Data from the World Health Organization (WHO) show that corneal damage ranks first among the leading causes of blindness after glaucoma, age-related macular degeneration and cataracts. The cornea is the anterior transparent part of the outer shell of the eye, which is very vulnerable to the negative effects of mechanical, physical and chemical environmental factors.
Any changes in the basic properties of the cornea (transparency, sphericity, sensitivity, size, specularity) are accompanied by a decrease in visual acuity and require conservative or surgical treatment. Unfortunately, conservative treatment methods require a long time and cannot always guarantee the restoration of the original characteristics of the cornea and the restoration of impaired visual functions. Therefore, there is an urgent need to use surgical treatment methods and, in particular, keratoplasty.
Who is a corneal transplant indicated for?
According to statistics, various types of corneal pathologies account for 25% of all diseases of the visual organs. Impaired visual acuity caused by corneal pathologies is in most cases irreversible and cannot be corrected with glasses or contact lenses. That is why keratoplasty is actually the only effective treatment for patients with changes in the transparency (opacity) of the cornea or a violation of its sphericity. Corneal transplantation is used for:
- keratoconus and keratoglobus;
- avascular corneal cataract (formed as a complication of keratitis and corneal ulcers, after a chemical or thermal burn);
- post-traumatic scars of the cornea (including after operations);
- congenital or acquired corneal dystrophies.
Before undergoing surgery, all patients who require a cornea transplant must undergo a thorough examination to identify contraindications and risk factors, as well as predict the results of the intervention. If risk factors such as entropion, ectropion, blepharitis, bacterial keratitis, etc. are detected, they must be eliminated before keratoplasty.
Types of keratoplasty
Cornea transplantation (keratoplasty) is a microsurgical surgical intervention during which the damaged cornea is removed and replaced with a donor graft or keratoprosthesis (KP).
There are two types of corneal replacement material:
- donor tissue - which is removed from the corpse within no more than 2 hours after death;
- keratoprostheses (artificial cornea) - examples of such devices: Boston KP (types I and II), osteo-odonto-keratoprosthesis (OOKP), AlphaCor and Fedorov-Zuev KP. The Boston KP is the most common implantable corneal prosthesis.
All over the world, preference is given to donor corneas. This is a very favorable material for transplantation, since the risk of rejection is minimal due to the peculiarities of its anatomical and physiological structure and the absence of its own blood vessels. But sometimes corneal transplantation is still complicated by rejection (repeated in some patients); it is in such situations that they resort to installing a keratoprosthesis.
Implanted keratoprosthesis Boston
Donor materials for cornea replacement are produced by special licensed medical institutions. There are even special eye donor banks that collect material, process it and store it. Such transplants are made in sterile laboratory conditions, and they are all tested for the presence of viral, bacterial and other lesions.
In eye microsurgery, cornea transplant operations are classified:
- by size of the transplanted area: complete (total) and partial (local and subtotal);
- according to the layers of the cornea, which the surgeon changes: through, anterior layer-by-layer and posterior layer-by-layer.
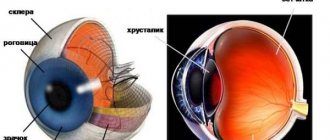
REFERENCE! The cornea of the eye has 5 layers: superficial epithelial cell layer, Bowman's membrane, stroma, Descemet's membrane, endothelial cell layer.
Structure of the cornea
Penetrating corneal transplantation is the most common type of keratoplasty. In this situation, the damaged cornea is replaced completely, that is, the entire thickness (all 5 layers are replaced). This operation is needed for patients with keratoconus and other congenital anomalies of the structure of the cornea in children, as well as for extensive injuries, burns, and necrosis.
Layer keratoplasty is indicated for patients with damage to the cornea that is superficial. Surgical interventions on the anterior or posterior part of the cornea are performed for people with burns, dystrophies, opacities or various keratopathies. Such interventions can be divided into 2 subcategories:
- DALK – deep anterior layered keratoplasty (transplantation of the anterior 3 layers of the cornea, leaving Descemet’s membrane and endothelial layer of cells);
- DMEK – posterior partial keratoplasty (replacement of only the posterior endothelial layer of the cornea).
The main types of keratoplasty, depending on the layers of the cornea that are changed during the operation
How does the operation take place?
The operation is performed in a “one day” mode; the choice of anesthesia method depends on various factors (age, type of corneal pathology, general condition of the patient, etc.); both local and general anesthesia can be used.
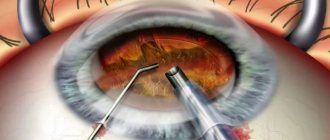
The eyeball is fixed, the surgeon determines the exact size of the area of the cornea that needs to be removed. After forming a corneal flap with the specified parameters, the affected tissue is removed. In their place, a corneal graft is implanted, the dimensions of which completely coincide with the dimensions of the removed flap.
If necessary, laser support for keratoplasty can be used using a femtosecond laser (our clinic uses the latest installation - Wavelight FS200 Femtosecond, which has the highest speed of corneal flap formation).
According to indications, reconstruction of the anterior segment of the eye can be performed simultaneously (cataract removal, installation or replacement of IOLs, destruction of synechiae, iris plastic surgery, etc.). After completing all the necessary manipulations, the transplant is fixed with a special suture material (the thickness of the thread is much thinner than a human hair), a tight pressure bandage is applied to the operated eye, and special protective contact lenses can also be used. On the day of surgery, the patient returns home.
In what cases can organ transplantation be performed?
The history of already performed operations shows that for their successful implementation it is necessary to coordinate the actions of doctors of several specialties: immunologists, hematologists, laboratory diagnosticians, and sometimes biophysicists.
But in order to transplant an organ into a person, serious reasons are needed. The list of diseases that serve as indications for transplant operations is presented in the table:
| Organ | Indications for transplantation |
| Bone marrow | cancer diseases (lymphomas and leukemia); severe types of anemia; hereditary metabolic disorder; immunodeficiency conditions of a hereditary nature. |
| Liver | viral hepatitis B, C, D; pathology of alpha-1 antitrypsin metabolism; autoimmune hepatitis; hemochromatosis; Wilson's disease; cancer; polycystic disease; fulminant, massive and acute necrosis of hepatocytes without the possibility of recovery. |
| Heart | myocarditis; cardiomyopathy; final stage of ischemic disease; congenital defect; tumor (myxoma). |
| Kidneys | chronic failure at the last stage; malignant tumors in the kidneys. |
Organ transplantation in Germany is regulated by the relevant transplant law, which allows organs to be taken from a living or deceased donor. In this case, no monetary reward is provided. Otherwise, the transplant may be considered organ trafficking, which entails criminal liability.
Regardless of which system will be transplanted, there must be pathologies or conditions that cannot be eliminated therapeutically or surgically, or that pose a direct threat to the patient’s life.
Recovery after keratoplasty
The rehabilitation period after keratoplasty is quite long and ranges from 9-12 months or more, this is due to the structural features of the cornea. Sutures are removed no earlier than 6 months (or later) after surgery. To avoid postoperative inflammation of the cornea and reduce the risk of transplant rejection, glucocorticoids and antibacterial drugs in the form of eye drops are prescribed (for at least 2 months after surgery). During the entire healing period, it is recommended to carefully protect the eye from mechanical damage and avoid heavy physical work.
Corneal rejection after transplantation and other complications
Corneal transplantation is usually successful. The most dangerous and unfavorable complication of keratoplasty is graft rejection. Donor corneal biomaterial is rejected quite rarely, which is due to the lack of blood vessels in the graft, and it is sutured to the same avascular (without vessels) surface.
Typically, the risk of rejection does not exceed 5% (with keratoconus), but can increase to 68% with a severe chemical burn of the cornea. Also, the risk of rejection increases in patients with penetrating keratoplasty, compared to the layer-by-layer surgical technique.
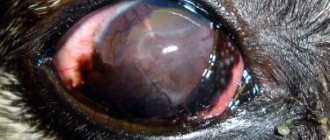
Symptoms that may indicate the development of donor corneal rejection:
- decreased visual acuity,
- photophobia,
- eye pain,
- redness of the eyeball.
As a rule, an episode of rejection can be stopped if appropriate treatment is prescribed in time (glucocorticosteroids in eye drops, in the form of parabulbar injections, in severe cases - systemically orally in tablets or intravenously in an injection solution). After successful therapy, the graft function is completely restored.
To prevent rejection of the donor cornea, the patient is prescribed instillations of glucocorticosteroid hormones into the conjunctival sac for a long time
In cases where the episode has been long and severe, or the patient has already experienced several such situations, the donor cornea may become unusable. Such people are indicated for a second transplant, but the long-term prognosis in this situation is worse than with the first transplant. If the donor cornea is rejected from the patient for the first time, a keratoprosthesis (artificial cornea) can be installed.
Other possible complications include infection, inflammation, bleeding, and increased intraocular pressure. Their risk is higher with penetrating keratoplasty and posterior lamellar keratoplasty than with anterior lamellar keratoplasty, since with the latter the operation occurs outside the cavity of the eyeball, but only on its surface.
Advantages of keratoplasty in MGK
Before undergoing surgery, our patients undergo a thorough eye examination using the most modern diagnostic equipment from major international manufacturers. Our Clinic has all the necessary equipment for cornea transplantation and its own bank of biotransplants. In 2014, 21 end-to-end corneal transplants were performed at MGK, which is the highest figure among non-state ophthalmological centers in Russia.
World-class specialists work at the Moscow Eye Clinic. Penetrating keratoplasty is one of the priority tasks of the clinic. The clinic employs Professor Alexey Yurievich Slonimsky, one of the most authoritative specialists in the treatment of patients with various corneal pathologies, a recognized leader in the field of end-to-end transplantation for keratoconus, and the author of a monograph on keratoconus. Professor Slonimsky Yu.B. - Member of the Board of the Russian Society of Ophthalmologists. Among fellow ophthalmologists, Yuri Borisovich is a recognized authority in the field of treatment of patients with severe corneal pathology. These operations are performed by a surgeon of the highest category, the chief physician of the clinic, Natalya Ivanovna Fomenko, who has successfully performed more than 12 thousand operations of varying complexity.
An individual approach and attentive attitude to each patient are the key to effective treatment at the Moscow City Hospital. We care about our patients, so we are ready to provide all the required assistance every day, seven days a week, from 9 am to 9 pm. For the convenience of our patients, we have a hospital (including a day hospital).
Keratoplasty price
Donor cornea transplantation is an expensive surgical procedure, as it requires a highly qualified specialist and expensive medical equipment. The average cost of surgery on one eye is 100,000 rubles, the price of a donor transplant is approximately the same.
Fortunately, there is a special government program that guarantees free surgery for patients with indications for it. But in order to take advantage of this chance, it is necessary to undergo a special medical examination, provide all the necessary documents to the commission and get in line at the local department of the Ministry of Health.
Cost of treatment
The price of keratoplasty surgery is determined by the volume of surgery, the need to use general anesthesia, etc. The cost of performing penetrating keratoplasty in our clinic ranges from 90,000 rubles. for one eye, when reconstructing the anterior segment of the eye, the cost of the operation may increase. Biomaterial is paid separately (its cost is 98,000 rubles).
You can find out the cost of a particular procedure by calling the MGK hotline number 8(800)777-38-81 (toll-free from mobile phones and regions of the Russian Federation) and telephone in Moscow +7(499)322-36-36 or online, use Skype consultation on the website, you can also familiarize yourself with the “Prices” section.
Go to the “Prices” section>>>
Cost of operations
The financial component of travel for treatment worries foreign patients the most. Indeed, even without preliminary monitoring, one can assume that the price will be quite high, given the complexity of the operations.
An approximate price list for 2021 is shown in the table:
| Service | Estimated cost, € |
| Lab tests | 250-300 |
| Examination in hospital | 3 500-4 000 |
| MRI of the heart | from 1 600 |
| Heart valve replacement | from 22 000 |
| Joint replacement | from 13 000 |
| Bone marrow examination | from 8 000 |
| Allogeneic bone marrow transplant from an unrelated donor | from 200,000 |
| Allogeneic bone marrow transplantation from a related donor | from 250,000 |
| Autotransplantation | from 100,000 |
To these amounts you must add the cost of flights and accommodation in the country.
Statistics on transplantology in Germany
The first thing that worries patients who are about to undergo such a complex operation is how long the person can live after the transplant. And here it all depends on which organ is being replaced, how old the patient is, and what is his general state of health.
On average for the country, according to the German Ministry of Health, the figures look like this:
| The likelihood of organ rejection after operations in German clinics | 0,5 %. |
| Survival after surgery | One-year – 88% for men, 86% for women; Two-year – 79 and 77%, respectively; Five-year – 73 and 69%. |
| Survival by gender | Men have a 15% higher life expectancy than women. |
| Early mortality (immediately after surgery) | 5-10% of cases. |
| The main indication for liver transplantation is Hepatitis C | In 30% of cases. |
| Organ most often donated by deceased donors | Kidney - in 50% of cases. |
| Number of organs that were donated in 2021 | 797 (this is the minimum mark over the last twenty years). |
| Number of patients awaiting transplant | About 10 thousand (as of 2021) |
What do you need to go for treatment?
The process of organizing a trip can be the most difficult part. First you need to decide whether you will deal with all the details yourself or turn to the services of intermediaries. The latter will relieve you of the burden of emotional and time costs, but will impose the obligation to pay for assistance.
If you are more satisfied with the first option, then stick to the following scheme:
- Find a clinic that specializes in your problem.
- Make a request to the medical institution with a description of the disease and diagnosis. Attach the results of the examinations already completed. All documentation must be drawn up in German or, in extreme cases, English.
- If the answer is positive, the medical center will tell you the account number where the money needs to be transferred.
- Having received an invitation from the clinic, go to apply for a visa permit.
Most often, for trips of this type, the German consulate issues a visa category C. On its basis, you can stay in the country for no more than three months.
Be prepared for the fact that the medical center will first ask you to look for a donor on your own. Most often, they are close relatives, especially when it comes to liver or kidney transplantation.
In some cases, the clinic accommodates the patient and offers to use an organ bank. But this most often happens when the upcoming operation is of high significance for science and research.
Keratoplasty
- Methods and types of keratoplasty
- Posterior automated lamellar keratoplasty (PAK or DSAEK)
- Operation prognosis
- Transplant material
In the literature, along with keratoplasty, another term is also found - corneal transplantation. Most authors put the same meaning into these concepts, although this is not entirely true.
Keratoplasty should be understood as surgical operations on the cornea aimed at restoring its shape and functions, eliminating congenital and acquired defects and deformations after injuries and diseases using various transplantation methods.
Corneal transplantation is the transplantation (movement) of the cornea with its subsequent engraftment within one organism, or from one organism to another of the same species, or even of a different species. Thus, it turns out that in keratoplasty, although a graft is used, it is not necessarily a corneal one. The corneal graft itself can also be used for corneal, scleral, conjunctival and other types of plastic surgery. In other words, when we use the term corneal transplantation, we mean that we are transplanting the cornea, but with the term keratoplasty we specify that we are transplanting onto the cornea.
Methods and types of keratoplasty
The division of keratoplasty by type is based on:
- the area of the excised area of the recipient's cornea and the corneal graft used;
- depth of intervention on the recipient's cornea and thickness of the transplanted graft;
- purpose of the operation.
The size of the excised area of the recipient's cornea and the transplanted donor corneal graft in the vast majority of cases is judged by the diameters of the trephines used during the operation. So, with a normal size of the cornea (vertical - 11 mm, horizontal - 12 mm) of the patient, keratoplasty is distinguished
- partial (up to 6 mm in diameter, usually 4-6 mm),
- subtotal (6.5-9 mm), when the patient’s own cornea remains on the periphery, and
- total (9.5-12 mm). In total corneal transplants, grafts with a scleral border are occasionally used. The latter is necessary for fixing the graft within healthy tissue (for example, behind the sclera in burns).
Much less often, depending on the shape, size and location of the pathological area on the patient’s cornea, the ophthalmic surgeon does without the usual trephines, cutting out other geometric shapes (regular and irregular) on the patient’s cornea. However, in this case, depending on the area of the recipient’s remaining cornea, we can talk about partial, subtotal and total keratoplasty.
Layer-by-layer corneal plastics are those in which only part of its layers are replaced (or restored) with a graft. Depending on the depth of the intervention and, consequently, the localization of the replaced corneal layers, layer-by-layer keratoplasty is divided into
- anterior lamellar keratoplasty (ALK) - only the anterior layers of the cornea are replaced (or restored), while the posterior layers (part of the stroma, posterior limiting membrane, endothelium) remain intact.
- interlamellar layer keratoplasty (ILK) - part of the stroma is replaced,
- posterior lamellar keratoplasty (PLK) - only the posterior layers are replaced.
In most cases, grafts with a diameter of 6-10 mm are chosen for PPC, 5-7 mm for ILC, and 4-8 mm for PPC.
Posterior automated lamellar keratoplasty (PAK or DSAEK)
In the last few years, the operation of posterior automated layered keratoplasty (PAK or DSAEK) has gained wide popularity and is now recognized as the standard of surgical treatment for patients with corneal endothelial dysfunction in the absence of irreversible destruction of the fibrillar elements of the stroma.
The generally accepted method of preparing a graft for PAD is its layer-by-layer cutting out from the corneoscleral disc of the donor cornea, fixed in the artificial anterior chamber apparatus using an automated microkeratome. In this case, the surgeon performs one cut with a microkeratome using 300 or 350 µm heads, the choice of which is made depending on the initial thickness of the donor cornea. The final pachymetry value, measured in the central zone after making the cut, averages 250 µm and often varies over a very wide range of values (from 180 to 350 µm).
This is facilitated by fluctuations in the depth of cut, inherent in all types of microkeratome heads, due to the deviation of their geometric parameters from ideal, as well as the presence of backlash in the connections. The variability of the depths of the microkeratome head sections is also determined by the parameters of the intracameral pressure in the donor cornea fixation system and the diameter of the cut out flap. It should be noted that the individual anatomical features of the donor material, including the timing of collection and the characteristics of its storage, as well as the type of preservation medium, determine the different initial thickness of the cornea. Precision cutting of a transplant from a donor cornea for PAD requires the surgeon to have skills in working with various models of microkeratomes, takes a lot of time and is labor-intensive. Also worth mentioning is the factor of numerous additional manipulations, including the assembly of a microkeratome, installation of a donor cornea in an artificial anterior chamber, repeated ultrasound pachymetry of the cornea and a number of others.
In connection, the preparation of donor material began to be carried out in advance, in the conditions of specialized institutions involved in the collection and storage of donor tissue - eye tissue banks. This is the so-called “pre-cut” or “pre-cut” technology. The results of PAD operations performed using donor corneas prepared both by the surgeon during the operation and cut in the eye bank did not reveal significant differences in the incidence of complications and gave comparable clinical and functional results.
Currently, the ZAK technology is gaining increasing popularity, which involves the formation of an ultrathin graft (uZAG) with a minimum thickness of the residual stroma (no more than 130 μm), which makes it possible to obtain a significant increase in visual functions compared to the traditional ZAK technology.
However, depending on the location of the corneal graft on the surface of the patient’s eye, transplants (but not keratoplasties) are divided into corneal (central and peripheral, corneo-extracorneal (corneal-scleral) and scleral. Peripheral corneal and corneo-extracorneal transplants are called according to their functional purpose also barrier. ILC and PCC are only corneal, since the transplantation is carried out in a bed prepared within the patient’s cornea. In the interests of a better optical effect, the grafts are placed centrally.
Among layer-by-layer keratoplasties used for reconstructive purposes, there are overlay keratoplasties (epiceratoplasties), in which a layer-by-layer corneal graft is located on the de-epithelialized surface of the cornea without creating a bed within the optical zone.
Penetrating is a keratoplasty in which the entire thickness of the recipient's cornea is replaced with a graft. Depending on the size of the graft used, penetrating keratoplasty, as well as layer-by-layer keratoplasty, is divided into partial, subtotal and total. The ideal size for optical penetrating keratoplasty is a 7.5 mm centered graft.
With partial penetrating keratoplasty, irregular astigmatism often develops, which significantly reduces visual acuity even with perfectly transparent graft engraftment, and a large area of the native cornea (often genetically altered) remaining around the graft can contribute to the recurrence of the disease in the long term and make it impossible to wear a corrective contact lens. Large graft sizes during total penetrating keratoplasty lead to an increased risk of developing allergic-immunological reactions, anterior, sometimes even circular, synechiae, and a worse prognosis for retransplantation in case of clouding of the primary graft.
Layered-through-layer (usually mushroom-shaped) keratoplasty combines the qualities of both - the “mushroom cap” replaces the anterior or posterior layers of the cornea, and the “mushroom stem” makes the graft end-to-end. If the “mushroom cap” is facing anteriorly, such a “mushroom” is called anterior, but if the “mushroom cap” is facing posteriorly (towards the anterior chamber of the eye), then the “mushroom” is called posterior. Depending on the purpose of the operation, keratoplasty can be optical, therapeutic or cosmetic. The purpose of the former is obvious - their immediate goal is to restore (or improve) the transparency of the cornea and increase visual acuity. Therapeutic keratoplasty is resorted to when the disease progresses or damage to the cornea occurs in cases where conservative therapy is unsuccessful. Cosmetic surgeries are aimed at improving the appearance of the cornea and restoring (reconstructing) its congenital or acquired defects and deformations after injuries and diseases.
However, it must be recognized that such a division is conditional, since optical keratoplasty is very often used for eye diseases (for example, dystrophies), and also, ultimately, can have a therapeutic effect on surrounding tissues (the effect of clearing a cloudy cornea in the neighborhood with a transparently engrafted graft). In some cases, therapeutic keratoplasty can provide an optical effect over time. In addition, optical and therapeutic keratoplasty also help improve the appearance of the eye and the subject, restore the cornea after defects (ulcers, wounds), deformations (scars, ectasia, tumors, abscesses), that is, they lead to a cosmetic effect. In turn, cosmetic surgery can also contribute to the optical and therapeutic effect.
When determining the indications for a particular method of operation, it is always necessary to weigh the extent to which the degree of risk justifies the expected result of the intended intervention, the likelihood and severity of complications encountered with it. Layer-by-layer transplants are technically simpler and always involve less risk than end-to-end transplants. The exception is posterior lamellar keratoplasty, which is not only more labor-intensive, but also technically more difficult to perform.
Accurate localization of changes in the cornea in depth, as is known, is carried out using biomicroscopy, and currently the maximum amount of information with an accuracy of nanometers is provided by OCT of the cornea. Additional information that allows you to adjust the plan for the upcoming operation and predict its outcome is obtained using ultrasound echobiometry, electrophysiological studies, diaphanoscopy, and tonometry.
In its most general form, the basis for optical keratoplasty is pathological changes in the cornea, which, due to its persistent clouding, are accompanied by a significant decrease in vision, impairing the ability to work or self-care at home, with encouraging results of predictive tests for the preservation of visual reception. For keratoplasty with optical purposes, the through-and-through option is often chosen, since during a layer-by-layer operation it is not always possible to count on very high visual results (due to slight clouding that inevitably occurs at the boundary of the layers of your own and transplanted tissue). However, due to the much lower risk of layer-by-layer transplantation, compared to end-to-end transplantation, there are “optical indications” for the former, especially in cases of a single sighted eye.
Cloudy graft engraftment after the first operation does not exclude repeated optical keratoplasty or keratoprosthesis. In these cases, if the optical effect cannot be achieved, but the anatomical relationships of the cloudy cornea and neighboring tissues are improved (synechiae are eliminated, the sphericity of the cornea is improved, etc.), the first operation can be considered as a therapeutic-reconstructive one. In general, the indications for therapeutic keratoplasty can be formulated as follows. This operation is resorted to in case of pathological processes (plus - or minus - tissue) in the cornea that are not amenable to conservative treatment methods and, due to progression, threaten the death of the eye, decreased visual acuity, frequent relapses of the disease, manifested by debilitating corneal eye irritation syndrome, including pain.
Therapeutic keratoplasty as an urgent operation is indicated for fresh perforated wounds of the cornea with a tissue defect, for severe and especially severe burns of the eyeball (after necrectomy and in combination with so-called vascularizing operations).
Cosmetic keratoplasty combines two groups of operations aimed at both improving the appearance of the eye and reconstructing the cornea for congenital and acquired anomalies, defects and deformities. Currently, cosmetic operations of the first group, performed, as a rule, on blind eyes, and pursuing only one goal - improving appearance - are used extremely rarely, since the same can be achieved by using cosmetic contact lenses and thin-walled ocular prostheses. Keratoplasty operations of the second group, in turn, are divided into two subgroups: proper restorative (reconstructive) and refractive.
It is not by chance that refractive keratoplasty is singled out into a separate subgroup, since unlike all other keratoplasties, refractive keratoplasty is performed on the transparent, unchanged cornea of an eye that has a congenital or acquired refractive error. Among all cosmetic operations, refractive keratoplasty is the most widespread.
Operation prognosis
Available and expected visual functions.
Corneal opacity that occurs in early childhood and the associated amblyopia from disuse (ex anopsia), nystagmus or congenital strabismus are poor prognostic signs, although, of course, in these cases there are no absolute contraindications to surgery.
Considering that after keratoplasty, especially penetrating keratoplasty, vision, due to a number of complications, may not only not improve, but even worsen, this operation should not be performed for optical purposes if the visual acuity of the better eye is 0.1 or more. With such vision, it is sometimes possible to restore the ability to write and read without surgery, as well as with the help of telescopic or other correction. Therapeutic keratoplasty in some cases (with recurrent pterygium) is performed even with vision of 1.0.
If you have objective vision, it is important to get an idea of the field of view, since even with the most successful keratoplasty you can hardly count on its expansion. In the absence of object vision, one has to rely on the ability to perceive colors, the results of the Primrose test (with a Maddox stick), the results of entoptic and electrophysiological studies. With correct color perception, unmistakable recognition of the positions of the luminous strip formed when the eye is illuminated through the Maddox daddy (in the Primrose test), with the presence of a sensation of the figures of the vascular tree of the retina during autoophthalmoscopy (according to Purkinje), and finally, with normal thresholds of electrical sensitivity of the optic nerve (up to 6 V) and the high frequency of disappearance of electrical phosphene - after successful keratoplasty, you can count on fairly high central vision.
The absence of retinal detachment and the prospects for a good field of vision can be indicated by the positive phenomenon of diascleral transillumination and mechanophosphenes in all four quadrants of the eyeball under study.
A normal electroretinogram (with a b wave amplitude of at least 150 μV) also plays an important role. The presence of the correct form of the general (ganzfeld) electroretinogram (ERG) with a b wave amplitude of at least 2/5 of normal indicates the functional integrity of a part of the retina sufficient to obtain objective vision. In the absence of a general ERG, it is advisable to record a rhythmic electroretinogram (rERG, flicker) at a stimulus frequency of 30 Hz. If in this case the retina reproduces the rhythm of stimulation (even at small values of potential amplitudes), then we can talk about the preservation of part of the cone apparatus of the retina. In all cases, recording visual evoked potentials (VEP) is advisable. The absence of VEP will be an extremely unfavorable prognostic sign for postoperative visual functions.
The ability to project light correctly is very reassuring, as this can often rule out neuro-ophthalmic pathology, in particular optic atrophy. If there are significant violations of at least one of the above tests, although the indications for keratoplasty remain, the prognosis for improved vision becomes questionable.
State of ophthalmotonus.
Ocular hypertension and even glaucoma in eyes with cataracts can occur quite unnoticed, and therefore the possibility of their presence must be specifically excluded even before keratoplasty. The fact is that hydrodynamic disturbances existing in the eye can negate the results of even perfectly performed keratoplasty. In some cases, organic causes that cause periodic increases in ophthalmotonus can be easily eliminated during keratoplasty performed with the opening of the eye (dissection of synechiae, elimination of pupillary block, etc.). Naturally, this leaves no grounds for special antihypertensive interventions.
Another thing is that if the entire symptom complex of glaucoma has already formed, then even before keratoplasty (especially penetrating) it is necessary to perform one of the modern anti-glaucomatous operations: sinusotrabeculectomy with an open angle of the anterior chamber, basal valve iridencleisis with a closed angle, trepanocyclodialysis in case of aphakia, drainage with an explant of the anterior or posterior chambers of the eye, if the iris is greatly changed (for example, due to a burn), cyclocryopexy - with severe hyperproduction of chamber moisture. With the introduction of lasers into clinical practice, the possibility of antiglaucomatous surgery has increased. However, the production of laser irido- or goniopuncture for cataracts that do not allow the iris to be seen is, as a rule, very difficult.
The condition of a cataract or affected area of the cornea and adjacent tissues.
In optical keratoplasty, first of all, the etiology of the opacification and the possibility of its further development are extremely important.
If the clouding is stationary (thorn) and has no tendency to develop further, you can count on a good outcome. The most favorable are corneal opacities as a result of past inflammatory diseases and mechanical injuries, if they are not accompanied by abundant vascularization, the presence of anterior and posterior synechiae, and also if the cataract is quite limited in size and occupies the central zone. In this case, during the operation you can use a trephine with a diameter not exceeding the diameter of the cataract.
In prognostic terms, the least promising for optical keratoplasty are opacities that occur in the cornea after severe burns. In this case, the cornea usually suffers over its entire area; it is either very thin, or, conversely, excessively thickened, abundantly vascularized, devoid of sensitivity, its tissue has roughly degenerated into scar tissue.
Optical keratoplasty also has a favorable prognosis for familial hereditary corneal dystrophies, including keratoconus and other ectasia. This is explained by the slow (years and decades) course of the disease and damage predominantly to the central zone of the cornea. However, the corneal graft to be transplanted must be located within healthy tissue. The prognosis of the operation is significantly complicated if the clouding occurs due to secondary dystrophy, especially endothelial-epithelial dystrophy. In these cases, optical keratoplasty is indicated only in the terminal stage of the disease.
During therapeutic keratoplasty, in addition to the etiology of the disease (bacterial, viral, fungal, etc.) and the nature of the injury (physical or chemical), it is necessary to take into account the area and depth of damage to the cornea and, possibly, the sclera, the duration of the pathological process, the presence (depth) or absence of anterior chambers, its contents, the state of the iris, pupil, lens, vitreous body, ciliary body, vascular, retina. The presence of adhesions between the cornea and iris can significantly complicate the course and outcome of penetrating and posterior lamellar keratoplasty. As a rule, it is not possible to eliminate adhesions before surgery, but during keratoplasty they must be eliminated. In order to prevent repeated sealing of the iris to the cornea, it is advisable, taking into account the localization of synechiae, to perform a basal iridectomy.
It must be remembered that during therapeutic keratoplasty, the graft must be placed within healthy tissue, since only in this case can one count, first of all, on a therapeutic effect. Failure to comply with this extremely important rule will lead to relapse of the disease, death or degeneration of the transplanted graft.
Condition of the lens and vitreous body.
It is advisable to remove the cloudy lens during penetrating or posterior lamellar keratoplasty, which requires a trephine of sufficient size (in people over 40 years old, preferably at least 6 mm). If the lens is subluxated, it is necessary to perform its intracapsular extraction. If the lens is located in its usual place and the back part of its capsule is not damaged, it is advisable to limit ourselves to extracapsular extraction. Through the burr hole, not only the lens (or the excised part of the anterior capsule, the nucleus and the lens masses) is removed, but, if necessary, an intraocular posterior chamber lens is also implanted.
Initial opacities of the lens, naturally, are not grounds for its extraction. At the same time, it must be remembered that after keratoplasty, the opacities already present in the lens may noticeably increase.
It is customary to consider the state of aphakia as an unfavorable moment for penetrating keratoplasty. However, the point is not in aphakia itself, but in the presence of adhesions of the vitreous body to the cornea and, as a consequence, the development of secondary endothelial-epithelial dystrophy of the cornea. To improve the prognosis of keratoplasty, measures must be taken to free the anterior chamber from the vitreous strands soldered to the cornea.
Vitreocorneal fusion can also occur in the presence of a lens, if it is displaced from its place, and the vitreous body dislocated into the anterior chamber reaches an area of the cornea devoid of endothelium. The cloudy vitreous must also be removed. For perforating types of keratoplasty, vitrectomy is best performed during one operation using the “open palate” method. The presence of a transparent lens or at least only a transparent posterior capsule allows you to delay the operation for 3-6 months and, after improving the transparency of the cornea, perform vitrectomy in a closed way through the flat part of the ciliary body.
Condition of the eyelids, conjunctiva, tear-producing and tear-draining functions.
Incomplete closure of the eyelids due to their cicatricial insufficiency or paralytic lagophthalmos should alert the surgeon planning the operation. After keratoplasty, he may need to undergo blepharorrhaphy. Sometimes it is preferable to perform plastic surgery on the eyelids or conjunctiva. In case of partial ankylo- or symblepharon, keratoplasty is usually combined with plastic surgery on the conjunctiva and skin of the eyelids. If trichiasis is present, it must be eliminated before keratoplasty.
Keratoplasty can also be doomed to failure if tear formation is sharply delayed, therefore, in case of dry eye syndrome (Sjögren's syndrome), corneal transplantation should be preceded by other interventions aimed at restoring normal eye wettability (in case of insufficient function of the lacrimal glands - coagulation of lacrimal openings, in the complete absence tear production - transplantation of the outlet end of the common salivary duct into the conjunctival sac). To assess tear-forming function, the Schirmer test is used.
Impaired lacrimal drainage, manifested in complaints of lacrimation, is not an obstacle to keratoplasty. However, in these cases it is absolutely necessary to examine the contents of the conjunctival cavity for microflora. The presence of abundant growth of microorganisms on nutrient media will require sanitation of the lacrimal ducts (for chronic purulent dacryocystitis, surgery is necessary - dacryocystorhinostomy).
If the pathological process threatens the death of the eye, then therapeutic keratoplasty in such conditions can be performed even with purulent inflammation in the lacrimal sac, however, in this case, before transplantation it is necessary to ligate the lacrimal canaliculi and thoroughly sanitize the conjunctival cavity.
Acute inflammatory diseases of the conjunctiva and cornea are a contraindication for keratoplasty planned for optical purposes. However, in some cases, therapeutic keratoplasty can be a very effective method of treating severe inflammatory diseases of the cornea, limbus and conjunctiva that occur with ulceration, including purulent infection.
Transplant material
Corneal tissue used for corneal transplantation can be autologous, isogenic, allogeneic, or xenogeneic.
Autologous tissues (the recipient's own tissues) would be the most suitable for corneal transplantation, but they are rarely used in practical ophthalmology. The possibility of their use is limited to refractive keratoplasty (keratomileusis) and those emergency cases when the patient’s second eye was blind (terminal glaucoma, total multiple and unsuccessfully operated retinal detachment, atrophy or interruption of the optic nerve), but had a good cornea.
More often, autotransplantation for optical purposes is used within the same eye, when, with small central cataracts, there is transparent tissue on the periphery of the cornea. By rotating the eccentrically cut corneal disc or by interchanging the cloudy and transparent areas, the desired optical effect is achieved.
Isogenic tissues are tissues transplanted between identical twins. Being identical genetically and having the same set of antigens, they are completely compatible immunologically. However, the use of such tissues can only be of a casuistic nature, since the victims practically do not have twin brothers and sisters who can be donors.
Allogeneic for a person is the tissue of another person. For a long time, corneal transplantation remained an exclusive, episodic intervention, carried out immediately after the transplant was removed from a donor who died in an accident. However, this was clearly not enough due to the large number of patients awaiting keratoplasty. Ophthalmology was in urgent need of a more accessible donor, the development of various methods of corneal preservation, and the creation of a reserve of corneal material.
Academician is recognized throughout the world as the intellectual father of today's eye banks. V. P. Filatov (Odessa), who already in 1934 reported the possibility of taking eyes from a cadaver (several hours after death), followed by treating them with a solution of brilliant green and storing them at a temperature of 2-4 ° C in a closed glass vessel . This type of storage, carried out for up to 1-3 days in a humid chamber, remained the method of choice for several decades. The main goal of tissue preservation, as a way of preserving it for subsequent keratoplasty, is to inhibit the processes of autolysis and weaken the antigenic properties in the transplant material. The corneal preservation methods themselves must satisfy the following basic requirements: be simple and cheap, universal (suitable for all types of keratoplasty), and disrupt the vital functions of the corneal tissue as little as possible.
grafts dehydrated over silica gel continue to be used in our country and abroad . The simplicity of the method, long shelf life, which allows the accumulation of transplant material, and ease of transportation are attractive advantages for the use of such material for emergency indications. At the same time, dehydrated grafts are deprived of vital activity and, first of all, of the endothelial lining. There is no need to count on their true transparent engraftment. Therefore, after rehydration, this material can only be used for anterior lamellar keratoplasty in the partial and almost complete version, primarily not for optical, but for therapeutic purposes. If corneal perforation threatens or develops as a result of severe and especially severe eye burns, these grafts can be used as a biological bandage during vascularization operations.
The most promising method of long-term preservation of corneas for layer-by-layer and especially penetrating keratoplasty is low-temperature (-196°C) keeping them in liquid nitrogen using various cryoprotectants. Thus, the freezing of corneas with a border of sclera, placed in a 10% solution of polyethylene oxide cryoprotector of molecular weight 400, is carried out according to a two-stage program with a cooling rate at the 1st stage of 1-2 degrees / min before the start of crystallization and at the 2nd stage - 300-400 degrees /min up to -196°C. This program helps preserve the structural and functional properties of corneal tissue. The biological and optical results of keratoplasty obtained using grafts preserved in this way are in some cases not inferior to freshly preserved ones. Therefore, cryopreservation promises to be the only method of corneal preservation with an unlimited shelf life. However, the high cost of the technique and the resulting damage (albeit reversible) to endothelial cells prevent the widespread introduction of this preservation method into the clinic.
The only reliable, but expensive method that today allows corneas to be preserved for up to 35 days is storage in an organ culture medium under thermostatic conditions (t = 32-37°C), filled with 5% carbon dioxide to create buffer properties of the medium.
The advantages of such organ cultivation of donor corneas for up to 35 days are:
- constant availability of transplants from donors who died as a result of accidents;
- multiple sterility control;
- multiple assessment of the endothelium;
- post-mortem HLA typing.
Currently in Russia there is no (presumably temporarily) legislative framework prescribing rules for the collection of donor transplant material, including corneal material. Accordingly, there are no contraindications for collecting corneas. And they are very important both for the safety of bank staff and the patient, and for the correct choice of donor cornea and the outcome of keratoplasty. Therefore, it is better to familiarize yourself with the list of the most important “contraindications for the use of corneas” based on the existing one in Europe (adopted in January 1990 at the 3rd European Conference of Cornea Banks).
| Contraindications for the use of donor corneas (adopted by the European Conference on Cornea Banking, Leiden, 1990). | |
| Diseases that can put even cornea bank staff at risk |
|
| Diseases that may put the corneal transplant recipient at risk |
|
| Reasons excluding corneal donation due to poor quality |
|
The advanced age of the donor is not a criterion for excluding donation, but it is better to limit it to 65 years. Decisive, however, is the study of the quality of the endothelium. However, the age difference between the donor and recipient should not exceed 30 years. If possible, the donor's age should not be less than 2 years in order to avoid significant myopization of the recipient during penetrating keratoplasty. Of course, this does not matter for transplantation in infants or young children.
Where possible, an interval of 50 hours between circulatory arrest and enucleation should not be exceeded, although when storing the corpse in a refrigerator, postmortem storage times of up to 72 hours are compatible with successful organ culture.
Xenogeneic tissues are tissues obtained from animals. Being the most accessible, they were used at the first stage of the development of corneal transplantation. Interest in them disappeared, since all transplants from xenogeneic tissues either became cloudy or were rejected. The reason for this, generally accepted, lies in the immunobiological conflict (incompatibility) between the tissues of the donor and recipient. However, in recent years there has been renewed interest in them. Such a transplantation with a good outcome is possible by raising special universal donor animals that are genetically close to humans, preoperative effects on the immune system of the transplant, and drug correction of the immune response in the postoperative period.