Ophthalmologist, Ophthalmosurgery
Gevorkyan
Armine Seyranovna
15 years of experience
Ophthalmologist, highest qualification category, member of the Russian Society of Cataract and Refractive Surgeons (RSCRS) and the European Society of Cataract and Refractive Surgeons ESCRS
Make an appointment
Keratitis is an inflammatory lesion of the cornea that has various causes and mechanisms of development. Diseases provoke clouding of the cornea, which leads to a significant decrease in vision. An accompanying clinical picture appears: lacrimation, photophobia, sensation of a foreign body in the eye, cutting pain, increased sensitivity of the cornea. Treatment is medication and microsurgical (if corneal ulcerations are detected).
Description
Keratitis is an ophthalmological disease in which the patient experiences an inflammatory lesion of the cornea of the eye, which is accompanied by ulceration, clouding, pain and hyperemia.
Eye keratitis is a fairly common disease, so when making this diagnosis, patients usually do not wonder what it is. If this pathology is not treated, patients may experience a decrease in visual function.
Today, doctors identify the following causes of keratitis:
- any injuries to the cornea that negatively affected its integrity;
- viral infection of the cornea of the eye (as a rule, the causative agent of herpes in this case is herpes);
- bacterial or fungal infection of the eye;
- complications after untreated conjunctivitis;
- violation or complete impossibility of closing the eyelids as a result of any injuries, disruption of the activity of the facial nerves;
- allergic reactions;
- vitamin deficiency, especially vitamin A;
- negative impact of contact lenses on the cornea.
Types of keratitis
Ophthalmologists distinguish the following types of keratitis: deep and superficial.
In the first case, the disease is usually a complication of conjunctivitis or other inflammatory eye diseases. After superficial keratitis, the patient does not experience scar tissue measurements and the cornea does not darken.
At the same time, deep keratitis of the eye is characterized by damage to the deeper layers of the eyeball. After treatment for deep keratitis, many patients experience scarring of the cornea of the eye, which subsequently negatively affects vision.
That is why, when the first symptoms of this pathology appear, it is recommended not to hesitate and not engage in self-diagnosis and self-medication, but to contact a specialist. Only a doctor knows the correct symptoms and treatment for keratitis.
In order to avoid serious complications of keratitis, specialists often prescribe hormonal drops and other “heavy” medications to patients.
Types of pathology
Bacterial keratitis
As a rule, this form of the disease develops after injury to the eye or with prolonged wearing of contact lenses, or poor hygiene when wearing lenses. Bacterial keratitis is usually caused by Pseudomonas aeruginosa. Although in some cases other bacteria may also be the causative agent of the disease. One of the most complex forms of bacterial keratitis is Acanthamoeba keratitis. In this case, the disease often affects both eyes at once and often leads to complete blindness;
Viral keratitis
In 80% of cases, the causative agent of viral keratitis is the herpes simplex virus;
Onchocerciasis keratitis
The cause of this pathology is usually various allergic reactions that occur in severe form. In this case, the pathology can affect both the anterior and posterior parts of the eyeball. In the absence of timely treatment, the pathology often leads to sclerosis of the eye membranes. The first signs of this pathology are itching, increased lacrimation and photophobia. In this case, patients often complain of redness of the cornea and severe swelling of the eyelids. In the absence of medical care, the disease can lead to severe vision loss, and in some cases to complete blindness;
Ulcerative keratitis
As a rule, this form of the disease develops in patients who have previously received injuries to the cornea of the eye from foreign objects. Ulcerative keratitis is often combined with purulent inflammation of the lacrimal sac. The disease is very severe and, if left untreated, can result in perforation of the cornea;
Fungal keratitis
In this form of the disease, the causative agent is usually various kinds of pathogenic fungi. In this case, the patient experiences severe pain, and the cornea of the eye begins to turn red. With fungal keratitis, the patient develops ulcerations in all layers of the cornea (both in the superficial and in the deepest). In advanced cases, patients may develop a through hole in the eyeball. In this case, the inflammatory lesion affects not only the cornea of the eye, but also nearby vessels (vascular keratitis). Often, a fungal infection causes the formation of a cataract and deterioration of vision. Fungal keratitis is very difficult to diagnose. This is why treatment for this disease often begins at the wrong time and occurs incorrectly;
Seasonal keratoconjunctivitis
As a rule, this pathology occurs in patients in the spring, when various plants begin to bloom. The main cause of the disease in this case is allergy;
Non-ulcerative keratitis
This is a fairly mild form of the disease in which the cornea of the eye swells, but no ulcerative lesions form on it. Often develops due to pathogenic bacteria entering the cornea of the eye;
Photokeratitis
This form of keratitis usually develops as a result of being burned by ultraviolet rays or artificial bright light. Often, patients with this pathology turn to doctors after a long stay in the sun without sunglasses or after using welding machines and neglecting protective parts;
Herpetic keratitis
The causative agent of this pathology, as a rule, is herpes simplex, much less often - the herpes zoster virus. After this form of the disease, patients often have deep ulcers on their corneas. It is a form of keratitis that is prone to recurrence. It can occur in both superficial and deep forms. In the superficial form of the pathology, cloudy spots form on the cornea of the eye. Superficial herpetic keratitis almost always occurs without pronounced symptoms. However, this type of disease is extremely rare. Much more often, patients turn to doctors with deep herpetic keratitis of the eye. With it, the patient develops extensive ulcerative lesions on the surface of the cornea. During recovery, such patients experience cicatricial changes in the tissues of the eye, and a cataract often forms.
Forecast and prevention of the disease
If the patient noticed signs of keratitis in time and immediately consulted a doctor, then the prognosis of the disease will be quite favorable. With the availability of a huge number of medications today, it will not be difficult for doctors to stop the pathological process in the cornea of the eye. This means that vision loss and the formation of eyesores can be completely prevented.
Disease prevention includes measures by which a person can avoid the development of pathology. These measures include proper storage and use of contact lenses. Lenses should only be stored in a special container. They should not be touched with dirty hands or worn for longer than expected.
In addition, prevention of corneal keratitis also involves timely treatment of conjunctivitis, since it is often a complication. It is also important to treat herpes on time, strengthen the immune system, and consume enough vitamins.
It is also worth avoiding injuries that may lead to the development of keratitis, and if they occur, immediately consult a doctor.
Causes
Caused by provoking factors:
- infections of various nature (viruses, fungi, bacteria);
- damage to the cornea due to a foreign object, burn, or injury;
- the influence of strong winds and the ingress of sand and dust particles;
- impaired metabolic processes, a consequence of endocrine diseases (diabetes, hypothyroidism, obesity);
- malnutrition, hypo- and vitamin deficiency;
- improper or insufficient care of contact lenses, especially long-term wear, when amoebas, Pseudomonas aeruginosa and Staphylococcus aureus multiply on the surface;
- diseases of the organ of vision (conjunctivitis, blepharitis, allergies, lagophthalmos and others);
- impaired innervation of the cornea;
- hypersecretion of meibomian glands;
- pathologies of the immune system;
- unknown reasons.
Symptoms
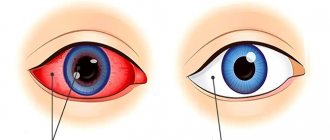
Photo: linza.guru
Keratitis is almost always accompanied by pain, the severity and nature of which largely depend on the prevalence of the process, as well as the reasons that provoked it.
With this pathology, the human sclera turns red, and the surface of the cornea of the eye loses its healthy shine.
Keratitis is often combined with corneal syndrome, the main symptoms of which are:
- photophobia;
- involuntary blinking or complete closure of the eyelids and the inability to open them;
- pathological tearfulness;
- sensation of a foreign body in the eye;
- decreased sensitivity of the cornea.
When examining such patients, ophthalmologists may see blood and lymph impurities (infiltrates) in the cornea, which are usually accompanied by clouding of the eye. These infiltrates may have different sizes, shapes, colors and be present in different quantities in different patients.
Depending on how deep the pathological process has spread in the tissue, infiltrates can be superficial or deep.
Superficial infiltrates often resolve on their own without any treatment and leave behind a slight cloudiness.
At the same time, deep infiltrates often disappear only after long-term treatment with “heavy” drugs and often leave behind scar changes that negatively affect a person’s visual functions.
In order to determine how long the patient has had an infiltrate, doctors examine its borders. Thus, blurred edges usually have fresh infiltrates, while clear ones have old ones that will soon begin to resolve.
Almost always, signs of keratitis include active vascularization of the cornea. During this process, the vessels begin to grow into the cornea of the eye. This has an extremely negative effect on the resorption of infiltrates.
On the one hand, ingrowth of blood vessels is a protective reaction of the cornea, and on the other hand, it has an extremely negative effect on its transparency, since normally a healthy person has no vessels in the cornea of the eye (which is why the cornea is transparent).
In severe cases, inflammation due to keratitis can also spread to the iris and ciliary contour. If keratitis is not treated in time or if you try to treat it yourself, it can lead to ulceration of the cornea and even rupture.
In addition, a frivolous attitude towards one’s health in this case can result in infection of the cornea of the eye, which can provoke a purulent-necrotic process, which in turn almost always entails complete loss of the eye.
In general, the symptoms of keratitis can vary quite greatly depending on the age of the patient, the state of his body (and immunity in particular), the individual characteristics of the pathogens, etc.
Viral keratitis
The causative agent of viral keratitis is often the herpes simplex virus. With it, damage to the cornea of the eye can be either deep or mild, superficial.
The very first and characteristic symptom of herpetic keratitis is the formation of a large number of small bubbles filled with liquid on the cornea of the eye. These blisters subsequently burst open on their own and leave behind ulcerations that often resemble the shape of a tree branch. Moreover, the more advanced the form of keratitis the patient has, the deeper the ulcerations on his cornea will be present. Often, symptoms of viral keratitis include the formation of a large number of deep infiltrates.
Filamentous keratitis
Filamentous keratitis in humans occurs as a result of various pathological processes in the body. The main symptom of filamentous keratitis is pathological dryness of the eye (in some cases, patients may even have a complete absence of tears when crying), cutting pain, photophobia, a feeling of the presence of a foreign body in the eye, involuntary closure of the eyelids.
In this case, as a rule, a filamentous viscous secretion forms in the eye. In advanced cases, patients may experience signs of hyperkeratosis. In severe cases, hyperkeratosis can cover the entire area of the cornea. In this case, clouding occurs, as a result of which the vision of patients sharply deteriorates.
If left untreated, patients may experience recurrent erosions and ulcers, which can ultimately lead to the formation of a through space in the eyeball.
Purulent-ulcerative keratitis
A purulent ulcer of the cornea of the eye, the causative agents of which, as a rule, are various types of cocci, also has characteristic features of its course. Even the most minor injury to the cornea of the eye or inflammatory damage to the eyelids can lead to this pathology. At the very beginning of the disease, patients usually develop a gray spot in the center of the eye or in the paracentral part of the eye, in place of which, after a short period of time, an acute ulcerative process develops. In this case, one of the edges of the ulcer is often slightly raised, which often leads to infection and the occurrence of a purulent-necrotic process. It is worth noting that this phenomenon occurs extremely rapidly. So, already 3-5 days after the formation of ulcers, the pathological process can spread completely to the entire cornea. In this case, at the bottom of the eyeball, as a rule, a fairly large amount of pus accumulates.
If the disease is not treated at these stages, a through hole may form in the eyeball, through which the pus will subsequently release on its own. As a rule, after this the patient begins to recover, and rough scars or a cataract begin to form on the cornea, which subsequently negatively affects vision.
It is worth noting that recovery in such patients does not always occur. In some cases, the purulent-necrotic process can spread to healthy tissues of the human body.
Neurogenic keratitis
The main cause of neurogenic keratitis is damage to the trigeminal nerve. As a result, a flat ulcer begins to form in the center of the eye. Moreover, this process can take a lot of time and not be accompanied by any special sensations, since the cornea of the eye often completely loses its sensitivity.
With this form of keratitis, the clouding of the cornea is insignificant, and ulcers that have a small area heal quickly. However, if an infection is added to the ulcerative lesion, the pathology may be complicated by a purulent-necrotic process.
Acanthamoeba keratitis
Patients who prefer wearing contact lenses to glasses are at risk of developing Acanthamoeba keratitis. The disease gets its name from the causative agent, the Acanthamoeba bacterium. This form of the disease is difficult to treat. However, it often affects both eyes. After such keratitis, the cornea of the eye often becomes cloudy, which can negatively affect vision in the future.
At the first symptoms of keratitis, patients should immediately contact an ophthalmologist and not self-medicate. This pathology can only be treated in a hospital setting under the close supervision of doctors, since this disease can lead to significant changes in the structure of the eye tissues, which can subsequently cause decreased vision and even lead to complete blindness.
Classification
The division of the disease into varieties is based on many criteria - the depth of the lesion, the cause, the location of the infiltrate, the nature of the course.
According to the depth of the lesion there are:
- superficial keratitis – affects the epithelium and upper stromal layer, total depth up to a third of the cornea;
- deep type - the entire stroma is inflamed;
Depending on the location of the infiltrate, 3 types of keratitis are distinguished:
- central - in the area of the pupil, so vision deteriorates as much as possible;
- paracentral – in the projection of the iris belt;
- peripheral - in the limbus area.
One of the classification criteria is origin, or etiology. According to him, there are the following types of keratitis:
- exogenous forms;
- endogenous forms.
In turn, exogenous forms are divided into:
- bacterial;
- viral;
- fungal;
- amoebic;
- traumatic types;
- meibomian;
- keratitis caused by damage to the conjunctiva and eyelids;
- corneal erosion.
Exogenous forms include varieties provoked by infections and other factors:
- allergic;
- tuberculosis;
- syphilitic;
- brucellosis;
- hypo- and vitamin deficient;
- malarial;
- neurogenic;
- dystrophic;
- keratouveitis;
- traumatic;
- photokeratitis;
- of unknown origin (rosacea keratitis, filamentous keratitis, corneal ulcer), etc.
The filamentous type is provoked by insufficient production of tear fluid and drying of the epithelium.
The disease is divided into acute, subacute, recurrent and chronic stages.
Diagnostics
Photo: gc-iris.ru
The number of methods for diagnosing keratitis today is sufficient to make a correct diagnosis and prescribe effective treatment. At the first symptoms that affect a person’s health, it is necessary to consult a doctor - an ophthalmologist, who will perform the required examination of the cornea using certain diagnostic methods. Statistics, according to experts, indicate 60% detection of keratitis due to the use of modern diagnostics.
Methods for diagnosing keratitis, depending on the individuality of the case, can be as follows:
- examination of the cornea of the eye, study of its sensitivity;
- corneal biopsy and scraping;
- corneal microscopy;
- fluorescent antibody method;
- tuberculin tests;
- bacteriological culture;
- pachymetry.
Characteristics of methods for diagnosing keratitis
Diagnostic methods include:
- The study of the sensitivity of the cornea of the eye is the following procedure: a wick consisting of cotton wool is applied to the center of the cornea, and then at 4 different points, approximately equally distant from each other, with the eyes wide open. If the patient does not respond to this manipulation, then we can conclude that the sensitivity of the cornea is reduced or absent;
- The cornea is scraped using a special spatula with a curved needle end or blade. In order to numb the pain, the doctor injects local anesthesia, after which a scraping is taken from the cornea with a high degree of accuracy, monitoring the process using a slit lamp. The taken material must be placed on glass to identify the environment. This method is often used for acanthamoeba keratitis, which is caused by unhygienic use of contact lenses;
- Corneal microscopy is one of the most modern research methods; it helps to study corneal tissue, measure its layers, and also allows us to understand how much tissue viability is impaired. If a patient has problems with the cornea due to the effects of inflammatory processes, injuries or surgical operations, this method makes it possible to make a reliable assessment of the severity of the negative impact, determine the treatment regimen and its effectiveness;
- The fluorescent antibody method is most often used in cases of herpetic keratitis, which appears under the influence of the herpes virus. It consists of taking a smear that contains the antigen, applying it to glass with the addition of globulins, keeping it in a humid chamber for half an hour or 40 minutes, then rinsing the smear with distilled water. In the case of antibody and antigen specificity, a light green glow of the antibodies can be seen;
- Tuberculin tests are considered the main diagnostic method for tuberculous keratitis. With their help, the body's predisposition to the possibility of infection with tuberculosis bacteria is studied. To identify this predisposition, Alttuberculin is injected into the body (in the forearm). After this, the body's reaction to the drug is monitored. The mantoux test is harmless; it is given routinely even to children in the first week of life. If the patient is infected, an increase in compaction is observed, as well as a negative test result after several positive results in previous years;
- Bacteriological culture for keratitis is carried out if purulent discharge from the eye is observed; it helps to determine the presence of microorganisms on the cornea of the eye, their type and allows us to understand how to prevent the reproduction and spread of these bacteria. When examining the eye, the ophthalmologist puts forward a hypothesis about the presence of bacteria; using bacteriological culture, it is possible to assess whether the microflora is disturbed and identify the presence of an inflammatory process. Before carrying out bacteriological culture, the patient is given an anesthetic, after which biological material is collected using a glass rod, Pasteur pipette or bacterial loop. The collected biological material is placed in a sterile environment and transferred to the laboratory for research;
- Pachymetry - this method is used to study the thickness of the cornea of the eye. It can be done in two ways (using ultrasound or a slit lamp). The feasibility of the procedure is determined by the presence of swelling and inflammation of the eye. Pachymetry is considered a non-contact examination method: using a slit lamp, the ophthalmologist is on one side of the equipment and the patient is on the other. His chin is placed on a special stand, and the doctor directs the light to the required point, automatically measuring the thickness of the cornea in different places, and then compares it with the norm.
The diagnostic procedure using ultrasound equipment is the most accurate: the patient lies on a couch next to the device, is given an anesthetic, and is touched with the part of the device on which the nozzle is located. Through automated information systems, measurement results are displayed on the screen and data is calculated, which are then used to assess the thickness of the corneal region.
If you find primary signs of keratitis, then independent use of medications is strictly contraindicated, since only an ophthalmologist can diagnose using specialized equipment and prescribe effective treatment. After all, when prescribing drugs, it is necessary to take into account the individual characteristics of the human body, the presence of allergic reactions to drugs, the causes of keratitis, the severity of the course and the type of disease. A quick visit to a specialist can affect the final result of the treatment process.
Treatment
Photo: sovdok.ru
Keratitis is a serious inflammatory disease of the cornea of the eye, manifested by a variety of ophthalmological symptoms. This disease is treated by an ophthalmologist in a specialized medical hospital. Treatment of keratitis is determined by three factors: the cause of the disease; the depth of corneal damage and the severity of the process.
The following types of therapy are used in treatment:
- Medicinal methods of treatment, including antibacterial and antiviral agents, antiseptic solutions, drugs that promote epithelization on the cornea, etc.
- Surgical methods: keratoplasty, corneal transplantation, etc.
Drug therapy
Treatment of keratitis is recommended to be carried out in a medical hospital (due to the risk of developing complications that are severe for the patient’s vision). The basis of treatment for keratitis is eliminating the causative factor. Most often, in adults it is a bacterial or viral infection that affects the cornea both primarily and against the background of an ongoing infectious disease of another localization in the body. In children, the most common cause of keratitis is a viral infection and eye injury. It is very important to stop using lenses for the entire duration of treatment for keratitis.
Treatment of viral keratitis requires the prescription of antiviral agents, which are usually used in the form of drops or ointments that must be placed in the conjunctival sac. In addition, it is possible to use interferon drugs and interferon inducers both locally and systemically. Interferons make it possible to block the reproduction of the virus and its transition from cell to cell, thereby reducing the intensity of the disease and damage to the cornea. Additionally, immunomodulators are used orally or intravenously to stimulate the activity of the immune system.
If ulcers form on the cornea during antiviral therapy, then it is necessary to use microsurgical methods (microdiathermo- and laser coagulation, cryoapplication) to close the resulting defect and prevent it from spreading to healthy eye tissue.
Herpetic keratitis is treated with acyclovir, used both internally in the form of tablets and topically, in the form of drops. This allows you to easily and quickly block the virus in the body and destroy it. The most modern drug in the acyclovir group is ganciclovir (the trade name for the eye gel is Zirgan). In no case should you use glucocorticosteroid ointments, since their use against the background of infectious keratitis can lead to the formation of extensive corneal ulcers and the spread of infection to other parts of the eyeball. If therapy is not effective within a month, then surgical treatment in the form of a corneal transplant is recommended.
If keratitis is caused by a bacterial infection, then the key point of treatment is the prescription of antibacterial drugs. The most commonly used drugs are sulfonamides, penicillins and cephalosporins in the form of drops, ointments and special medicinal films. It is recommended to conduct a study on the sensitivity of the pathogen to antibiotics before prescribing these drugs. In case of severe purulent processes in the cornea (often with infection with staphylococcus and Pseudomonas aeruginosa), antibacterial drugs are administered subconjunctivally, as well as intramuscularly or intravenously. In cases of ulceration, microsurgery methods are indicated.
For specific types of keratitis, for example tuberculosis, drugs are used that target a specific pathogen - anti-tuberculosis drugs, anti-syphilitic drugs, etc.
Along with medications aimed at the causative factor of keratitis, other medications are also used:
- Mydriatics, which improve the outflow of intraocular fluid from the eye cavity. Their use is due to the increased formation of intraocular fluid during keratitis due to the development of the inflammatory process in the cornea. They are usually used in the form of drops.
- Antiseptic solutions allow you to quickly clean and disinfect the surface of the conjunctiva, clearing it of bacteria. Used in the form of drops for instillation or rinsing of the conjunctival sac.
- Medicines that promote epithelization of the corneal surface are especially often used against the background of formed and developing ulcers. They allow you to quickly close the epithelial defect without the formation of connective tissue, which helps maintain clear vision.
- For the allergic component of the disease, it is recommended to use eye drops with antihistamine properties (Opatanol) or containing glucocorticosteroids. In this case, it is especially important to eliminate the allergen that causes keratitis.
- Vitamin therapy is also used to improve regenerative processes in the body and increase the rate of corneal epithelization.
To treat common herpetic ulcers, corneoplast is used - this is crushed, dried and preserved cornea of humans and a number of animals (pigs, sheep, etc.). The corneoplast contains large quantities of collagen and keratin sulfate, which determine the basic properties of the cornea. Corneoplast has a good healing effect. For long-term, recurrent herpes keratitis, an antiherpetic vaccine is used to cause long-term remission of the disease in the patient.
For bullous keratitis, use baths with a 10-20% glucose solution and placing 0.5% thiamine ointment in the conjunctival sac. In addition, collazin is used in the form of eye drops or subconjunctivally with a solution of novocaine.
Surgery
Surgical methods for treating keratitis are used for various forms of the disease. It is important to remember that during treatment and rehabilitation it is necessary to stop wearing contact lenses for keratitis due to the risk of complications and progression of the disease. If ulcers form on the cornea, then microsurgical interventions are used: laser and microdiathermocoagulation or cryoapplication of the defect. These methods can quickly stop the spread of the ulcer and improve a person’s prognosis in the long term.
If, as a result of keratitis, clouding of the cornea occurs and, as a result, decreased vision, then excimer laser scar removal techniques or keratoplasty are used. The operation of choice is layered keratoplasty, which allows you to preserve healthy layers of the cornea. Only corneal tissue that has changed as a result of the disease can be removed.
The development of secondary glaucoma against the background of keratitis requires laser or surgical correction of this condition, which consists in normalizing the outflow of intraocular fluid from the internal cavities of the eyeball.
If keratitis cannot be treated with conservative and surgical methods for a long time, then the best treatment option is eye enucleation.
Prevention of keratitis
The outcome and long-term consequences of keratitis depend on a number of factors: the cause of the disease, the depth and duration of the inflammatory process. Modern treatment methods make it possible to quickly cope with keratitis and prevent the development of opacities in the cornea.
Prevention of keratitis consists of several points: rapid detection and treatment of inflammatory diseases of the eye (conjunctivitis, blepharitis, dacryocystitis) and infectious diseases in the body. In addition, it is recommended to avoid traumatic effects on the eye, as well as undergo treatment for somatic and allergic diseases. Timely treatment of herpetic infections can minimize the risk of developing the most commonly detected herpetic keratitis.
In conclusion, we can answer the most common question: is it possible to cure keratitis? Yes, of course it is possible, if you consult a doctor in a timely manner and start treatment. It is important to remember that keratitis is a disease that requires hospitalization of the patient due to the risk of developing complications from the eyeball and impaired vision clarity. Diagnosis and treatment of keratitis should be carried out by an ophthalmologist.
Medicines
Photo: vesti-ukr.com
Productivity of drugs for keratitis, their features
Treatment of keratitis with medications depends on the degree of damage to the cornea of the eye, the cause of the disease, as well as the severity of the disease. Keratitis should be treated with:
- ointments;
- eye drops;
- injections (intramuscular and intravenous);
- tablet drugs.
Statistics, according to eye doctors, indicate that herpetic keratitis is in first place in terms of the prevalence of the disease.
When the first symptoms of the disease appear, you need to see a doctor who will conduct a diagnosis, make a diagnosis, and prescribe effective treatment. In order to understand what medications to take for keratitis, you need to know what type of keratitis is progressing in your case. When keratitis occurs, it is important to have a comprehensive and structured treatment using all medications that support the body. Each case is individual, the prescription of medications depends on the cause of the disease and the severity of the disease. Using medications on your own without consulting a specialist can lead to negative consequences and complications that arise from improper use of medications.
Taking medications for keratitis depending on the type of disease
There are several types of keratitis, according to which the effect of drugs that act on the original cause of the disease is determined:
Herpetic keratitis
Drugs for herpetic keratitis most often use anti-inflammatory drugs (treatment of keratitis with drops "Garazon", ointment for keratitis "Dexagentamicin"), immunomodulating drugs (tablets "Lavomax"), as well as drugs based on acyclovir - "Zovirax", "Acyclovir-acri" " Such drugs correct the activity of the immune system and relieve inflammation of the cornea. Antiherpes drugs act on viral cells, killing them.
Viral keratitis
Antibacterial agents (Baziron, Alpizarin ointment), Interferon (in eye drops for keratitis) have a great influence on the inflammatory process; they support the body, restore immunity, and supply vitamins.
Fungal keratitis
drugs for the treatment of keratitis of fungal etiology can be the following: antifungal agents - “Natamycin”, “Amphotericin B” in tablets, they have a destructive effect on the fungus and contribute to the successful restoration of the functions of the cornea of the eye.
Allergic keratitis
The main medications for treatment are antihistamines - Suprastin, ointments based on corticosteroids - Sinaflan. These products relieve swelling and suppress the allergen that provokes the development of keratitis.
In case of severe disease or complications in the body, injections are used for keratitis, which are administered intramuscularly (“Trifosadenine”, “Retinol”). The therapeutic effect for keratitis is aimed at destroying the infection and stopping the inflammatory process of the cornea. And if ulcers form in the corneal area, specialist doctors may prescribe antibiotics for keratitis - Erythromycin, Tetracycline. In case of any damage to the cornea, drops are used for keratitis, such as Tobrex, Korneregel, they promote rapid healing of the area of inflammation.
In addition to drug treatments, many people use folk remedies.
Main manifestations of bacterial keratitis
- clouding of the cornea;
- the appearance of ulcers of varying degrees of depth;
- formation of purulent mucous discharge;
- corneal syndrome;
- severe pain in the affected eye.
To diagnose bacterial keratitis, microscopy, keratometry, keratotopography, eye biometry, and corneal sensitivity analysis are used. When treating bacterial keratitis, a course of antibiotic therapy and medications that dilate the pupil are prescribed. In case of complications, surgery may be prescribed.
Folk remedies
Photo: dzhmao.ru
The appearance of keratitis is promoted by various infectious diseases, eye injuries, and negative environmental influences. The patient has an inflammatory process of the cornea of the eye. Keratitis can develop over a long period of time – from several days to several months. An advanced stage of the disease can lead to complete blindness. Therefore, at the first symptoms of keratitis, you should immediately consult a doctor. Treatment of a disease begins with identifying the cause of its occurrence. To do this, the patient should undergo examination by a specialist who will prescribe surgical treatment. Together with medications, effective methods of treatment with folk remedies will help.