Preventive measures, prognosis
It is unlikely that retinal detachment can be prevented. But reducing the risk of relapse is easy if you follow simple rules:
- Monitor blood pressure readings.
- Try not to take hormones.
- Avoid overexertion.
- Perform gymnastics to relax your eyes.
People over 30 and those who are prone to chorioretinopathy should be regularly examined by an ophthalmologist; if a distorted image of objects appears, they should not wait until vision recovers on its own. The effectiveness of preventive examinations is confirmed by participants in thematic forums, who describe the features of the course of the disease and leave feedback on treatment.
Angioprotector, reduces the permeability of the vascular wall
Symptoms
The clinical picture of the disease largely depends on the severity of the thrombotic process in the retinal vein. In this regard, there may be 2 types of pathology:
- Ischemic thrombosis. Severe bleeding into the retina occurs, and damage to the blood flow leads to a decrease in visual acuity and the development of serious ophthalmological disorders;
- Non-ischemic or incomplete occlusion. Damage to the retina and blood vessels is much less pronounced, there are no profuse hemorrhages, and visual acuity may remain intact.
The disease often develops rapidly, with critical condition occurring within a few hours after the onset of thrombosis. First, general malaise and weakness, painful sensations in one or both eyes occur, and only then characteristic visual disturbances are added - fog or spots before the eyes, distortion of the perception of objects. If the hemorrhages do not affect the central part of the retina, then visual acuity may remain unchanged for some time, but then gradually decrease.
Usually, 1-2 months after thrombosis, vision begins to return to normal, but complete recovery is extremely rare. Even after a full course of therapy, maculopathy and tissue degeneration are possible, as well as a general thinning of blood vessels, which can lead to their rupture. Every 5 patients with thrombosis subsequently develop glaucoma.
International code
ICD 10 is the international classification of diseases, a short adapted version of the 10th revision, adopted at the 43rd World Health Assembly. Varicose veins according to ICD 10 code consists of three volumes with encodings, transcripts and an alphabetical index of diseases. Deep vein thrombosis has a specific code in the ICD-10 classification - I80. It is characterized as a disease with inflammation of the walls of the veins, disruption of normal blood circulation and the formation of blood clots in the venous lumens. Such an acute inflammatory process of the lower extremities is dangerous for human life, and ignoring it can lead to death.
The main factors that can provoke deep vein thrombophlebitis are:
- Infectious pathogens;
- Injuries and damage to tissues and bones;
- Impaired tissue nutrition and development of aseptic inflammation;
- Introduction of a chemical irritant into the vessels of the lower extremities;
- Long-term use of hormonal drugs or pregnancy;
- Increased blood clotting.
Read also: Chronic thrombophlebitis
With diseases such as vasculitis, periarthritis or Bruger's disease, the risk of thrombosis of the veins of the lower extremities increases by approximately 40%. Vascular disease can be triggered by addiction to smoking and alcoholic beverages, problems with the cardiovascular system, as well as excess weight, which leads to obesity.
At the initial stages of development, disease of the vessels and deep veins of the lower extremities can occur without the appearance of any symptoms. But soon the following signs appear:
- swelling of the lower extremities occurs. Moreover, the higher the area of inflammation is located, the more pronounced the edematous process;
- painful sensations of a pulling and bursting nature;
- the skin becomes very sensitive and reacts to any pressure. In the place where vascular thrombosis has formed, it becomes warmer and acquires a reddish tint. Often the surface of the lower extremities acquires the cyanosis characteristic of the disease;
- itching and burning;
- the venous system becomes more expressive and changes its structure.
Sometimes an infection is added to the inflammatory process, which can lead to an abscess and purulent discharge.
Thrombophlebitis has several forms: acute and chronic. With acute manifestations of inflammation of the deep veins and vessels of the lower extremities, severe swelling and unbearable pain appear without any reason. It is quite difficult to completely get rid of the disease, and most often this is the cause of chronic venous insufficiency. Chronic inflammation is very often accompanied by the formation of pustules and abscesses.
Separately, mesenteric and ileofemoral thrombophlebitis are distinguished:
- mesenteric thrombosis is characterized by an acute disturbance of the blood flow of the mesenteric vessels, which forms against the background of embolism. The cause of mesenteric thrombus formation is heart disease, for example, myocardial infarction, cardiosclerosis, rhythm disturbance;
- Ileofemoral thrombophlebitis is a rather complex disease that appears against the background of thrombotic clots blocking the femoral and iliac vessels. The acute inflammatory process passes quite quickly as a result of compression of the arteries of the lower extremities and can lead to the formation of gangrene. The most dangerous complication may be the rupture of the embolus and its transfer to the vessels of the lung and parts of the heart, arterial thrombophlebitis.
Why does the disease occur?
A reliable fact is that central vein thrombosis does not develop independently. The following body pathologies associated with blood clotting may be accompanied: diabetes mellitus, atherosclerosis, thrombophlibia, hyperonia, systemic vaculitis and other blood diseases.
The main cause of the disease is formed as follows: the listed diseases thicken the walls of the artery, thereby putting pressure on the adjacent veins. Accordingly, blood flow is disrupted and clots form.
Clots prevent blood from moving further and provoke a reverse flow of blood, increasing pressure, which leads to hemorrhage in the retina and the appearance of edema.
A special feature is that it is asymptomatic; in a patient with central vein thrombosis, visual acuity slowly deteriorates, but it is practically impossible to track this. Sometimes it decreases gradually over several days or months; in these cases, patients complain of fogging, veil, and distortion of objects. If the macula is not involved in the process, then there may be no complaints. Visual acuity ranges from counting fingers to 1.0.
Associated factors that increase the risk of developing ocular vascular thrombosis
- Infection.
- Intraocular tumor-like formations. The formation of thrombosis is especially affected by the presence of an optic nerve tumor.
- Ophthalmic hypertension. IOP is often asymptomatic, which reduces the chance of diagnosing the pathology in a timely manner.
- Endocrine disruptions in the body.
- Alcohol abuse, smoking. A bad habit has a detrimental effect on the body's circulatory system.
- Inactivity, weight gain.
- Diseases of the soft tissues of the eye (orbitopathy).
The classification of the disease divides it into ischemic (complete occlusion) and non-ischemic (partial occlusion) types of thrombosis.
Types of retinal thrombosis
Incomplete occlusion
Characterized by a small area, there are no signs of a hemorrhagic rupture in the retinal area, visual functions are partially deteriorated, the symptoms are practically not noticeable. While at home, the patient may not notice minor visual impairment. And if minor discomfort occurs, most often patients do not go to the doctor, trying to be treated with folk remedies.
Complete occlusion
The degree and nature of thrombosis damage increases, covering most of the blood vessels. The patient's vision deteriorates sharply due to extensive hemorrhage in the retina. Upon admission, the patient complains of a sharp deterioration in vision, which occurs as a result of extensive hemorrhage in the retina due to burst thrombophlebitis. With complete occlusion, the likelihood of complications increases.
Causes
The disease occurs due to pathological changes in the functioning of the walls of blood vessels or a violation of blood viscosity. As a rule, this occurs due to the fact that dilated arteries in some functional or ophthalmological diseases begin to compress nearby veins, thereby disrupting the natural outflow of blood. Similar problems are most often observed with the following ailments:
- Arteriosclerosis;
- Diabetes mellitus of any type;
- Blood pressure disorders;
- Diseases accompanied by changes in blood clotting;
- Ophthalmological pathologies in which intraocular pressure increases, for example, glaucoma.
In most cases, retinal vein thrombosis is diagnosed in elderly people over the age of 65 years. In addition, it is in this group that bilateral lesions occur in every 10 cases. The disease can also develop at a young age, usually as complications after acute infectious diseases or severe inflammation of the nasopharynx.
It is believed that the risk of pathology increases in people who lead a sedentary lifestyle, suffer from obesity and disruption of the endocrine system.
Methods for diagnosing and treating a blood clot in the eye
If you detect the slightest sign of a blood clot in the eye, it is very important to immediately contact an ophthalmologist. The thing is that even with complete thrombosis of a vein in the eye, if blood flow can be restored within an hour, a decrease in visual acuity, and in some cases, complete blindness can be avoided
In addition to interviewing the patient and collecting anamnesis to identify the characteristics of circulatory disorders of the eye, the following studies can be carried out:
- visometry;
- perimetry;
- biomicroscopy;
- ophthalmoscopy;
- angiography;
- retinal tomography;
- blood pressure measurement;
- ECG;
- general blood and urine tests.
In addition to consulting an ophthalmologist, you may need to visit a cardiologist, neurologist, endocrinologist and other highly specialized doctors.
In cases where incomplete thrombosis occurs, drug treatment has a good effect. Medicines used to treat a blood clot include:
- antiplatelet agents;
- angioprotectors;
- antihypertensive drugs;
- hormonal agents;
- antispasmodics;
- fibrolytics;
- vitamin complexes.
Even if treatment was carried out in a timely manner, blood clots do not go away without a trace, so after a few months laser coagulation of the retina is performed.
Vascular thrombosis of the eye is a condition characterized by the formation of blockage of the central retinal vessel or its branches. As a result, blood circulation is disrupted and stagnation begins. Retinal thrombosis is currently one of the causes of progressive vision loss. In most cases, the disease affects older people, but the pathology can develop at any age.
Factors of occurrence
The causes that provoke the development of the disease (ICD code 10 I 80) are divided into 3 factors:
- Thickening of the blood due to changes in its composition.
- Reducing the speed of blood flow.
- Damage to the inner lining of blood vessels.
Read also: Medicine for deep vein thrombophlebitis
These factors are diagnosed individually or in combination. They contribute to the development of varicose veins, which is the cause of acute thrombophlebitis.
Vein thrombosis is a rather dangerous disease that can be fatal if a blood clot breaks off and enters the arteries of the lung or heart.
Thrombophlebitis (ICD code 10 I80) develops with forced immobility of a limb (with a fracture).
Thrombosis of the veins of the lower extremities is caused by taking estrogen-containing hormones prescribed for infectious and autoimmune diseases. Oncological diseases provoke thrombophlebitis of the lower extremities. Installation and long-term presence of a catheter in the venous bed and frequent injury to the walls by injections lead to the formation of blood clots.
In 65% of cases, thrombophlebitis is diagnosed in women. The pattern is associated with wearing high-heeled shoes, tight jeans and taking hormonal contraceptives. The cause of the disease may be pregnancy. During this period, physiological activation of coagulation processes occurs, preventing bleeding in the postpartum period, and the inflamed vessel wall leads to the formation of a blood clot. People aged 40-55 years are at risk. At this age, the condition of the body's vascular system deteriorates significantly.
Thrombosis is hereditary. Causative factors include obesity, unbalanced diet, physical activity, smoking and drinking alcoholic beverages.
Deep vein thrombosis has a specific code in the ICD-10 classification – I80
Characteristic symptoms
The main problem in diagnosing vein thrombosis is that the pathology is extremely difficult to identify. The disease has minor clinical manifestations in the early stages, which many patients do not pay attention to.
Moreover, middle-aged and elderly people often already have poor vision and may attribute the symptoms of eye vein disease to age-related changes.
A distinctive feature of thrombosis is that the lesion is unilateral. In other words, the pathology occurs in one eye and does not spread to the second.
Another key feature of the disease is that the main clinical signs develop at night, with the most striking symptoms appearing immediately after waking up.
Symptoms:
- Slow blood circulation, the beginning of vein deformation;
- Pinpoint hemorrhages;
- Development of bloody forms along the entire length of the retina;
- Swelling of the optic nerve area;
- Redness;
- In places of vascular necrosis, pathogenic changes occur, obscuring the visual zones and forming blind spots;
- Flashing of midges before the eyes.
With thrombosis, tortuous veins often burrow into the retina and cause swelling. If the disease is partial, the number of hemorrhages will be less.
If thrombosis affects entire branches of the veins, then the spectrum of damage is much larger, which leads to the development of white foci - accumulations of protein on the surface of the retina. The result of disease damage can be late complications.
Classification of the disease
ICD 10 code I80 includes phlebitis and thrombophlebitis. Symptoms vary depending on the location of the clot. There are 2 types of diseases:
Superficial thrombophlebitis develops in the great saphenous vein. It is easy to diagnose. Inflammatory changes occur in the area of the affected vessel, but if varicose veins are not observed, then thrombophlebitis is interpreted by ICD 10 as a complication of gynecological pathology or a symptom of a malignant tumor in the organs of the digestive system. Thrombophlebitis ICD 10 also includes thrombosis in the intestine.
When palpating the inflamed saphenous vein, the patient experiences stabbing pain. Symptoms of superficial thrombophlebitis: scarlet stripes on the skin, swelling of the ankles and feet, increased body temperature.
Without treatment, thrombosis spreads to the deep veins. The patient's health worsens. Infiltration and hyperemia are observed in the area of the thrombosed vessel.
There are 2 types of thrombosis that require special attention:
- Ileofemoral thrombosis is a subtype of deep vein thrombophlebitis. The disease affects large vessels in the femoral and iliac veins. If blocked, it can be fatal. Ileofemoral thrombosis develops rapidly. The patient develops severe swelling of the lower extremities. High body temperature is added to the symptoms. The skin acquires a bluish tint. Complete blockage can lead to the development of gangrene.
Such an acute inflammatory process of the lower extremities is dangerous for human life, and ignoring it can lead to death
- Mesenteric vascular thrombosis is a blockage of the mesentery or mesentery. Without treatment, thrombosis of the mesenteric vessels leads to the death of the affected area. Mesenteric thrombosis (code K55 in ICD 10) requires immediate surgical intervention.
Thrombosis of the lower extremities according to the clinical picture is classified into:
- Spicy. Symptoms of the acute form appear suddenly. The patient experiences muscle pain along the thrombosed vessel. Acute thrombosis is accompanied by elevated body temperature. Red stripes appear on the skin. Deep vein thrombophlebitis differs from superficial thrombophlebitis in severe swelling, heaviness in the legs and bluish skin. The pain intensifies, causing lameness.
- Chronic. With this form, blood clots may dissolve or enlarge. Chronic deep vein thrombophlebitis has a sluggish nature. The patient may experience pain only upon palpation.
The main factors that can provoke deep vein thrombophlebitis are: tissue nutritional disorders and the development of aseptic inflammation
When the inferior vena cava is blocked, bilateral swelling of the limb is observed. If the thrombus is located in the iliac segment, then unilateral edema is noted. When walking for a long time, aching pain appears in the calf muscle.
Thrombosis is manifested by numbness of the limbs, loss of sensitivity, tingling of the skin, chills and hardening of the lymph nodes. The first symptoms of the chronic form may appear a year after the exacerbation. The disease can be migratory in nature. This form is characterized by rapid development. The migratory form affects the superficial veins. Dense thrombosed nodules can change their position, appearing in different parts of the limb. Seals are accompanied by swelling and increased body temperature.
For thrombophlebitis, doctors prescribe treatment based on the diagnostic results obtained. Treatment includes:
- drug therapy;
- surgical intervention.
Thrombophlebitis has several forms: acute and chronic
If thrombosis affects the superficial veins, then treatment is carried out with medication. The patient is prescribed phlebotonics, anti-inflammatory drugs, ointments. Conservative treatment relieves swelling, reduces pain and restores blood flow. Anti-inflammatory drugs include drugs such as Ibuprofen, Aspirin and Diclofenac. Heparin ointment and Troxevasin have a local effect.
For thrombosis of superficial veins, doctors prescribe electrophoresis with anticoagulants, UHF therapy and magnetic therapy. Physiotherapeutic procedures dissolve blood clots and reduce swelling and pain.
Conservative treatment is carried out in combination with compression therapy. For thrombophlebitis, elastic bandages and compression stockings (stockings or tights) should be worn. The degree and class of compression is prescribed by a phlebologist depending on the severity of the disease.
Read also: Nutrition for thrombophlebitis
For superficial thrombophlebitis, treatment with folk remedies is effective. Verbena leaves will help eliminate swelling, heaviness and relieve pain in the legs. Pour 20 g of leaves into 200 ml of boiling water. Take the drink 100 ml 3 times a day during the day.
Deep vein thrombosis of the lower extremities requires a radical method of treatment. Depending on the stage and nature of the disease, the method of surgical intervention is selected. The endoscopic procedure is a low-traumatic method of treatment. During the procedure, the vessel is “sealed” above the site of phlebitis. In modern medicine, radiofrequency obliteration and laser coagulation are used. Minimally invasive methods do not cause complications and are carried out even during pregnancy. Due to the low-traumatic nature of the operations, the rehabilitation period is minimal. As the disease progresses, the thrombosed vessel is completely removed. In case of deep venous thrombosis, elastic compression is prohibited. Bandaging leads to the development of complications.
Main signs of the disease
This pathology is characterized by the fact that its manifestations become noticeable only at the stage when the processes of retinal destruction reach a certain level.
At first, patients do not complain of blurred vision, although this is the most important symptom of the disease. Sometimes patients note a distortion in the visibility of objects, some blurring of vision. But if the macula area is not involved in the pathological process, patients are not bothered by these signs.
The process of gradual deterioration of vision can last a very long time - from several months to several years. However, even over this long period of time, a person’s vision can remain relatively high.
The danger of the pathology is that a person does not pay attention to the dangerous signs of decreased vision. After all, often incomplete thrombosis may not bother a person and may not manifest itself as noticeable disturbances in visual function.
How is acute thrombosis detected?
We use the following diagnostic methods:
- Phlebography is one of the most accurate methods for diagnosing deep vein thrombosis.
- Vascular ultrasound.
- Radionuclide scanning and other new methods for detecting thrombosis.
After making an accurate diagnosis and a comprehensive study of thrombosis parameters, the attending phlebologist prescribes a course of treatment taking into account the individual characteristics of the patient.
Patients with this diagnosis require treatment in a hospital setting. The patient can only be transported to the hospital in a horizontal position on a stretcher. The patient is prescribed bed rest until the process of blood clots has stabilized and laboratory confirmation of a decrease in blood clotting. After this, active movements are gradually restored, but a compressive bandage with an elastic bandage must be applied. Prolonged bed rest is contraindicated.
Conservative therapy is carried out using drugs that can reduce blood clotting - anticoagulants are prescribed for this purpose. It is also necessary to use drugs to prevent platelet aggregation - disaggregants. The implementation of thrombolytic therapy is possible only in the first 6 hours after the onset of the disease. It should not be performed without installing a cava filter in the inferior vena cava. The fact is that there is a risk of embolus formation, which will lead to the development of complications. Surgical therapy is indicated when there is a high probability of pulmonary embolism.
For this purpose, the following activities are carried out:
- installation of a cava filter in the inferior vena cava just below the connection of the renal veins;
- dismemberment of the inferior vena cava with sutures, the formation of several channels - is carried out if it is impossible to install a cava filter;
- injection of the streptase enzyme is carried out through a catheter directly to the blood clot;
- blood clot removal – used for blue phlegmasia and lack of effect from conservative treatment.
Reasons for development
This pathological condition develops as a consequence of various health problems of the patient.
There is a division of the most common causes according to the patient’s age:
| Age | Causes |
| Elderly |
|
| Young people |
|
| All age categories |
|
Factors that provoke the development of the disease are also identified:
- Increased body weight.
- Passive lifestyle.
- Alcohol abuse.
- Lack of vitamins in the body.
These factors are not capable of independently triggering the development of thrombosis, but their combination increases the likelihood of its occurrence several times. This disease affects women and men equally.
Preventive measures
You can prevent the development of central retinal vein thrombosis if you take into account the following tips:
- Stop smoking and drinking alcohol.
- Adjust your daily diet so that your body receives enough nutrients.
- Don't forget about daily physical activity.
- Perform eye exercises aimed at developing the ciliary muscle.
- Monitor your blood pressure.
Another step towards reducing the risk of retinal vein thrombosis is timely treatment of cardiovascular diseases and periodic visits to an ophthalmologist.
Clinical picture
Thrombosis develops gradually. With partial occlusion, a person does not notice any bright signs, the change in vision is minimal. The disease is often diagnosed accidentally during an examination by a doctor.
A sick person may experience:
- Slight decrease in visual function.
- Peripheral hemorrhages.
- Pallor of the arteries.
- Areas of excess blood are difficult to discern.
The ischemic form of thrombosis is characterized by the presence of more pronounced symptoms:
- Massive hemorrhages.
- Severe swelling.
- Excess blood accumulation is very noticeable.
- Noticeable loss of vision.
- Poor reaction of the pupils to light.
- Marked narrowing of the ophthalmic artery.
There are several stages of thrombosis. Each of them is characterized by the development of different symptoms.
Stages:
- The first stage is called prethrombosis. At this stage, venous blood stagnates. The veins become wider, darken, and tortuosity of the vessels appears. The center of the retina becomes swollen. At the first stage, a person may experience blurred vision; this phenomenon is not perceived as a symptom of the disease.
- The second stage is thrombosis. It is characterized by serious circulatory disorders, the occurrence of hemorrhages in the retina and other parts of the eyeball. The boundaries of the optic nerve are poorly visible or not visible at all. Macular edema is present and visual function is severely impaired. The patient notes the presence of a veil before the eyes, loss of visual boundaries. In the absence of adequate treatment, complete or incomplete thrombosis develops, and pathological changes in the retina are noted.
- Postthrombotic retinopathy is the third stage of the disease. The return of a person's vision occurs at a slow pace. Unnatural capillary formations are diagnosed. There are residual hemorrhages in the fundus. During the recovery period, new blood vessels may form in places where they should not be.
Unfortunately, relapse of the disease is possible in the absence of proper treatment.
How to get rid of thrombosis of the central veins of the retina and what is the ICD 10 code for the disease
The vascular network permeates the entire human body and brings blood to every cell. Vascular pathologies can occur in any organ and lead to characteristic consequences and disruptions in its functioning.
The organs of vision are no exception. A condition called thrombosis most often occurs in the veins of the lower extremities, but in some cases it affects the central retinal vein. What needs to be done to preserve vision and how to suspect pathology in time?
Epidemiology
Thrombosis of the central veins of the retina occurs in approximately 2 people out of 1000. The disease mainly affects people over 40 years of age, which is explained by age-related changes and other causes of this pathology.
Central retinal vein thrombosis is more common in people with glaucoma. With age, the incidence rate increases even more.
According to studies, it was found that most people with this disorder developed extraocular vascular problems.
In approximately 18% of patients with blocked veins in the eye, after some time the other eye was also affected. In this case, the problem can occur in both veins and arteries.
Scheme of step-by-step patient management
Many diseases in ophthalmology are accompanied by similar symptoms, so additional examinations are necessary to make an accurate diagnosis.
The development of the disease from the first symptoms to the receipt of a doctor’s conclusion goes through the following stages:
- A condition of prethrombosis , in which people often do not go to the doctor. The patient's vision is practically unimpaired, with only periodic blurring or decreased sharpness possible. During an instrumental examination during this period, visual acuity can be recorded within 0.6-1.0, and also reveal a slight dilation of the veins and their tortuous structure. The results of ophthalmoscopy show minor hemorrhages and slight swelling.
- In the absence of adequate treatment, thrombosis of the central retinal vein develops . The patient experiences a veil before the eyes, a decrease in visual acuity to 0.2-0.6 and minor painful sensations. An ophthalmoscopic examination reveals unclear boundaries of the optic disc, tense and dilated veins, edema and exudative deposits.
After identifying central vein thrombosis, the condition of the branches and the presence of blood clots in smaller vessels are determined. The consequence of blockage may be ischemia of the affected area, which also has important diagnostic significance.
With non-ischemic thrombosis, the prognosis for the patient is more favorable. At this stage, the doctor must examine the patient’s visual system in detail to confirm the diagnosis and determine the type of thrombosis.
For this purpose, ophthalmoscopy and fluorescein angiography of the fundus are used.
- The last stage is postthrombotic retinopathy, which can develop within a few months after the circulatory disorder. At this stage, ophthalmoscopy detects hemorrhages, aneurysms, edema and other pathologies.
At this stage, the doctor must make a differential diagnosis and exclude vision pathologies caused by diabetes mellitus and other non-ophthalmological causes.
Classification
Thrombosis of branched vessels or central retinal vein is classified according to the following criteria:
- localization - the thrombus is located in the central vein or its branches;
- etiology – inflammatory or other;
- stage – prethrombosis, thrombosis, postthrombotic retinopathy, recurrent thrombus formation;
- type – non-ischemic pathology or ischemic;
- condition of the macula - edematous or not.
According to the international classification (ICD 10), this disease is listed under code H 34.8.
Etiology and pathogenesis
The formation of a blood clot in the vessels of the eye can occur for various reasons. The main provoking factors can be divided into:
- systemic – atherosclerosis, increased blood pressure, diabetes mellitus, previous infectious diseases;
- local – inflammatory processes in the retina, age-related changes in the organs of vision, glaucoma.
After the action of a provoking factor in the retinal vein system, blood flow slows down and an inflammatory process occurs. This leads to blood thickening and the formation of blood clots.
Symptoms
Symptoms of retinal vessel thrombosis may be similar to other diseases of the visual system. To make an accurate diagnosis, a more detailed examination of the patient using instrumental methods will be required.
Clinical signs depend on the stage of development of the pathology:
- Prethrombosis . This is the stage at which structural changes are already occurring, but are still poorly felt by the patient. There are no specific complaints, and the diagnosis is often made during a random eye examination. The field of vision and acuity are practically unchanged.
- Thrombosis. The patient experiences an unpleasant haze before his eyes and visual acuity noticeably decreases. The quality of life deteriorates and forces you to see a doctor. An ophthalmoscopic examination reveals hemorrhages and structural changes in the veins.
- If the blood clot affects a branch of the central vein , the patient begins to see objects distorted, and his vision deteriorates gradually over several months.
- Chronic blockage of blood vessels leads to changes in retinal trophism and retinopathy. When examining the fundus, areas of hemorrhage, macular edema, and aneurysms are revealed. In the presence of ischemia, edema is more pronounced, and hemorrhages are detected mainly in the posterior pole of the eye.
Establishing diagnosis
Assuming thrombosis of the central retinal vein, the doctor will ask the patient about the patient’s medical history, lifestyle, and also prescribe an ophthalmoscopic examination. Based on its results, making a diagnosis will not be difficult. Additionally, fluorescein angiography may be prescribed.
General principles of treatment
Treatment of central retinal vein thrombosis is aimed at:
- restoration of blood flow in the affected area;
- decreased pressure in the affected vein;
- restoration of metabolic processes and tissue nutrition;
- eliminating the root cause;
- prevention of complications.
In most cases, surgical treatment with laser is recommended. In parallel with this, maintenance drug therapy can be carried out.
- At the prethrombosis stage, anti-inflammatory drugs , anticoagulants, and artificial tear preparations are prescribed.
- At the thrombosis stage, diuretics, enzyme preparations , vitamins and anti-inflammatory drugs are used. If ischemia is observed in the affected area, laser coagulation and ultraviolet irradiation may be used.
- For retinopathy, peripheral vasodilators and anti-inflammatory drugs are prescribed.
The disease is progressive in nature, so it is not possible to talk about a successful outcome of conservative treatment. Doctors often recommend laser surgery. The earlier therapy is started, the better the result can be expected.
To receive quality medical care, it is better to be treated in a specialized ophthalmology clinic. There, the patient will undergo a complete diagnosis, determine the degree of neglect of the pathology, and prescribe the correct treatment regimen.
Complications and side effects of treatment
Modern treatment methods, such as laser coagulation, are highly effective and rarely lead to complications. In some cases, the patient may experience allergic reactions to concomitant medications, form a cyst after surgery, or develop macular edema.
Errors and unreasonable assignments
Symptoms of retinal thrombosis are similar to complications of other diseases, such as diabetes. If the patient is not fully diagnosed, the doctor may mistakenly assume a different diagnosis, taking into account some features of the medical history. In this case, unreasonable prescriptions may be made, which will lead to the progression of the pathology and a worsening prognosis.
Forecast
With early diagnosis and uncomplicated course, the prognosis is favorable. With medication it is possible to stop the progression of the pathology and achieve resorption of the blood clot. In other cases, thrombosis of the central retinal vein leads to complications, including optic nerve atrophy, glaucoma and others.
Vascular diseases occupy a leading place in the world in terms of prevalence. Problems can occur in any part of the body and always involve dysfunction of the affected organ. Find out from our other articles recommendations for varicose veins of the legs, as well as how to remove veins on the legs without surgery
Source: https://varikoza.guru/tromboz/tsentralnoj-veny-setchatki.html
Treatment of the disease
After making a final diagnosis, the doctor prescribes a treatment regimen suitable for the individual patient. As a rule, it requires hospital stay under constant medical supervision. If treatment is carried out promptly and correctly, the patient can be completely relieved of the symptoms of the pathology and restored to his original vision.
Surgical intervention is required only in advanced cases, when irreversible changes are observed and there is a risk of complete loss of vision. Often, thrombosis of the central retinal vein is treated with conservative methods. These include taking medications in the form of tablets, intravenous injections through a drip, etc.
First of all, fibrinolytics are prescribed. These are medications that destroy fibrin, a protein involved in the formation of a blood clot. As a result of the effects of these drugs, blood flow is restored, and the symptoms gradually decrease in intensity. Most often from this group Fibrinolysin and Plasminogen are prescribed. These drugs are injected daily into the area under the eye for two weeks.
The doctor also prescribes antihypertensive drugs that lower blood pressure and help eliminate swelling. These drugs can be in different forms - in the form of tablets (Nifedipine, Phenigidine), intramuscular injections (Lasix), intravenous injections (Papaverine, Dibazol) or drops (Arutimol, Glautam and Okumed). These drugs are most effective in the presence of hypertension or ocular hypertension.
After completing the course of fibrinolytics, anticoagulants can be prescribed - drugs that prevent pathological blood clotting and the formation of blood clots. The treatment course with these drugs should not exceed a week. The main representative of anticoagulants used in the occurrence of thrombosis of various localizations is Heparin. It can be used in the form of injections or tablets.
If the root causes of the disease have not been eliminated, a blood clot in the vessels of the eye may form again, so in such cases the doctor prescribes a course of antiplatelet medications. These drugs, like anticoagulants, prevent the formation of blood clots, but act on the body more delicately. Most often, Aspirin or Plavix, familiar to many, is prescribed as preventive therapy.
Additional medications may be prescribed to relieve symptoms. Non-steroidal anti-inflammatory drugs include Ibuprofen or Diclofenac; antispasmodics include Papaverine, No-shpu and Riabal. If NSAIDs do not help, the doctor prescribes corticosteroid medications. To restore immunity, vitamins are prescribed.
For more serious lesions, therapy is carried out in a short time and more intensively, since doctors need to prevent complications from occurring and try to avoid surgical interventions. Preventive courses after such treatment are prescribed more often, and their duration increases.
If conservative therapy does not produce results, or there is a danger of irreparable consequences, the patient is prescribed laser coagulation. This is a non-invasive treatment method that allows you to achieve the desired effect in a short time. In this case, after completion of the intervention, the patient is prescribed a specialized course of medication.
Treatment
For thrombophlebitis, doctors prescribe treatment based on the diagnostic results obtained. Treatment includes:
- drug therapy;
- surgical intervention.
Thrombophlebitis has several forms: acute and chronic
If thrombosis affects the superficial veins, then treatment is carried out with medication. The patient is prescribed phlebotonics, anti-inflammatory drugs, ointments. Conservative treatment relieves swelling, reduces pain and restores blood flow. Anti-inflammatory drugs include drugs such as Ibuprofen, Aspirin and Diclofenac. Heparin ointment and Troxevasin have a local effect.
For thrombosis of superficial veins, doctors prescribe electrophoresis with anticoagulants, UHF therapy and magnetic therapy. Physiotherapeutic procedures dissolve blood clots and reduce swelling and pain.
Conservative treatment is carried out in combination with compression therapy. For thrombophlebitis, elastic bandages and compression stockings (stockings or tights) should be worn. The degree and class of compression is prescribed by a phlebologist depending on the severity of the disease.
Diagnostics
Diagnostics • Ophthalmoscopy • Fluorescein angiography.
Differential diagnosis • Diabetic retinopathy • Hypertensive retinopathy.
Treatment • In the acute stage •• Intravenous infusions of fibrinolysin 20,000 units and heparin 10,000 units (4-6 injections in total), alternate with intravenous infusion of rheopolyglucin •• Retrobulbar injections of RDG (reopolyglucin - 0.2, dexon - 0.2, heparin - 1000 units) and fibrinolysin 700–1000 units (alternate) •• Pentoxifylline 0.2 orally 3 times a day or 0.1 intravenously daily •• Etamsylate 250 mg orally 3 times a day or intramuscularly • • Acetylsalicylic acid 500 mg 3 times a day •• Antispasmodics, for example papaverine hydrochloride •• Diuretics, for example furosemide, acetazolamide • Laser coagulation of the retina •• For macular edema, barrier coagulation is indicated •• For postthrombotic retinopathy - sectoral (for thrombosis of the branches) or panretinal (for central vein thrombosis) coagulation of the retina to close ischemic areas and destroy neovascular complexes.
Complications • Optic nerve atrophy • Secondary neovascular glaucoma • Cystic macular degeneration
The prognosis depends on the size of the affected area of the retinal veins, the severity of macular edema and the timeliness of treatment procedures. However, in all cases the outcome is some degree of reduction in visual acuity.
ICD-10 • H34 Retinal vascular occlusions
http://eyesdocs. ru/zabolevaniya/redkie-bolezni/tromboz-centralnyx-ven-setchatki-opisanie-i-lechenie-problemy. html
http://gipocrat. ru/boleznid_id35075.phtml
Stages of the disease
Thrombosis of the central vein develops gradually in humans. If treatment is started too late, the person may develop vision loss. Sometimes absolute or partial thrombosis can be discovered accidentally during a routine examination.
The blockage is of a non-ischemic type (in this case, visual acuity remains above 0.1). With ischemic thrombosis, massive hemorrhages develop and signs of impaired capillary function are noted.
There are several stages of retinal vein thrombosis:
- Prethrombosis. In this case, the presence of tortuous, dilated, pathologically altered veins with an uneven diameter is observed. Macular edema is sometimes observed. Typically, patients at this stage do not present any symptoms. In some cases, visual acuity is slightly reduced. Visible objects may often become foggy.
- At the stage of occlusion of a vein or its branches, hemorrhages of various sizes are often noticeable. If the central vein is destroyed, then they are present throughout the retina. There are also cases where foci of hemorrhage appear only in the area of one branch of the vein. On examination, the boundaries of the nerve are usually not distinguished or are unclear. Swelling develops in the area of the macula. Characteristic symptoms are a significant decrease in visual acuity, scotoma (loss of part of the visual field). Often the patient notices a characteristic haze in the visual field.
- Some time after thrombosis, postthrombotic retinopathy develops. The patient's vision returns very slowly. Exudates and blood clots are visible at the bottom of the eye. Vascularization is noted, that is, unnatural formations of capillaries (normally they are not visualized at all).
Finally, recurrent thrombosis is also possible, when vein occlusion occurs repeatedly.
Retinal thrombosis: treatment
IT IS IMPORTANT TO KNOW! An effective remedy for restoring vision without surgery or doctors, recommended by our readers! Read more. Retinal diseases of vascular origin represent a serious problem in ophthalmology today.
With the widespread prevalence of hypertension, especially in combination with widespread vascular atherosclerosis, retinal vein occlusion is becoming more common. Today, retinal thrombosis is registered in every 2 people per 1000 population. The disease leads to a noticeable decrease in visual acuity, often resulting in loss of entire visual fields. This disables and causes professional unfitness and even disability for relatively young patients. But there is also reason to rejoice - methods of treating the disease described are being improved, the effectiveness of new drugs and techniques is being tested. Treatment of retinal thrombosis at the present stage involves the use of medications (conservative approach), cryotherapy using low temperatures, and laser exposure. Surgery is also possible
Retinal diseases of vascular origin represent a serious problem in ophthalmology today. With the widespread prevalence of hypertension, especially in combination with widespread vascular atherosclerosis, retinal vein occlusion is becoming more common. Today, retinal thrombosis is registered in every 2 people per 1000 population. The disease leads to a noticeable decrease in visual acuity, often resulting in loss of entire visual fields. This disables and causes professional unfitness and even disability for relatively young patients. But there is also reason to rejoice - methods of treating the disease described are being improved, the effectiveness of new drugs and techniques is being tested. Treatment of retinal thrombosis at the present stage involves the use of medications (conservative approach), cryotherapy using low temperatures, and laser exposure. Surgery is also possible.
Diagnostics
An experienced ophthalmologist can easily determine the degree of thrombosis. Diagnosis of the disease consists of interviewing the patient and conducting specific examinations. The doctor finds out when changes in visual functions began, what medications the patient is taking, and whether the person has certain diseases.
After conducting a survey and collecting information, studies are prescribed using special techniques:
- Visometry. The method involves studying visual acuity. In the ischemic form of thrombosis, the severity exceeds 0.1, in the non-ischemic form - below this indicator.
- Tonometry. During the study, the pressure in the eyeball is measured. Indicators are taken throughout the day. In a diseased organ, the numbers will be 2-3 mmHg. Art. lower than in a healthy person.
- Perimetry. A method that helps determine the narrowing of the field of vision (scotoma). With thrombosis, a similar phenomenon is observed in the area of the affected retina. The density of the scotoma varies with different amounts of hemorrhage and the presence of ischemic foci.
- Microperimetry. The method is used to determine the reaction of certain parts of the retina to light, which allows you to accurately identify the affected area.
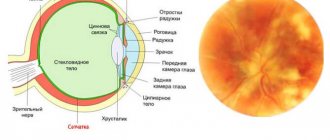
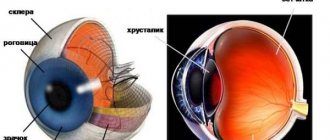
- Biomicroscopy. Allows you to see signs of thrombosis: crushing of the anterior chamber of the eye, a suspension of blood in the vitreous body, lack of a friendly reaction of the pupils when illuminating the diseased eye.
- Optical coherence tomography. Examination using a scanning beam helps determine the structure, size of swelling and features of the course of the disease. The method is used to evaluate the effectiveness of treatment.
- Fluorescein angiography (FA). An effective technique that helps determine the type of thromboembolism, the degree of the pathological process, the affected area, and the period of onset of the disease. The method is often used during the first examination; it helps determine the presence of thrombosis if other methods have not helped.
After confirming the diagnosis, appropriate treatment is prescribed aimed at eliminating the causes and symptoms of thrombosis and restoring visual function.
Self-determination of the disease at an early stage is impossible.
Symptoms are minimal; people often do not pay attention to minor visual impairment. Intense signs are observed with a serious course of the disease, when the person no longer sees well
A preventive ophthalmological examination is required at least once every 6 months. Regularly visiting a medical specialist will help you not to miss the onset of the disease and select therapy on time.
Diagnostic features
Determining the diagnosis is not difficult for an experienced ophthalmologist. Sometimes it is quite enough to perform an ophthalmoscopy of the fundus. Angiography is used to more accurately determine the extent of eye damage. Particular care should be taken to diagnose the anterior areas of the eyes.
Examination of the fundus of the eye is usually performed using a Goldmann lens. Additionally carried out:
- blood pressure measurement;
- determination of the degree of blood clotting;
- general clinical examinations - urine and blood tests (plus biochemistry);
- additional examinations are prescribed by a neurologist, endocrinologist, and cardiologist.