The eye is considered one of the key sensory organs. It plays a vital role in a person’s perception of the world around them. In the diverse activities of people, the organ of vision is of paramount importance. The eyes capture light and direct it to sensitive cells. A person can recognize color and black and white images, see objects in volume at different distances. The organ of vision is paired and is located in the cranial fossae of the facial part. It is surrounded by the auxiliary apparatus of the eye.
Structure of the retina
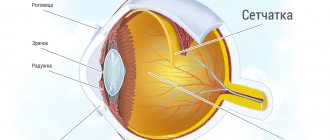
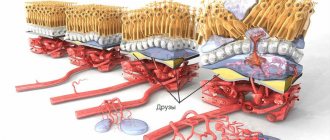
The inner shell has two parts: a large back and a smaller front. The latter combines the iris and ciliary sections. The visual part includes the internal pigment and neural regions. The latter contains about 10 layers of cells. They enter the inner part of the shell with processes in the form of rods and cones. Due to them, a person perceives rays in daylight and twilight. Other nerve cells play a connecting role. Their axons, connecting into a bundle, emerge from the shell.
Outer cover
Sclera
The anatomical features of the membrane covering the eye lie in its heterogeneity. The back part is represented by a denser layer - the sclera. It is opaque, as it is formed by a random accumulation of fibrin fibers. Although in infants the sclera is still so tender that it has a blue tint rather than a whitish one. With age, lipids are deposited in the membrane, and it characteristically turns yellow.
This is the supporting layer that provides shape to the eye and allows attachment of the extraocular muscles. Also in the back of the eyeball, the sclera covers the optic nerve, which extends from the eye, for some extent.
Cornea
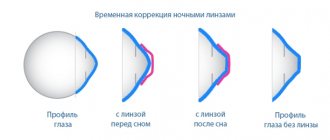
The eyeball is not completely covered with sclera. In the anterior 1/6 part, the shell of the eye becomes transparent and is called the cornea. This is the dome-shaped part of the eyeball. It is on its transparency, smoothness and symmetry of curvature that the nature of the refraction of rays and the quality of vision depend. Together with the lens, the cornea is responsible for focusing light onto the retina.
Tasks
First of all, it should be noted the protective functions of the auxiliary apparatus of the eye. It provides hydration to the front surface of the organ of vision, preventing it from drying out. In addition, this section helps remove foreign particles. The functions of the auxiliary apparatus of the eye include the destruction of bacteria that fall on the surface of the organ. The department also promotes the removal of substances that are formed during stress and nervous tension. They come out with tears.
Visual apparatus
At the inner corner of both eyelids there are points called lacrimal, from which the lacrimal canaliculi originate. The gland that produces tear fluid is located under the upper eyelid in the fossa of the orbit. About 15 ducts emerge from it, which drain fluid from the gland into the lacrimal sac at the border of the lower eyelid and eye.
The composition of the lacrimal substance includes the substance lysozyme, which has antibacterial properties. Near the inner corner of the eye, in a small depression called the lacrimal lake, this liquid substance is concentrated.
It has already washed the surface of the organ and moves through the excretory canals into the duct connecting to the nasal sinuses. There it dries. Functions of tear fluid:
- nutrition and hydration of the cornea;
- prevents drying of the conjunctiva and cornea;
- promotes cleansing of foreign bodies;
- plays the role of a lubricating fluid when flashing;
- releases emotions in the form of crying.
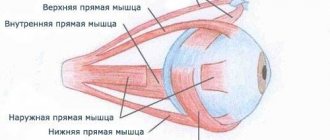
Muscles
Humans have a unique eye structure. An auxiliary apparatus is a department without which the normal functioning of an organ would be impossible. Muscles are of particular importance. Attached to the apple are 4 rectus (medial, lateral, inferior, superior), 2 oblique (lower and superior) muscles. Almost all of them come from the depths of the orbit, starting from the tendon ring. The exception is the inferior oblique muscle. Partially the fibers extend from the edges of the orbital (superior) fissure. The muscle that lifts the eyelid originates from the tendon ring. It is located in the orbit above the straight fiber. It ends in the thickness of the eyelid. The rectus muscles are directed along the walls of the orbit. They are located on the sides of the nerve. In front of the equator, at a distance of 5-8 mm from the edge of the cornea, the muscles are woven into the sclera with the help of short tendons. The rectus muscles ensure rotation of the apple around axes that mutually intersect each other. It moves left and right vertically and down and up horizontally. The lateral muscle turns the apple outward, the medial muscle turns it inward relative to the vertical axis. At the fixation site, a tendon stretch is the first to form. Most of its bundles are woven into the sclera. Some of them extend forward and outward. Subsequently, they are fixed on the lateral wall. The lower and upper straight fibers ensure the rotation of the apple relative to the horizontal axis. The former participate in the movement downwards and inwards, the latter - upwards and slightly outwards.
The superior oblique muscle arises from the tendon ring. It lies in the superomedial region of the orbit. Near the lateral fossa, the fibers pass into a round thin tendon covered with a synovial sheath. It runs through a block that looks like a ring made up of fibrous cartilage. Next, the tendon deviates slightly posteriorly and outward. Passing under the rectus superioris muscle, it is fixed on the superolateral part of the apple at a distance of approximately 18 mm from the edge of the cornea. The oblique top fibers provide outward and downward rotation. The inferior muscle arises from the orbital surface in the upper jaw near the opening of the nasolacrimal duct. Next, it is directed outward and backward, passing between the straight fibers and the wall of the orbit. The muscle is fixed on the lateral surface behind the equator. It ensures the apple rotates outward and upward. The muscular structures of the auxiliary apparatus of the eye work in concert. By this they ensure the synchronization of the movement of the left and right apples.
Accessory organs of the eye
The auxiliary organs of the eye include the muscles, eyelids, conjunctiva and lacrimal apparatus.
Motor apparatus of the eye
represented by striated muscles that move the eyeball. The muscles are distinguished: superior, inferior, medial and lateral rectus and superior and inferior oblique. All these muscles begin from the tendon ring deep in the orbit in the circumference of the optic canal (with the exception of the inferior oblique, which originates from the lower wall of the orbit) and are attached to the sclera. The rectus muscles rotate the eyeball up, down, laterally or medially, and the oblique muscles turn the eyeball down and out (superior oblique) or up and out (inferior oblique). Thanks to the joint action of the muscles, the eyeball can rotate around any axis. In addition to the rectus and oblique muscles, the orbit also contains the muscle that lifts the upper eyelid.
The eyeball is covered with a connective tissue sheath, which is connected to the sclera by loose connective tissue. Between the periosteum of the orbit and the vagina of the eyeball lies the fatty body of the orbit.
The eyelids,
palpebrae
, protect the eyeball and ensure uniform distribution of tear fluid and its movement to the inner corner of the eye. The upper and lower eyelids are folds of skin along the edges of which eyelashes grow. Between the free edges of the upper and lower eyelids there is a palpebral fissure. Its inner corner is rounded and forms a tear lake. At the base of the eyelids there is a dense connective tissue plate, in the thickness of which there are sebaceous glands (meibomian), the secretion of which lubricates the edges of the eyelids and eyelashes. The back surface of the eyelids is covered with a connective membrane (conjunctiva of the eyelids), which passes from the eyelids to the visible part of the sclera (conjunctiva of the eyeball). At the junction of the conjunctiva from the eyelids to the eyeball there are the upper and lower fornix of the conjunctiva.
Lacrimal apparatus
consists of the lacrimal gland and lacrimal ducts. The lacrimal gland is located in the superolateral corner of the orbit. It produces tear fluid that moisturizes the eyeball. Through the excretory ducts of the lacrimal gland, tears are secreted into the conjunctival sac and, washing the eyeball, enter the medial corner of the eye to the lacrimal lake, and from there into the lacrimal canaliculi. The superior and inferior lacrimal canaliculi begin as pinholes on the medial part of the eyelids and open into the lacrimal sac, which continues into the nasolacrimal duct. The latter opens into the nasal cavity into the lower nasal meatus.
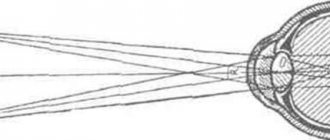
Light rays, passing through the light-refracting media of the eyeball, enter the retina, where they are perceived by rods and cones. Visual information travels to the bipolar cells and then to the retinal ganglion cells. The axons of ganglion cells form the optic nerve, which leaves the orbit through the canal of the same name and forms an incomplete decussation at the base of the brain (the medial fibers are decussated). Next, the fibers in the optic tract follow to the subcortical centers of vision - the lateral geniculate body and the cushion of the visual thalamus. The cortical end of the analyzer is located in the occipital lobe along the banks of the calcarine groove.
Rice. 2. Visual analyzer. 1 – optic nerve; 2 – visual chiasm; 3 – optic tract; 4 – thalamus; 5 – pillow; 6 – lateral geniculate body; 7 – handle of the superior colliculus; 8 – superior colliculus; 9 – occipital lobes; 10 – tegnospinal tract.
Some of the fibers of the optic tract reach the nuclei of the superior colliculi of the midbrain roof and, thanks to their connections with the motor nuclei of the cranial nerves and autonomic centers, it is possible to place the eyes on the object in question and automatically regulate the size of the pupil. Their connection with the motor nuclei of the spinal cord (tegnospinal tract) facilitates the transmission of impulses to the striated muscles, providing appropriate movements in response to visual information.
Organ of hearing and balance
The organ of hearing includes three sections: the outer, middle and inner ear.
External ear, auris externa
, consists of the auricle and the external auditory canal.
Auricle
represented by elastic cartilage covered with skin.
Along the edge of the auricle it forms a helix, helix,
in front of which there is
an antihelix, anthelix.
In front of the external auditory opening there is a protrusion, the tragus, opposite it behind the opening there is an antitragus. The external auditory opening leads into the external auditory canal.
External auditory canal, meatus acusticus externus
, is an S-shaped curved canal that ends blindly with the eardrum. There are smaller cartilaginous and larger bony parts of the external auditory canal. The skin of the cartilaginous part of the external auditory canal is rich in sebaceous glands and glands that secrete earwax.
Eardrum, membrana tympani,
a thin, oval plate that separates the external auditory canal from the middle ear. The eardrum is divided into skin (outer) and mucous (inner) layers, between which there are fibrous fibers. The upper part of the membrane, where these fibers are absent, is called the free, unstretched part, and the lower part is called the tense part. In the center of the membrane on the outside there is a depression - the navel of the eardrum, caused by the attachment of the hammer handle in this place on the inside.
The middle ear,
auris media,
consists of the tympanic cavity and the auditory tube.
Tympanic cavity, cavitas tympanica,
located at the base of the pyramid of the temporal bone between the external auditory canal and the inner ear.
The tympanic cavity has six walls. Upper (tegmental)
- separates the tympanic cavity from the cranial cavity.
Lower (jugular)
- facing the base of the skull and separates the tympanic cavity from the internal jugular vein.
Medial (labyrinthine)
– separates the tympanic cavity from the bony labyrinth of the inner ear.
It has two openings: the window of the vestibule, closed by the base of the stapes, and the window of the cochlea, covered by the secondary tympanic membrane. The lateral (membranous)
is formed by the tympanic membrane and the surrounding parts of the temporal bone.
The anterior (carotid)
separates the tympanic cavity from the canal of the internal carotid artery.
At the top of this wall, the tympanic opening of the auditory tube opens. The posterior (mastoid) wall
faces the mastoid process. In its upper section there is an entrance to the cave.
Rice. 3. Auditory ossicles. 1 – head of the malleus; 2 – hammer handle; 3 – anvil body; 4 – short leg; 5 – long leg; 6 – head of the stirrup; 7 – base of the stirrup; 8 – front leg; 9 – rear leg.
The tympanic cavity contains three auditory ossicles: the malleus, the incus and the stapes.
which form a circuit that transmits sound vibrations from the eardrum to the window of the vestibule leading to the inner ear. The handle of the malleus is fused with the eardrum, and the head is fused with the body of the incus. The incus articulates with the stapes, the base of which covers the window of the vestibule. Two muscles are attached to the auditory ossicles that regulate their movements: to the handle of the malleus - the muscle that strains the tympanic membrane (moves the ossicles towards the window of the vestibule), to the leg of the stapes - the stapedius muscle (moves the ossicles towards the tympanic membrane).
Eustachian tube
serves to conduct air from the nasopharynx into the tympanic cavity, thereby balancing the pressure of the tympanic cavity with external pressure. The auditory tube has bone and cartilaginous parts. The cartilaginous part opens with the pharyngeal opening on the lateral wall of the nasopharynx.
The inner ear,
auris interna
, is located in the pyramid of the temporal bone between the tympanic cavity and the internal auditory canal. It consists of a bony labyrinth and a membranous labyrinth located in it, between which there is a perilymphatic space filled with perilymph.
The bony labyrinth is divided into: the vestibule, semicircular canals and cochlea.
Rice. 4. Bone labyrinth. 1 – anterior semicircular canal; 2 – common bone pedicle; 3 – lateral bone ampulla; 4 – posterior semicircular canal; 5 – lateral semicircular canal; 6 – posterior bone ampulla; 7 – window of the vestibule; 8 – cochlear window; 9 – vestibule; 10 – snail; 11 – spherical recess; 12 – elliptical recess.
vestibule, vestibulum
- an expanded middle section of the bony labyrinth, communicating posteriorly with the semicircular canals, and anteriorly with the cochlear canal. On the lateral wall of the vestibule there is a window of the vestibule and a window of the cochlea, and on the medial wall there are spherical and elliptical recesses.
Bone semicircular canals
, form the posterior section of the bony labyrinth and are located in three mutually perpendicular planes: sagittal (anterior canal), horizontal (lateral) and frontal (posterior canal). Each canal is arched and has one expanded (ampullary) leg. The simple legs of the anterior and posterior semicircular canals are connected into a common stalk, and therefore, three canals open into the vestibule with five openings.
Snail, cochlea
, located anteriorly and is a bony spiral canal that starts from the window of the vestibule and forms two and a half circular passages around the bone rod. From this rod, along its entire length, a spiral bone plate extends into the cavity of the cochlear canal, which (together with the cochlear duct of the membranous labyrinth) divides the cochlear canal into the scala vestibule and the scala tympani. At the apex of the cochlea they communicate with each other.
The membranous labyrinth (Fig. 5) is located inside the bone labyrinth, it is filled with endolymph and consists of the following sections: spherical and elliptical sacs and semicircular ducts, which constitute the organ for recording movement and maintaining balance, as well as the cochlear duct, which belongs to the organ of hearing.
Spherical sac, sacculus
, and
the elliptical sac or utricle, utriculus,
are located in the same recesses of the bony vestibule and communicate with each other.
The sac in front, through the connecting duct, communicates with the cochlear duct, and the semicircular ducts, ductus semicirculares,
located in the corresponding bony semicircular canals, open into the uterus from behind.
Each semicircular duct has one expanded leg - ampulla
.
On the inner surface of the membranous labyrinth there are clusters of sensitive hair cells with a gelatin-like mass. In the ampoules of the semicircular ducts they are presented in the form of scallops that are capable of perceiving rotational (angular) accelerations, in the sac and uterus - in the form of spots. The otolithic apparatus of the saccule and uterus (the gelatin-like mass of the spots contains crystals of calcium carbonate) perceives changes in the position of the head and linear acceleration.
Rice. 5. Membranous labyrinth. 1 – spherical sac; 2 – cochlear duct; 3 – elliptical pouch; 4 – membranous ampulla; 5 – posterior semicircular duct; 6 – lateral semicircular duct; 7 – anterior semicircular duct.
The movements of the endolymph during body movement are perceived by the receptor apparatus of the cells located in the area of ridges and spots. The resulting nerve impulse is transmitted along the dendrites to the neuron bodies of the vestibular node, located at the bottom of the internal auditory canal (Fig. 6). The central processes of neurons form the vestibular part of the VIII pair of cranial nerves, which goes to the vestibular nuclei of the brain stem.
Rice. 6. Scheme of a statokinetic analyzer: 1 – macula of the sac and utricle; 2 – vestibular ganglion; 3 – lateral vestibular nucleus; 4 – superior vestibular nucleus; 5 – vestibulospinal tract; 6 – tent cores; 7 – medial loop; 8 – thalamus; 9 – thalamo-cortical tract; 10 – superior temporal gyrus
From them, information flows to the visual thalamus, and then to the cortex of the middle and inferior temporal gyri, where the cortical end of the statokinetic analyzer is located. In addition, the impulse from the vestibular nuclei enters the cerebellum, spinal cord, and reticular formation, resulting in involuntary muscle contractions that coordinate movements and align the body position.
Cochlear duct, ductus cochlearis,
is located in the spiral canal of the bony cochlea and in cross section has the shape of a triangle.
Its outer wall is fused with the bony cochlea. The upper (vestibular) wall separates the cavity of the cochlear duct from the scala vestibule, and the lower wall separates it from the scala tympani. The lower wall is represented by a basilar membrane formed by fibers of different lengths that act as resonator strings. On the basilar membrane there is a spiral organ (Corti)
in the form of sensitive hair cells with a covering membrane above them, which is the receptor of the auditory analyzer.
Sound waves reach the eardrum through the external auditory canal, the vibrations of which are transmitted to the chain of auditory ossicles. Movements of the stapes in the window of the vestibule cause vibrations of the perilymph of the scala vestibule, and then the scala tympani, which ends with the window of the cochlea, where the waves are attenuated due to the presence of a secondary tympanic membrane. Vibrations of the perilymph are transmitted to the endolymph, as a result of which a nerve impulse arises in the receptor cells, which is carried along the dendrites to the body of the nerve cells of the spiral ganglion, located at the base of the bony spiral plate. The central processes of these cells form the cochlear part of the VIII pair of cranial nerves, which goes to the ventral and dorsal nuclei of the rhomboid fossa, where the impulse switches (Fig. 7).
| Rice. 7. Diagram of an auditory analyzer. 1 – receptor (organ of Corti); 2 – spiral ganglion; 3 – ventral nucleus; 4 – dorsal nucleus; 5 – brain stripes; 6 – trapezoidal body; 7 – tegnospinal tract; 8 – lateral loop; 9 – dorsal decussation of the tegmentum; 10 – nuclei of the inferior colliculi; 11 – medial geniculate bodies; 12 – superior temporal gyrus. |
The axons of the neurons of the auditory nuclei pass to the opposite side, forming the trapezoid body and the medullary striae of the fourth ventricle, and then, as part of the lateral loop, go to the subcortical auditory centers - the medial geniculate body and the lower colliculus of the roof of the midbrain. From the medial geniculate body, the impulse enters the cortex of the superior temporal gyrus, where the cortical end of the auditory analyzer is located.
From the lower colliculi of the midbrain, the descending motor path begins to the motor nuclei of the spinal cord (tectospinal tract), the axons of which, as part of the spinal nerves, are directed to the striated muscles, resulting in instinctive movements to auditory stimuli.
Olfactory organ
The olfactory organ is located in the mucous membrane of the superior turbinate and the adjacent small part of the nasal septum. This organ includes olfactory neurosensory cells, the receptors of which perceive the smell of substances dissolved in the water vapor of the nasal cavity and the secretion of the glands of the mucous membrane. The central processes of the olfactory cells form thin nerve trunks that make up the olfactory nerves, which pass into the cranial cavity through the openings of the cribriform plate to the olfactory bulb
, where the impulse switches to the mitral cells of the olfactory glomeruli.
The fibers of these neurons as part of the olfactory tract end in the subcortical olfactory centers ( olfactory triangle, anterior perforated substance, septum pellucidum),
from where the impulse reaches
the uncinate cortex
of the parahippocampal gyrus, where olfactory information is analyzed and the corresponding sensations are formed.
Organ of taste
The taste organ is represented by taste buds of the mucous membrane of the tongue (in the grooved, foliate and fungiform papillae), epiglottis, soft palate and posterior wall of the pharynx. In the receptors, under the influence of the chemical components of food substances, a nerve impulse arises, which along the dendrites reaches the bodies of the neurons of the sensory nodes VII, IX and X pairs
cranial nerves.
Their central processes end in the nucleus of the solitary tract, located in the rhomboid fossa. The next neuron is located in the optic thalamus
, from where the impulse reaches
the uncinate cortex
of the parahippocampal gyrus, where it is perceived in the form of various taste sensations.
General cover
skin, cutis,
protects the body from external influences, participates in thermoregulation, metabolic processes, perceives environmental irritations (touch, pressure, temperature, pain). From receptors located in the skin, pathways are formed along which the impulse reaches the cerebral cortex. The path of the skin analyzer is outlined in the chapter “Central Nervous System. Pathways."
The skin is divided into: the superficial layer, epidermis,
formed from the ectoderm, and a deep layer of mesodermal origin -
the skin itself or dermis.
The epidermis is a stratified squamous keratinizing epithelium. The dermis consists of connective tissue with some elastic and smooth muscle fibers. The latter are collected in bundles and form the muscles that lift the hair. Papillary dermis
, located directly under the epidermis, contains blood and lymphatic capillaries, nerve fibers. The papillae on the surface of the skin correspond to ridges that form a complex individual pattern, which is used in forensic medicine (fingerprinting). Beneath the skin itself is the subcutaneous fat layer.
The horny appendages of the skin are hair and nails.
Hair
consist of a rod and a root. The rod is located above the surface of the skin, the root lies in the skin. The hair root ends in an extension - the hair follicle - and is surrounded by a hair follicle, into the cavity of which the excretory duct of the sebaceous gland opens.
Nail
- This is a horny plate that lies on the dorsal surface of the distal phalanx and protects it from mechanical influences. The nail is divided into the free edge, the root and the nail folds. Nail folds are folds of skin that cover the nail from the sides and at the root. Nail growth begins from its root.
Skin derivatives include sebaceous, sweat and mammary glands. Sebum secreted by the sebaceous glands serves as a lubricant for the hair and epidermis and protects the skin from microorganisms. Sweat glands, together with water, secrete certain metabolic products from the body (urea, salts, uric acid) and participate in thermoregulation.
Mammary gland, mamma
, is a derivative of the sweat glands, located on the fascia of the pectoralis major muscle and extends from the III to VI ribs. There is a nipple on it, surrounded by a pigmented area of skin - the isola. The mammary gland is a complex alveolar-tubular gland, consisting of 15-20 lobules, the excretory ducts of which open at the top of the nipple.
Fascia
The orbit, where the apple is located, is lined with periosteum. In the area of the superior fissure and optic canal, it fuses with the dura mater. The apple is surrounded by the vagina or Tenon's capsule. It connects to the sclera. The gap between the vagina and the surface of the apple is called Tenon's (episcleral) space. Along the posterior surface, the first fuses with the outer cavity of the optic nerve, and in front it approaches the conjunctival fornix. Nerves and vessels, tendons of oculomotor fibers pass through the vagina. In front, the orbit and its contents are partially covered by a septum. It starts from the periosteum of the lower and upper edges and is attached to the cartilage of the eyelids. In the area of the inner canthus, it connects with the medial ligament.
Fat body
Between the periosteum and the apple sheath, around the oculomotor fibers and the optic nerve, there is an accumulation of tissue. It is called the fat body. It is pierced by connective tissue bridges. The fat body performs a shock-absorbing function. Its smaller part is located outside the cone formed by the apple muscle complex. It is adjacent to the walls of the orbit. Most of the body is located inside the cone, surrounded by the nerve.
Accessory apparatus of the eye, its components
The accessory apparatus of the eye is of great importance
The human eye is a delicate, complex and fragile organism that needs protective devices. In order to efficiently perform its functions of ensuring a clear perception of the surrounding world in colors, an auxiliary device is needed.
The protective mechanisms of the eye consist of the eyelids, eyebrows, eyelashes, and conjunctiva. Eyebrows prevent salty sweat from getting into your eyes. Eyelashes are located along the edge of the eyelids; they protect the eyelids from dust and weather conditions. The eyelids consist of lamellar connective tissue, the structure resembles cartilage, they are capable of performing the following functions:
- protect from external damage;
- promote washing the eyes with tear fluid;
- when blinking, the cornea and sclera are cleared of foreign particles;
- help to focus vision;
- help regulate pressure inside the eye;
- reduce the intensity of the light flux.
On the outside there is a thin covering of skin that gathers into folds, under which the eyelid muscle is located. Inside it is covered with a thin tissue structure - the conjunctiva.
The conjunctiva moves from the eyelid to the eye organ, bypassing the cornea. Among the conjunctiva of the eyelid and eye there is a conjunctival sac, where foreign bodies mainly settle. The upper eyelid differs from the lower eyelid by the presence of several folds:
- supra-sulcata;
- sulcinate;
- tarsal.
Protective is the main function of the eyelashes.
The auxiliary devices of the human eye are the lacrimal apparatus and the motor muscles of the eyeball. They are created by nature to control the eye organ and help to functionally carry out its work.
This also includes the fascia of the orbit and the fatty body. The eyeball is placed in the orbit, the bottom of which is covered with a membrane - the vagina - and surrounds the eye. Fascia includes the vagina, tendons, ligaments, and blood vessels.
Around the muscles, the optic nerve, between the periosteum and the vagina, there are fatty partitions, and on the posterior plane of the eye organ there is the substance of the orbit - the fatty body, it is elastic, creates a place for the free position of the visual apparatus.
Eyelids
They are divided into upper and lower. These structures of the accessory apparatus of the eye are folds of skin that run in front of the apple. The eyelids cover it from below and above. When closed, they completely cover the apple. When open, the edges of the eyelids limit the transverse slit. On the lateral and medial sides it is closed by adhesions - adhesions. They form the eye angles. There is a slight elevation in the area of the medial commissure. It is called the lacrimal caruncle. There is a lake around it. Inward from the caruncle there is a vertical small conjunctival fold - the semilunar fold. It is considered a remnant of the third (blinking) eyelid found in vertebrates. On the free edge of the lower and upper eyelids, next to the medial angle, outward from the lake, an elevation is visible - the papilla. At its top there is an opening - the beginning of the lacrimal canaliculus. In the area of the edge of the orbit, the folds of the eyelids pass into the integument of adjacent areas of the face. At the border with the forehead there is a transversely directed ridge, the surface of which is covered with hair. This is an eyebrow. The anterior surface of the eyelids is convex. It is covered with thin skin, where many sweat and sebaceous glands lie. The back part faces the eyeball. It has a concave shape and is covered by the conjunctiva. Everything related to the auxiliary apparatus of the eye is actually protected by the eyelids.
Anatomy of the eye
The eyeball bears this name for a reason, since the organ has an irregular spherical shape.
Its curvature is greater in the direction from front to back. These organs are located on the same plane of the facial part of the skull, close enough to each other to ensure overlapping fields of vision. In the human skull there is a special “seat” for the eyes - the orbits, which protect the organ and serve as an attachment point for the extraocular muscles. The dimensions of the orbit of an adult of normal build are within 4-5 cm in depth, 4 cm in width and 3.5 cm in height. The depth of the eye is determined by these dimensions, as well as the volume of fatty tissue in the orbit.
The front of the eye is protected by the upper and lower eyelids - special folds of skin with a cartilaginous frame. They are instantly ready to close, exhibiting a blink reflex when irritated, touching the cornea, bright light, or gusts of wind. On the front outer edge of the eyelids, eyelashes grow in two rows, and glandular ducts open here.
The plastic anatomy of the eyelid slits can be raised relative to the inner corner of the eye, level, or the outer corner will be lowered. The most common occurrence is a raised outer corner of the eye.
A thin protective membrane begins along the edge of the eyelids. The conjunctival layer covers both eyelids and the eyeball, passing into the corneal epithelium in its posterior part. The function of this membrane is to produce the mucous and aqueous parts of the tear fluid, which lubricates the eye. The conjunctiva has a rich blood supply, and its condition can often be used to judge not only eye diseases, but also the general condition of the body (for example, with liver diseases, it may have a yellowish tint).
Together with the eyelids and conjunctiva, the auxiliary apparatus of the eye consists of the muscles that carry out eye movements (direct and oblique) and the lacrimal apparatus (lacrimal gland and additional small glands). The main gland turns on when there is a need to eliminate an irritating element from the eye and produces tears during an emotional reaction. To permanently wet the eye, tears are produced in small quantities by accessory glands.
Wetting of the eye occurs through blinking movements of the eyelids and soft sliding of the conjunctiva. The tear fluid drains through the space behind the lower eyelid, collects in the lacrimal lake, then in the lacrimal sac outside the orbit. From the latter, fluid is drained through the nasolacrimal duct into the lower nasal passage.
Connective tissue plate
It is located in the thickness of the lower and upper eyelids. In its density, the connective tissue plate is similar to cartilage. It distinguishes between the anterior and posterior surfaces, as well as 2 edges - free and orbital. The posterior surface of the plate fuses tightly with the conjunctiva. This determines the smoothness of the latter in this area. The anterior portion of the eyelid cartilage is connected to the circular muscle fibers by connective tissue. A common ligament runs from the superior and inferior surfaces to the medial wall along the posterior and anterior ridges. It covers the lacrimal sac. The ligament of the same name follows towards the lateral wall.
Free edge
It is limited to the anterior and posterior surfaces of the eyelid. The orbital edges are fixed at the corresponding part of the orbit with the help of muscle fibers of the lower and upper cartilages. The fibers of the latter are attached to the inner surface. They attach to the muscle that lifts the upper eyelid. The inferior muscle connects to the corresponding rectus muscle of the apple. It is attached to the edge of the cartilage of the same name. On the free edge there are hairs - eyelashes.
Conjunctiva
The auxiliary apparatus includes special recesses. They are formed at the junction of the conjunctiva from the lower and upper eyelids to the apple. It, in turn, covers the anterior part and passes to the limbus of the cornea. A ring forms at the junction of the sclera. The entire space extending from the apple in front and limited by the conjunctiva is called the sac. He is closed when his eyes are closed, and when his eyes are open he communicates with the external environment. In the thickness lie single conjunctival glands.
Functions of structures
The structure of the eye and the entire visual system perform important tasks to protect the organs. The lacrimal glands have a cleansing value. Thanks to them, the blinking process takes place and dirt is removed from the visual apparatus. Thus, the body resists infections. Medial and lateral muscle tissues rotate the eye in different directions. The superior straight line is responsible for the upward and outward movement of the organ of vision, and the inferior straight line is responsible for the upward and downward movement of the organ of vision. The protective functions of the auxiliary apparatus of the eye are provided by the conjunctiva: it is sensitive to all irritants. Therefore, with any unwanted touch, the eyelids quickly close. In addition, it blocks the path of allergens, chemicals and infections to the visual apparatus.
Blepharitis
The eye (auxiliary) apparatus, as mentioned above, includes eyelids. When their edges become inflamed, blepharitis is diagnosed. The etiology of the pathology is very diverse. Blepharitis, in particular, can be caused by hypovitaminosis, anemia, helminthic infestations, gastrointestinal disorders, etc. Prerequisites for the occurrence of the disease include pathologies of the lacrimal ducts, chronic conjunctivitis, exposure to smoke and dust. Blepharitis can be ulcerative, scaly, simple, etc. Treatment is prescribed only by a doctor. Maintaining hygiene in living and working conditions is mandatory. For simple blepharitis, 1% brilliant green solution or 1% mercury yellow ointment is prescribed. For peptic ulcers, a compress of fish oil or oil is first applied to the eyes. In case of complex pathology, autohemotherapy and physiotherapy are used.
Dacryocystitis
The auxiliary apparatus of the eye is especially vulnerable in newborns. Dacryocystitis is often diagnosed in infants. It is an inflammation in the lacrimal sac. Dacryocystitis can also be detected in adults. In this case, it is usually chronic. The prerequisites are inflammatory processes in the nasal cavity, paranasal sinuses, and bones that surround the sac. These processes cause the delay and development of pathogenic microbes. In newborns, dacryocystitis is associated with the preservation of the germinal film covering the lower part of the nasolacrimal canal. Therapy is carried out surgically. In the acute course of the pathology, anti-inflammatory drugs are prescribed. After suppression of inflammatory processes, surgery is performed.
↑ 1. The concept of “norm”, variation and anomaly in relation to the human body
The concept of “normal” is so capacious that one might almost consider it completely meaningless.
An example of replacing the concept of “average value” with the concept of “norm” is Gesell’s “ Table of Normal Physical Development of an Infant
«.
No doubt, this table is of interest to scientists and pediatricians. But we must not forget that it shows the average statistical indicators of child development. The result of this substitution of concepts is the anxiety of thousands of mothers, concerned that their children begin to drink from a cup or take their first steps later than they should according to the table. Obviously, having established an average value, we must then ask the question: “Should the average be considered as useful, desirable for a person?”
Too often, when we talk about “the norm,” we mean following traditions and conventional behavior. We use the word “normal” to express approval of the usual course of things. I remember how much talk, how much noise the issue of women’s smoking caused at one time.
Adaptation means blind submission to stereotypes and demands of society and environment. But what if this is a sick society, what if this is an unhealthy environment?
We are only now beginning to understand that juvenile delinquents are not necessarily bad, vicious, or psychiatrically unhealthy. Juvenile crime and delinquency are often a reaction to exploitation and social injustice; a child, by committing an offense, thereby asserts his legitimate biological right to justice.
Adaptation is a passive process; in the process of adaptation, a person does not need his individuality, his desires, his will, sometimes they simply interfere with adaptation. In this sense, we find ideal adaptability in a ram in a herd or in a slave, that is, in those creatures who do not know what free will is. Even a lunatic or insane person can be called an ideally adjusted person.
In its extreme forms, the theory of the “decisive influence of the environment” implies the absolute immutability of the environment and the unlimited malleability of human nature. Environmentalism is a philosophy of fatalism, a philosophy of the status quo that does not reflect the true state of affairs. Human nature is changeable, but not infinitely; the environment, on the contrary, is infinitely changeable.
A completely different tradition of defining the norm has developed in medicine, where the concept “normal” is used as a synonym for physical health, as a synonym for the absence of organic lesions and dysfunctions. If a patient complains, for example, of stomach pain, but during the prescribed examination no signs of a physical illness are found in him, then nine out of ten young doctors will tell the patient that “everything is fine” with him, even if he continues to be in pain. What they should really say is, “The methods at my disposal do not allow me to determine what is causing the pain.”
Only a very experienced doctor or a doctor with some psychological training is able to suggest that a psychological illness is hidden behind physical pain; You don’t hear the notorious “everything is fine” from him very often. Indeed, many psychoanalysts claim that no people are absolutely normal or absolutely healthy. In essence, their statement is somewhat reminiscent of the saying: “He who is not without sin,” which is difficult to argue with, but even if we agree with it, we will not be a millimeter closer to the desired moral ideal.
Let us now assume that crises are a necessary prerequisite for the emergence of new theories, and then let us see how scientists react to their existence. A partial answer, as obvious as it is important, can be obtained by first considering what scientists never do when faced with even strong and long-lasting anomalies. Although they may gradually lose confidence in previous theories from that point on and then think about alternatives to overcome the crisis, they never easily give up the paradigm that plunged them into the crisis.
In other words, they do not consider anomalies as counterexamples, although in the lexicon of the philosophy of science they are precisely that. In part, this generalization of ours is simply a statement of historical fact, based on examples similar to those given above and more extensive ones set out below. To some extent, this suggests something that our further exploration of paradigm rejection will reveal more fully: having once achieved the status of a paradigm, a scientific theory is declared invalid only if an alternative is suitable to take its place.
There is not yet a single process revealed by the study of the history of scientific development, which as a whole would resemble the methodological stereotype of refuting a theory through its direct comparison with nature. This statement does not mean that scientists do not reject scientific theories or that experience and experiment are not important in such a process of refutation. But this means (this point will ultimately be the central point) that the judgment that leads a scientist to abandon a previously accepted theory is always based on something more than a comparison of the theory with the world around us. The decision to abandon a paradigm is always simultaneously a decision to accept another paradigm, and the judgment leading to such a decision involves both a comparison of both paradigms with nature and a comparison of the paradigms with each other. If during the intrauterine life of the fetus, as a result of any reason, the formation of the nose is disrupted, then deformity occurs. The earlier a violation of the embryonic development of an organ occurs, the more severe the deformity. The degree of severity of the changes determines the concept of deformity, anomaly and variation: the more pronounced the developmental defect, the more rightly it should be classified as a deformity; weak degrees of disfigurement should be considered anomalies, and underdeveloped deviations – variations.
Systematic anatomy studies the structure of the “ normal”
”, i.e. a healthy person whose tissues and organs are not changed as a result of illness or developmental disorder. In this regard, normal (from the Latin normalis - normal, correct) can be considered a human structure that ensures the functions of a healthy body. At the same time, normal indicators for a larger or smaller number of people (weight, height, body shape, structural features, etc.) will always be in the range of maximum and minimum values due to individual structural features. The latter are determined by both hereditary factors and environmental factors.
The relationship between the body of a healthy person and the external environment under normal (physiological) conditions is in a state of equilibrium. According to the definition of G.I. Tsaregorodtsev, “a norm is a special form of adaptation to environmental conditions, which ensures ... optimal vital activity for the body.” Recently, the term “conditional norm” has been often used, which recognizes the relativity of this concept.
The presence of individual variability in the shape and structure of the human body allows us to talk about variants (variations) of the structure of the body (from the Latin variatio - change, varians - option), which are expressed in the form of deviations from the most common cases, accepted as the norm. The most pronounced persistent congenital deviations from the norm are called anomalies (from the Greek anomalia - irregularity). Some anomalies do not change a person’s appearance (right-sided position of the heart, all or part of the internal organs), others are pronounced and have external manifestations.
Such developmental anomalies are called deformities (underdevelopment of the skull, limbs, etc.). The science of teratology studies deformity (from the Greek teras, gender teratos - freak). The structure of the human body by region, taking into account the position of the organs and their relationships with each other and with the skeleton, is the subject of the study of topographic (surgical) anatomy.
Conjunctivitis
Protecting the organs of vision is the main task performed by the eye apparatus. The auxiliary department is constantly exposed to external influences. Conjunctivitis is one of the most common pathologies of the organ of vision. It is an inflammation in the connective membrane. Adenoviral conjunctivitis is spread by airborne droplets. Pathology develops sporadically, in the form of epidemic outbreaks. Most often it occurs in children's groups. The onset of the pathology is acute. Before eye damage, respiratory tract diseases usually occur, the temperature rises, and the pre-auricular lymph nodes enlarge. Conjunctivitis is accompanied by photophobia, lacrimation, redness and swelling of the eyelids, and hyperemia. Follicles or films often appear. The latter are detected, as a rule, in children.
Acute phase
The causative agents of the pathology are staphylo-, strepto-, gono-, pneumococci, Koch-Wicks bacillus, etc. Typically, exogenous damage to the conjunctiva develops. Autoinfection is also possible. The prerequisites are hypothermia or overheating of the body, microtrauma of the conjunctiva. The disease caused by Koch-Wicks bacillus is spread through dirty hands and contaminated objects. In the summer, epidemics often break out in countries with hot climates.
Chronic course
It is caused by prolonged irritation of the conjunctiva. The disease becomes chronic if the organ of vision is constantly exposed to chemical impurities, smoke, dust, etc. Vitamin deficiency, metabolic disorders, ametropia, and persistent damage to the lacrimal ducts and nose may also be prerequisites. Chronic conjunctivitis is manifested by a burning sensation, a feeling of sand in the eyes, hyperemia, and mild swelling. Scanty mucopurulent discharge is also observed. During treatment, first of all, favorable hygienic conditions are created. All negative factors that can cause pathology are eliminated. As a rule, local drugs are prescribed in the form of drops. This could be, for example, 025-033% zinc sulfate solution, supplemented with adrenaline and dicaine. If an exacerbation is noted, 30% sulfacyl sodium solution, 10% sulfapyridazine sodium solution and 0.3% syntomycin solution are prescribed.