterior and anterior chambers of the eye, communicating with each other through the pupil.
By the way, the presence of precisely two eyes allows us to form a three-dimensional image of the space around us.
Front camera
Where is the anterior chamber of the eye located? The anterior region of the eye is limited from the outside by the inner membrane of the cornea (endothelium). Behind it, the border runs along the outer surface of the iris and touches the anterior surface of the lens. The peripheral boundary is the angle of the anterior chamber.
In this case, the described area has different depths - its greatest value is in the pupil zone (3.5 mm). As you move away from the central part to the peripheral areas, the depth decreases, which is the norm.
Changes in chamber depth may be due to pathological changes. When the lens is removed, the depth of the chamber increases. Detachment of the choroid, on the contrary, leads to its reduction. Where the anterior chamber is located is described in detail in this article: https://fb.ru/article/407559/gde-nahoditsya-perednyaya-kamera-glaza-anatomiya-i-stroenie-glaza-vyipolnyaemyie-funktsii-vozmojnyie-zabolevaniya-i- metodyi-lecheniya.
Causes
The occurrence of hyphema can be caused by one of these reasons:
- Eye injury . This is a particularly common cause of intraocular bleeding. In this case, eye injuries are divided into two types - penetrating, with damage to the eye membranes, and non-penetrating (blunt), without damage to the eye membranes. The cause of bleeding into the anterior chamber during penetrating trauma is rupture of the eye membranes, accompanied by rupture of blood vessels. In the case of non-penetrating trauma, vascular rupture and bleeding occur due to a sharp jump in intraocular pressure. In addition to the rupture of blood vessels during a non-penetrating injury, the cause of bleeding can be a rupture of the internal membranes of the eye (the iris, which acts as a protective membrane in the anterior part of the choroid; the ciliary body in the choroid, consisting of a group of muscles that change the shape of the lens; the choroid - the choroid membrane that provides nutrition to the retina).
- Ophthalmic operations . A complication of both abdominal and laser eye surgeries is often the occurrence of hyphema. This occurs due to damage to the vessels of the iris and ciliary body during surgery, resulting in bleeding. Doctors can easily cope with such bleeding during surgery. However, even in the postoperative period, for almost several months, the risk of hyphema remains, since bleeding can occur again from a vessel damaged during surgery. In addition, at the site of the surgical incision, the growth of newly formed vessels often occurs, with defects in the vascular wall and prone to rupture.
- Some eye diseases . Eye diseases accompanied by the growth of newly formed vessels along the iris can also cause hyphema. These diseases include uncompensated severe diabetes mellitus, thrombosis of the central retinal vein and its branches, intraocular tumor formations, etc. Growing newly formed blood vessels have defective, fragile walls, which, at the slightest fluctuation in arterial or intraocular pressure, rupture with bleeding into the anterior chamber of the eye.
- General diseases of the body . Systemic diseases associated with bleeding disorders, such as hemophilia, anemia or blood cancer, often lead to the appearance of hyphema, seemingly without apparent ophthalmological causes. In addition, alcohol abuse can contribute to the occurrence of hyphema.
Blood leaking into the anterior chamber can cause some complications. As a rule, they occur with severe hyphema, with the anterior chamber completely filled with blood. Particularly serious complications in such a situation are: staining of the cornea with blood and a persistent increase in intraocular pressure - secondary glaucoma. Staining of the cornea with blood leads to deterioration of vision even after the hyphema itself resolves, since it does not go away for a long time and can even increase over time.
Rear camera
The posterior region, as you can understand, is located behind the anterior chamber. In this case, its anterior border passes inside the ciliary body and affects the anterior part of the vitreous body.
Almost the entire space of the posterior chamber is covered by the ligaments of Zinn - very thin numerous threads. They provide communication between the ciliary body and the lens capsule.
When the ciliary muscle relaxes or stretches, the degree of tension in the ligaments changes. Due to this, the shape of the lens changes, which in turn affects the ability to look at objects at different distances from the viewer.
Intraocular fluid
Both chambers of each eye are filled with aqueous fluid, which in its chemical composition is as close as possible to blood plasma. This substance contains micronutrients, which helps maintain the functioning of the eye tissues. In addition, there is also an accumulation of waste products that enter the general circulatory system.
As for the volume of fluid in the posterior and anterior chambers of the eye, it fluctuates in the range of 1.23-1.32 cm3. To ensure the normal functioning of all eye systems, it is important that a constant balance is maintained between the production of aqueous humor and its outflow.
Even a slight disruption in the functioning of this harmonious system can lead to a change in intraocular pressure, both up and down. The development of glaucoma is usually accompanied by an increase in this parameter. With subatrophy, low blood pressure is recorded.
But what’s most unpleasant is that neither increased nor decreased values are beneficial. Ultimately, partial or complete blindness may occur.
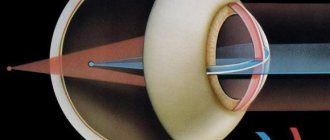
Aqueous humor is produced by processes of the ciliary body, which are responsible for filtering blood in small vessels. That is, it is formed in the posterior chamber, after which it enters the anterior region of the eyeball. The outflow of fluid occurs through the angle of the anterior chamber. This becomes possible due to the lower pressure of the venous vessels. It is in them that the absorption of intraocular fluid occurs.
REFERENCE INFORMATION AND INDICATIONS
Ocular complaints are estimated to account for 3% of all emergency department visits annually in the United States. The eye is a fluid-filled structure that provides an ideal acoustic window for sonographic assessment of intraocular and adjacent structures. Sonography has become a useful adjunct to the traditional evaluation of ocular pathology because it can provide additional information that is not obvious on physical examination and can help identify pathology and speed up treatment. It has been shown that emergency physicians can accurately recognize various ocular disorders using ultrasound compared to other imaging modalities such as orbital computed tomography (CT).
As with many focused ultrasound examinations performed in the acute setting, bedside ocular ultrasonography is a specialized examination and therefore has a limited range of coverage. The main purpose of an ultrasound examination of the eye is to identify pathology that requires immediate intervention and/or threatens the patient’s vision. Ocular sonography can be useful in both traumatic orbital and head injuries and in the evaluation of non-traumatic ophthalmic complaints. Sonographic ultrasound assessment of the orbit is especially useful for patients in whom physical and fundoscopic examination is limited by pain or swelling, or if the patient's eyelids cannot be sufficiently opened (Figure 1).
Rice. 1. Periorbital hemorrhage (H) and edema precluded physical and fundoscopic examination of the eye in this patient who suffered blunt trauma. Sonography allowed assessment of orbital structures, including normal orbital bone (OB) and posterior optic nerve (ON).
Sonographic evaluation can also effectively diagnose injuries in the posterior segment of the eye, such as vitreous hemorrhage, retinal detachment, lens luxation, or intraophthalmic foreign body, which may be hidden in the setting of corneal edema or anterior chamber hemorrhage, a condition known as hyphema. For traumatic injuries, ultrasound has been shown to be an accurate tool in assessing extraocular ocular movements, which are often difficult to assess in the setting of edema. In addition, ultrasound can be used to evaluate the pupillary light reflex in a swollen eye. The affected eye is visualized using ultrasound, and pupil constriction may be observed when light enters the contralateral, unaffected eye. In the case of head trauma, ocular sonography can help quickly diagnose increased intracranial pressure by detecting an increase in optic nerve sheath diameter (ONSD). Bedside ocular ultrasonography is also useful in the evaluation of patients with non-traumatic pathology that requires urgent treatment, such as central artery or retinal vein occlusion.
Camera functionality
Both the anterior and posterior chambers of the eye under normal conditions have a constant volume, which is precisely achieved by regulating the formation of intraocular fluid and its subsequent outflow. In this case, the posterior region of the eyeball, and in particular, the ciliary processes of the ciliary body, takes part in the formation of this fluid. And the anterior region, namely its drainage system, participates in its outflow.
In addition, both the anterior and posterior chambers perform another equally important function - supporting the normal relationships of intraocular tissues. In addition, these areas provide support in conducting light rays to the retina.
The required level of refraction is ensured due to the fact that the cornea and intraocular fluid have identical optical properties. Thanks to this, the rays are focused on the retina in a certain place, due to which, in fact, a clear image is formed.
Diseases of the chambers of the eye
Various diseases can lead to disruption of the structures located inside the anterior and posterior chambers of the eye.
These include:
- Congenital absence of the anterior chamber angle.
- The presence of embryonic tissue in the area of the corner of the eye.
- Violation of the outflow of moisture through the angle of the anterior chamber when it is blocked by pigment, the root of the iris.
- Incorrect attachment of the iris in the anterior region.
- Damage to the lens due to trauma, weakness of the zonules of Zinn, which leads to a change in the size of the anterior chamber. Its depth becomes uneven in different areas.
- Reduction in the size of the anterior chamber, which is possible with synechiae or pupillary fusion.
- Purulent inflammation (hypopyon).
- Hemorrhage into the cavity of the chambers (hyphema).
- Formation of adhesions consisting of connective tissue (synechia).
- Glaucoma associated with an imbalance between moisture synthesis and its outflow.
- Recession of the anterior chamber angle (its splitting).
The structure of the anterior chamber angle of the eye
What is the anterior chamber angle? This definition should be understood as the zone of the anterior region of the eyeball, which corresponds to the transition of the corneal membrane into the sclera and the iris into the ciliary body.
Here is another most important part of the eye - the drainage system. It is due to this that the controlled outflow of intraocular fluid into the bloodstream is carried out.
Structure
The anterior chamber is surrounded on one side by the cornea and on the other by the iris. This cavity is constantly filled with clear liquid. It comes from the posterior chamber of the eye, where it is produced by the ciliary body. Both chambers can be considered communicating vessels. The volume of intraocular fluid in them should always be the same.
The cavity is quite small. Its maximum depth is about 3.5 mm. This indicator should also be stable. Different chamber depths in different areas indicate the development of certain pathologies. An ophthalmologist can determine such quantitative and functional indicators during a standard initial examination.
This component of the visual system is of great importance in the functioning of the entire visual system, but the slightest disturbance in the functioning of the posterior chamber negatively affects other components of the organ. Their examination should be carried out in a comprehensive manner. This is the only way to maintain full vision.
Features of the drainage system
The drainage system consists of several elements:
- trabecular diaphragm;
- collector tubules;
- venous sinus of the sclera (Schlemm's canal).
If you look at a photo of the anterior chamber of the eye, in which the trabecular diaphragm is enlarged, you can see a dense network of porous-layered structure. Moreover, the pore size gradually decreases outward. Actually, due to this, the outflow of intraocular fluid is regulated.
The trabecular diaphragm itself, in turn, is represented by several plates:
- juxtacanalicular;
- uveal;
- corneo-scleral.
After the intraocular fluid overcomes the trabecular meshwork, it is directed into the narrow slit-like space of Schlemm's canal. It is located near the limbus in the thickness of the sclera.
Pathways for the outflow of intraocular fluid
Thanks to the collector tubules, which are located in the scleral sinus, the outflow of intraocular fluid occurs directly into the venous system. Outflow occurs in three ways:
- deep intrascleral venous plexus;
- superficial scleral venous network;
- episcleral venous vessels.
At the same time, there is an additional path for the outflow of moisture from the anterior chamber of the eye, located outside the trabecular meshwork (uveoscleral). It accounts for about 15% of all flowing fluid. Moreover, moisture is first directed from the angle of the anterior chamber to the ciliary body, after which it moves along the fibers of the eye muscles and then penetrates into the suprachoroidal space.
And only from here the fluid decreases in several directions: along venous outlets, directly through the sclera, or using Schlemm’s canal.
Treatment
The treatment method for a patient with hyphema is selected depending on the cause of the hemorrhage, the volume of blood shed, the duration of the hyphema, and the presence of complications.
To resolve the hyphema, blood thinners (anticoagulants, antiplatelet agents) must be temporarily discontinued. The patient is prescribed hemostatic agents, absorbable and vascular-strengthening drugs. If systemic blood coagulation disorders are detected, appropriate treatment for the disease is prescribed.
In some cases of hyphema, there are objective indications for surgery. It is required to remove blood or a blood clot from the anterior chamber of the eye if the cornea has already begun to stain; when the blood has coagulated to form a clot; if the entire volume of the anterior chamber is filled with blood and treatment carried out for 10-15 days does not help its resorption; when there is an increase in intraocular pressure, and the ongoing treatment using local and systemic drugs does not provide the desired effect.
The occurrence of hyphema is a rather dangerous condition due to the development of serious complications, and therefore requires immediate seeking specialized help.
Patients of our clinic have the opportunity to perform the necessary diagnostic procedures and receive advice from experienced specialists without tiring queues, at a time convenient for this. If necessary, they will be provided with emergency assistance or prescribed adequate treatment in accordance with international standards for the provision of medical services.
Undesirable symptoms
Now we know what an important role both ocular areas play in ensuring the functioning of the entire visual apparatus. For this reason, any detected violations should not be ignored! Moreover, all symptoms can be divided into two main categories - congenital and acquired.
The list of congenital characteristics includes the following cases:
- Complete absence of anterior chamber angle.
- Blockage of the chamber angle by embryonic tissues that did not have time to dissolve after the birth of the child.
- Improper fixation of iris tissue.
The number of acquired characteristics significantly exceeds congenital factors:
- Blockage of the angle of the anterior chamber of the eye by the root of the iris or other structures.
- Circular synechia or partial pupillary fusion. As a rule, this ends in a decrease in the volume of the anterior chamber or bombardment of the iris.
- Accumulation of purulent mass in the anterior chamber (hypopyon).
- Hemorrhage in the anterior region of the eyeball (hyphema).
- Damage to the trabecular system, including the iris of the anterior chamber angle (goniosynechia).
- Recession of the anterior chamber angle is a rather rare phenomenon, which, in addition, cannot always be diagnosed.
These symptoms appear throughout a person's life, and their occurrence can be associated with various injuries.
At the same time, we cannot exclude the influence of ophthalmological diseases, not only in relation to the organs of vision, but also the entire body as a whole.
OUTER EYE
TRADITIONAL OPINION OF TEACHERS
Many outdoor studies are carried out using a flashlight pen. You should carefully examine the orbits, the position of the eyelids, the conjunctiva, the anterior chamber of the eye and examine the corneal reaction to light.
Tears
40. What is the Schirmer test?
The Schirmer test aims to measure tear production. It is carried out to determine dry eyes due to keratoconjunctivitis or Sjögrep syndrome. Sjögren's syndrome is an autoimmune disease characterized by dry eyes and dry mouth. Often accompanied by other autoimmune disorders.
41. What is the Schirmer test?
Under local anesthesia, the doctor inserts a small strip of filter paper under the lower eyelid on the medial or lateral side. The test strip should not be in the center. After 5 minutes it is removed. The wet spot formed by tears is measured in millimeters. Normally, its dimensions correspond to 15 mm (before 40 years) and 10 mm (after 40 years). A distance of less than 5 mm usually indicates decreased tear production. A distance from 5 to 10 mm is suspicious for its decrease.
42. Who is Schirmer?
Otto Schirmer (1864-1917) was a German ophthalmologist.
Brows
43. What is the significance of thinning or absence of the lateral portion of the eyebrows?
Thinning or absence of the lateral portion of the eyebrows is a common symptom of hypothyroidism (often called the “Queen Anne sign” after a famous patient). However, it may also be a variant of the norm. The appearance of eyebrows can also be the result of cosmetic manipulation (plucking). Other causes include medications, skin diseases, and lupus.
Eyelids and orbits
44. What is xanthelasma?
Xanthelasma (from the Greek words xanthos - yellow and elasma - forged metal plate) is a yellowish fatty deposit located on top of the eyelid. Most patients with xanthelasma do not have lipid metabolism disorders. However, xanthelasmas occur in 25% of patients with type 3 hyperlipoproteinemia and also occur in the more common types 2 and 4 hyperlipoproteinemia. If xanthelasmas are a cosmetic problem, they are removed surgically.
Rice. 4.4. A patient with xanthelasmas on all four eyelids. (Reproduced with permission from: Tasman W., Jaeger E.L.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven, 1996.)
45. What is ectropion?
This is eversion (outward turning) of the lower eyelid. Often found in older people. In this case, the edge of the dorsal conjunctiva opens to external stimuli. Exposed corneas and keratinization of the exposed conjunctiva can lead to eye irritation.
46. What is entropion?
This is an inversion (inward folding) of the lower eyelid. Often occurs in old age. May also cause mechanical irritation to the eye due to contact with eyelashes.
47. What is barley?
This is an acute focal inflammatory process in one of the glands located along the edge of the eyelid (for example, a hair follicle). Classic signs are redness, swelling, tenderness and sometimes purulent discharge.
48. What is blepharitis?
This is a diffuse inflammatory process that involves the edge of the eyelid. Characterized by swelling and redness. Blepharitis is usually caused by Staphylococcus aureus or Staphyloccocus epidermidis and may be hypersusceptible. The edge of the eyelid may become crusty, covering the eyelashes. Patients often complain of dry eyes.
49. What is ptosis?
Ptosis (fall in Greek) is the drooping of the upper eyelid. Can be one- or two-sided.
Rice. 4.5. Involutional (aponeurotic) ptosis, too mild to smooth out the depth of the eyelid folds. The function of the levator muscle is usually preserved. (Reproduced with permission from: Tasman W., Jaeger E.A.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven. 1996.)
50. What are the causes of ptosis? How are they differentiated?
Common reasons include age (1); consequences of injuries and surgical procedures (2) and congenital causes (3). Less commonly, ptosis is caused by myasthenia gravis (1), Horner's syndrome (2), and third cranial nerve palsy (3). These reasons differ from the first three in the presence of a combined pathology: changes in the size of the pupils and paresis of other cranial nerves.
51. What is proptosis?
Proptosis (or exophthalmos) is an abnormal protrusion of one or both eyeballs (from the Greek word proptosis, meaning prolapse forward). Normally, the eyeballs can protrude forward by 19 - 24 mm, depending on race and gender. If one eye protrudes forward by more than 2 mm compared to the other eye, we speak of unilateral exophthalmos.
52. What are the most common causes of proptosis in adults?
The most common cause of unilateral exophthalmos is thyroid ophthalmopathy (Graves' disease). In second place are space-occupying formations (metastatic or primary tumors, malignant and benign). The main cause of bilateral exophthalmos is also Graves' disease. Next come cancer.
53. What are other signs of ophthalmopathy in thyrotoxicosis?
- Retraction of the eyelids (thyroid gaze).
- The upper eyelid lags behind when looking down (van Greif sign).
- Conjunctival edema (chemos) and hyperemia.
- Rare blinking and proitosis (Stellwag's sign).
- Slight tremor of loosely closed eyes (Rosenbach's sign).
- Violation of eye convergence following accommodation from a distance of 12.5 cm (Moebius sign).
- Weakening of extraocular mobility.
- Ulceration of the cornea.
- Compression of the optic nerve, leading to swelling and loss of vision.
Rice. 4.6. Ophthalmopathy in thyrotoxicosis with proptosis and eyelid retraction. (Reproduced with permission from: Vander JF, Gault JA: Ophthalmolo do Secrets. Philadelphia, Hanley and Belfus, 1998.)
54. What is the most common cause of unilateral proptosis in children?
The most common cause is cellulitis. Of the space-occupying lesions, unilateral exophthalmos in children is most often caused by rhabdomyosarcoma.
55. What are the differences between preseptal and orbital cellulitis? Preseptal cellulitis affects only the eyelids, which become red and swollen. The process does not affect either the orbital septum or its structures. There is no impression that the patients' ocular system is affected. Vision, pupils, conjunctivae and eye mobility remain normal.
In contrast, orbital cellulitis is an emergency. It affects not only the eyelids, but also the orbital structures. Patients give the impression of being systemic patients. Numerous symptoms include pain with eye movement (O); redness and swelling of the eyelids (2); conjunctival injection and chemosis (swelling) (3); limited eye movement on the affected side (4); proptosis (5); decreased vision (6 ); defect of afferent pupillary fibers (7).
56. What are the signs of an orbital fracture?
This is a fracture of the orbital floor (which is also the roof of the maxillary sinus). The inferior orbital rectus muscle may become impinged. In patients with blunt orbital trauma, the orbital rim should be palpated for mobility or discontinuity. The surrounding soft tissue should also be carefully palpated for subcutaneous crepitus. The latter is caused by air coming from the damaged maxillary sinus. Air bubbles are sometimes visible on the conjunctiva when illuminated with a flashlight. Patients also need to check the sensitivity on the side of the injury in the area of distribution of the 5th cranial nerve. Loss of sensation indicates a fracture. When the inferior rectus muscle is pinched, the patient cannot look up or complains of diplopia when looking up.
57. What is enophthalmos?
Enophthalmos is the opposite of exophthalmos (literally falling inward). The eyes are immersed in the orbits rather than protruding from them. Enophthalmos may result from extensive fracture of the orbit.
Rice. 4.7. Pseudoptosis in a patient with an orbital fracture. (Reproduced with permission from: Tasman W., Jaeger E.L.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven, 1996.)
Diagnostic methods
Since the human visual system is quite complex, most disturbances in its functioning cannot be detected by a simple visual inspection. In this regard, in order to make an accurate diagnosis, patients need to undergo a whole range of diagnostic and laboratory tests.
The most common methods of examining the eye chambers include the following procedures:
- Study of the eye chambers in transmitted light.
- Biomicroscopy is a detailed study of ocular structures using a slit lamp.
- Gonioscopy is a modern technique for examining the anterior chamber angle using a gonioscope.
- Ultrasound, including ultrasound biomicroscopy.
- Optical coherence tomography is a non-invasive (that is, non-contact) technique that examines the structure of the eye tissues.
- Pachymetry - to assess the depth of the anterior chamber.
- Tonometry - allows you to determine intraocular pressure.
- Tonography – is carried out to assess the production and outflow of moisture in the eyeball.
Such a variety of studies makes it possible to promptly identify occurring disorders in the eyeball and take the necessary measures.
Features of the course of therapy
Treatment of any dysfunction of the posterior and anterior chambers of the eye or their structures should be carried out only in specialized clinics using modern equipment. As a rule, the goal of therapy comes down to reducing the factors that provoke various disorders of the visual apparatus.
The drug course of treatment can be supplemented with anti-inflammatory drugs. Also, if necessary, procedures can be performed to relieve swelling caused by impaired outflow of moisture from the eyeball.
The structure of chamber formations
The anterior chamber of the eye is located directly behind the cornea. The peculiarity of the “element” is that it has different depths along its entire length. The greatest depth is in the area of the pupil, the indicator reaches three and a half millimeters, it decreases towards the periphery. Aberration in camera parameters can become a symptom of an eye disease. For example, the depth increases after removal of the lens or decreases when the mucous membrane is detached.
The posterior chamber of the eye is located directly behind the anterior chamber and contains many tiny zonules of Zinn, which act as a “connecting” element between the lens and the ciliary body. They are also responsible for the contraction of the ciliary muscles, whose task is to transform the shape of the lens. Thanks to this, a person sees well at any distance.
Both chambers are filled with a liquid identical in composition to blood plasma. Moisture contains a large amount of useful substances that are transferred to the organ of vision and ensure its smooth operation. The liquid also accepts metabolic products from the eye, after which it “redirects” them to the circulatory system. Moisture is produced through the ciliary processes of the ciliary body, and outflow occurs through the drainage system.
| The volume of the posterior and anterior chambers holds from 1.23 to 1.32 cubic centimeters of intraocular fluid. It is important to maintain a balance between the decrease and increase of moisture inside the eye. When the indicator shifts, the smooth operation of the visual apparatus is disrupted. |
If more fluid is produced than comes out, glaucoma develops. In the opposite situation, there is a high risk of eye subatrophy. Any slight imbalance has a negative impact on the functioning of the eyes and can even lead to blindness.
The volume of chamber formations in the visual apparatus must be stable; this is the only way to ensure uninterrupted production of intraocular moisture and its outflow.